-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2018; 8(1): 336-340
doi:10.5923/j.ajmms.20180811.08

Gender and Cardiovascular Risks in Awka, Nigeria
Ernest Ndukaife Anyabolu1, 2, Chinyelu Uchenna Ufoaroh3, Innocent Chukwuemeka Okoye1
1Department of Medicine, Chukwuemeka Odumegwu Ojukwu University, Awka, Nigeria
2Department of Medicine, Imo State University, Orlu, Nigeria
3Department of Medicine, Chukwuemeka Odumegwu Ojukwu University Teaching Hospital, Awka, Nigeria
Correspondence to: Ernest Ndukaife Anyabolu, Department of Medicine, Chukwuemeka Odumegwu Ojukwu University, Awka, Nigeria.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background and Objectives: Worldwide, cardiovascular risks are a recurring healthcare problem, spread across gender, in both the developed and the developing nations. Gender differences in cardiovascular risks have not been completely evaluated. This study sought to evaluate gender differences in cardiovascular risks in urban dwellers in Awka, Nigeria. Methodology: This was an unstructured, cross-sectional study conducted in Awka, Nigeria in 2017. Biodata and data on diabetes mellitus (DM) status, cigarette smoking, tobacco snuff use, hypertension (HTN) status, alcohol use, night-time sleep duration were obtained. The association between the variables and gender was determined. Results: The prevalence of smoking (Male=12.2%, Female=2.8% df=1, p=0.002)), tobacco snuff use (M=17.1%, F= 0.9%, df=1, p<0.001), alcohol use (M= 56.1%, F= 36.8%, df=1, p0.003), was higher in male than in female subjects. Short nighttime sleep duration (<4 hours) was more prevalent in females (6.6%) than in males (2.4%), df=2, p=0.002. The difference in the prevalence of DM status as well as HTN status between the male and female subjects (df=1, p=0.091 and df=1, p=0.294 respectively), was not significant. Conclusion: Smoking, tobacco snuff use and alcohol use, were cardiovascular risks with higher prevalence in males, whereas short night time sleep duration was more prevalent in females in this study.
Keywords: Gender, Cardiovascular risks, Smoking, Tobacco snuff, Alcohol, Diabetes mellitus, Short nighttime sleep duration, Hypertension, Awka, Nigeria
Cite this paper: Ernest Ndukaife Anyabolu, Chinyelu Uchenna Ufoaroh, Innocent Chukwuemeka Okoye, Gender and Cardiovascular Risks in Awka, Nigeria, American Journal of Medicine and Medical Sciences, Vol. 8 No. 1, 2018, pp. 336-340. doi: 10.5923/j.ajmms.20180811.08.
Article Outline
1. Introduction
- Cardiovascular risk is the probability of developing a cardiovascular disease (CVD) within a defined period of time, taking into account several risk factors at the same time established over six decades using the analytical epidemiology of CVD. This aims not at cure of CVDs but at prevention by means of life style modifications. [1]The prevalence of CVDs worldwide varies among racial and ethnic groups. Cardiovascular diseases are diseases affecting the heart or blood vessels. [2] Some of the cardiovascular risk factors include high blood pressure, smoking, diabetes, lack of exercise, obesity, high blood cholesterol, poor diet, and excessive alcohol intake, these risks can also worsen the existing CVDs. High blood pressure results in 13% of CVD deaths, while tobacco results in 9%, diabetes 6%, lack of exercise 6% and obesity 5%. [2] Victor Oguoma et al in a Nigerian study found impaired blood glucose in association with other traditional cardiovascular risk factors. [3]The incidence of CVD is known to be higher in men than in women of similar age. This gender difference is more pronounced at a younger age [4, 5] and is partly explained by protective effects of sex hormones. [6] On the other hand, female patients with coronary artery disease have been reported to be more likely to have a worse cardiovascular risk factor profile. [7, 8] EUROASPIRE III and IV studies demonstrated the presence of multiple cardiovascular risks higher in females than males. The gender difference in the prevalence of multiple cardiovascular risk factors was more prominent in elderly patients (≥70 years) and patients with a lower level of education. [8]There was a paucity of studies on gender-related cardiovascular risks in Nigeria. This prompted us to undertake this study to determine the gender differences in cardiovascular risks in urban dwellers in Awka, Nigeria, with a view to creating awareness and instituting appropriate preventive measures to stem down such risks among the subjects.
2. Materials and Methods
- This was an unstructured, cross-sectional study consisting of 294 subjects recruited from Eke Awka Main Market, in Awka, Southeast Nigeria. The population was heterogeneous, comprising of artisans, hawkers, clerical staff, and traders, among others. The study was approved by the management of the market. With the assistance of the leadership of the market, the subjects were informed of the study through a gong crier. Every subject that took part in the study gave informed consent, and the purpose of the study was communicated to them. With the aid of a questionnaire, which was pretested on those with different levels of cardiovascular risks, data were obtained. The factors which were addressed in the questionnaire were biodata, diabetes mellitus status, cigarette smoking, tobacco snuff use, hypertension status, alcohol use, nighttime sleep duration.Demographic and anthropometric data were collected. [9, 10, 11]The variables were graded into groups as follows:Smoking: 1) those who were smokers and 2) those who were non-smokersTobacco snuff use: 1) those who used tobacco snuff and 2) those who did notAlcohol: 1) those who have positive alcohol history and 2) those who have notNighttime sleep duration: A) >6 hours, B) 4 – 6 hours, C) <4 hoursDiabetes mellitus: 1) those known to be diabetic prior to the screening and 2) those whose diabetic status was not known prior to the study.Hypertension: 1) those that knew they were hypertensive prior to the study and 2) those whose hypertensive status was not known prior to the study.The influence of the variables on gender were compared between the groups for each variable. The potential cardiovascular risks factors for gender evaluated were diabetes mellitus, cigarette smoking, tobacco snuff use, alcohol use, night-time sleep duration, and hypertension status. [11]Data AnalysesThe data were analyzed using the Statistical Package for Social Sciences (SSPS Inc, Chicago, IL) version 17.0 statistical software. For continuous variables, mean values and standard deviations were calculated and the means compared using two sample t-test. Categorical variables were compared using the nonparametric tests Chi-square. The distribution and characterization of variables with gender were analyzed using cross tabulation. All tests were two-tailed with P < .05 taken as statistically significant. Definition of terms:DM status ‘yes’ those known to be diabetic prior to the screening.DM status ‘no’ those whose diabetic status was not known prior to the study.Hypertension status ‘yes’ those that knew they were hypertensive prior to the study.Hypertension status ‘no’ those whose hypertensive status was not known prior to the study.Counselling was given to those subjects who were found to have cardiovascular risks. They were advised to see clinicians in the hospitals.
3. Results
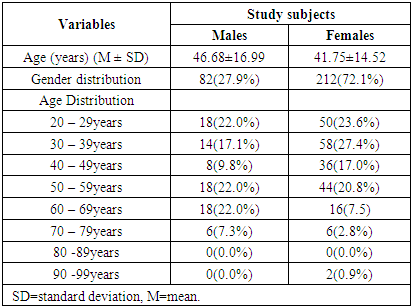
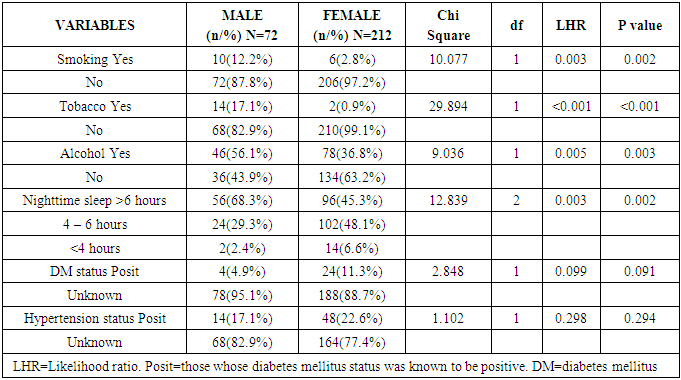
- The study subjects were 294. Out of this number, males were 82(27.9%) and females 212(72.1%). The mean age of the subjects was 43.13 ± 15.38, females 41.8 ± 14.5yrs and males 46.7±17.0yrs. There was no significant difference in age between the male and the female subjects, df=1, t=0.876, p=0.290. Majority (98.6%) of the subjects were Igbo.Among the 82 male subjects, 10(12.2%) were smokers, whereas only 6(2.8%) of the 212 female subjects were smokers. This showed that the prevalence of smoking of was significantly higher in males (12.2%) than in females (2.8%), df=1, p=0.002 (Table 2).Out of the 82 male subjects, 14(17.1%) were tobacco snuff users. In contrast, among the 212 female subjects, only 2(0.9%) used tobacco snuff, demonstrating that the prevalence of tobacco snuff use was significantly higher in males (17.1%) than in females (0.9%), df=1, p<0.001 (Table 2).Forty-six (56.1%) males out of the 82 have significant alcohol use, whereas 78(36.8%) of the 212 female subjects used alcohol. The prevalence of alcohol use was significantly high among males (56.1%) compared to females (36.8%), df=1, p=0.003 (Table 2).Only 2(2.4%) out of the 82 male subjects observed nighttime sleep duration <4 hours, whereas among the 212 females, 14(6.6%) observed a similar nighttime sleep pattern. This showed that the prevalence of low nighttime sleep duration (<4 hours) was significantly higher in females (6.6%) than in males (2.4%), df=2, p=0.002 (Table 2).Four (4.9%) of the 82 male subjects were observed to have a DM positive status, whereas 78(95.1%) did not know their status. On the contrary, 24(11.3%) of the 212 female subjects were found to have a DM positive status whereas in 188(88.7%) the status was unknown. However, this difference in the prevalence of DM status between the male and female subjects was not significant, df=1, p=0.091 (Table 2).Those who were observed to have a HTN positive status among the 82 male subjects were 14(17.1%), whereas 68(82.9%) had unknown status. Similarly, 48(22.6%) of the 212 female subjects were found to have HTN positive status whereas 164(77.4%) had unknown status. However, this difference in the prevalence of HTN status between the male and female subjects was not significant, df=1, p=0.294 (Table 2).
|
|
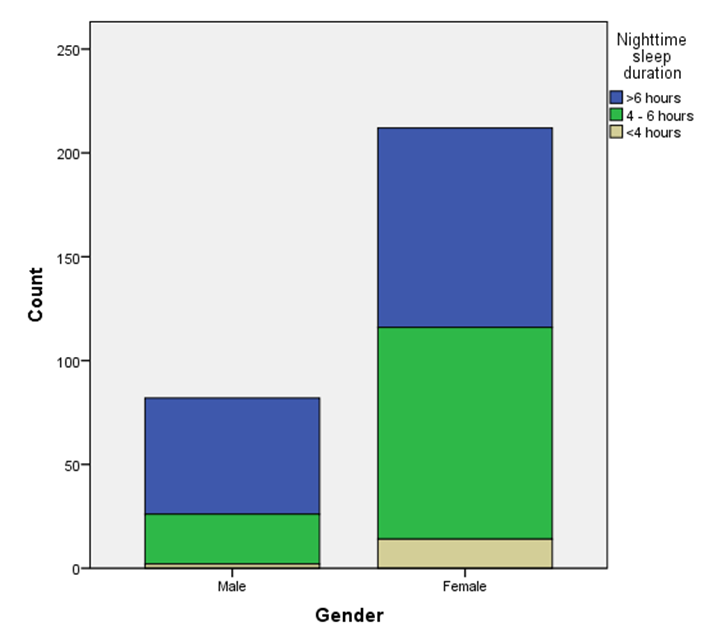 | Figure 1. Association between gender and nighttime sleep duration |
4. Discussion
- This study observed an association between gender and smoking. It further showed that the prevalence of smoking was significantly higher in males (12.2%) than in females (2.8%), p=0.002. In most developing countries more males smoke though there seems to be rising prevalence of female smokers. Often noted, the social stigma associated with female smoking might have also contributed to the fewer number of female subjects admitting to be smokers. This gap is almost closed in the developed countries. [12] This is similar to the study of Fred Pampel in sub-Saharan Africa which also showed higher prevalence of smoking and use of tobacco in males. [13] Smoking is often used as a means of stress reduction. [14] Male subjects are apparently exposed to high stress compared to their female counterpart in this part of the world. This might explain the higher prevalence of smoking in male subjects, as demonstrated in this study, with higher chance of developing CVD. Cardiovascular risks may result from the effects of smoking on the development of atherosclerotic changes with constriction of vascular lumen and inciting of a hypercoagulable state which may pave the way for acute thrombosis. [9, 15, 16] It was demonstrated in this study that the prevalence of tobacco snuff use was significantly higher in males (17.1%) than in females (0.9%), p<0.001. This agrees with the report of Fred Pampel et al which also found a higher prevalence of tobacco use in males than in females. [13] In this study, it was found that the prevalence of alcohol use was significantly high among males (56.1%) compared to females (36.8%), p=0.003. Alcohol is known to influence dyslipidemia and vascular changes which would cause peripheral resistance and predispose to hypertension, thus contributing to CVD. [9, 17] The higher prevalence of alcohol use in males, as found in this study, indicates that the contributory effects of alcohol to cardiovascular risks would be higher in males than in females. Male subjects at younger ages are more influenced by the environment and peers and as a result, are at higher risk of indulging in intake of significant amounts of alcohol. Poverty and lack of jobs for the youths and middle aged might also account for the higher prevalence of excessive alcohol use among males, with high propensity for developing CVDs like cardiomyopathy and hemorrhagic stroke. [18] Greater proportion of males were found to consume alcohol than females in this study and also at higher risk of cardiovascular events. A similar study by Richard W. Wilsnack et al [19] also documented a high prevalence of alcohol consumption in males compared to females, despite the differences in race and geographic locations of their subjects and ours.This study showed that the prevalence of short nighttime sleep duration (<4 hours) was significantly higher in females (6.6%) than in males (2.4%), p=0.002. Adequate sleep duration reduces the risk of CVDs. Estimated optimal sleep duration is 7 to 9 hours of night sleep. [20] In this study many of the study subjects especially the females had less than 6 hours’ duration of night sleep, thereby putting them at higher risk of CVDs. This might be explained by the fact that majority of the study subjects were less than 50 years, the age at which most women are caregivers e.g child rearing, caring for sick parents, grandchildren. A study by Naima Covassin et al [21] made a similar observation like our study and reported that more women had sleep deprivation and increased risk of hypertension, obesity and coronary artery diseases. Short nighttime sleep duration, if grossly inadequate, and devoid of restorative components, may generate stress and impart on onset of hypertension. High prevalence of hypertension among those engaged in nighttime duties has been documented in a large scale Korean study. [22] The difference in the prevalence of DM status between the male and female subjects observed in this study was not significant, p=0.091. Although the prevalence of these were higher in the female subjects, this observation might be as a result of other risk factors that put women at higher risk of CVDs, factors like poor sleep and obesity. However, these associations with female gender was not found to be significant in this study. [2]It was observed in this study that the difference in the prevalence of HTN status between the male and female subjects was not significant, p=0.294.A Nigerian study by Anyabolu et al found a significantly higher prevalence of hypertension in males compared to females. [9] Perhaps, this observed difference might be explained by the fact that the Anyabolu et al [9] study used measured blood pressure values in defining hypertension whereas this study used only hypertension status from the respondent’s responses to define the absence or presence of hypertension.Overall, this study has demonstrated that smoking, alcohol use, tobacco snuff use, and short duration of nighttime sleep were identifiable cardiovascular risks found in this study. Except for short nighttime sleep duration, the prevalence of the others was higher in male subjects compared to female subjects.
5. Conclusions
- Smoking, tobacco snuff use and alcohol use, were cardiovascular risks with higher prevalence in males than in females, whereas short nighttime sleep duration was more prevalent in females than in males in this study.
Limitations
- The study population was not structured. It was a cross-sectional study, in which many eligible subjects were missed out. The study population was small. A larger study size would have been more representative of the population.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML