A. J. Fayazov, V. U. Ubaydullaeva, D. B. Tulyaganov, T. A. Vervekina, U. R. Kamilov
Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Morphologic changes of rats’ internal organs at thermal-electric injuries based on the trial materials data have been described. The experimental animals were undergone electric current effect (220 Volt, duration – 3 seconds, direct current). The following internal organs have been taken for morphologic investigation: a cardiac muscle (left ventricle and interventricular septum), the lungs (central and peripheral parts), the pancreas (the head and the tail), the spleen (a portal area and parenchyma), the kidneys (the zone of cortical and medullary substance), the liver (central and peripheral parts), the brain (stem and hemispheres) in different periods after the burn. The development of pathologic processes was connected with circulation disorder, thermal and biochemical reactions which stipulated the reduce of oxidation process and were evidence of cells energy shortage with accumulation of acid products and denaturation of cytoplasm proteins.
Keywords:
Morphology, Electric injury, Thermal-electric lesions of rats’ internals, Experimental research
Cite this paper: A. J. Fayazov, V. U. Ubaydullaeva, D. B. Tulyaganov, T. A. Vervekina, U. R. Kamilov, The Impact of Electrical Injury to the Internal Organs of Laboratory Animals, American Journal of Medicine and Medical Sciences, Vol. 8 No. 0, 2018, pp. 259-266. doi: 10.5923/j.ajmms.20180810.02.
1. Introduction
The issue of electrical injury is multiform and complicated. It sets a lot of questions to the researchers and the most important one is providing emergency medicine to the victims – but it requires necessary knowledge about electrical injury pathogenesis. Electrical injury (EI) is characterized by the development of general and local pathologic changes in the organism due to the effect of the current [1]. Electricity renders thermal, electrochemical, mechanical and biological action to the organism [2, 3]. Thermal action occurs as the result of electrical energy transformation to the tissues resistance force. According to Joule law the greatest quantity of heat is discharged exactly in the tissues having a high resistance (skin) and the burns appear in the places of contact. Electrochemical changes lead to the blood corpuscle aggregation, proteins polarization, the change of ions balance in- and outside of cells. Mechanical action leads to the dissection and rupture of the tissues and to the bones fractures. Biological impact provokes the failure of heart conducting system function, nervous and endocrine systems disorders. The level of injury severity depends on many factors: current intensity, voltage, impact duration and others [5-9].
2. Goals
To conduct morphological research of experimental animals internals at the impact of the current in the trial.
3. Materials and Methods
The experimental research was carried out at the Republican Research Centre of Emergency Medicine (RRCEM) and the objects of investigation were 28 rats which were subjected to the current impact (220Volt). The impact duration made up 3 seconds. The following internal organs have been taken for morphologic investigation: a cardiac muscle (left ventricle and interventricular septum), the lungs (central and peripheral parts), pancreas (the head and the tail), spleen (a portal area and parenchyma), the kidneys (the zone of cortical and medullary substance), the liver (central and peripheral parts), brain (stem and hemispheres) in different periods after the burn. The received material was fixed in 10% neutral formalin solution (pН 7,2-7,4) and was poured into paraffin by Z.Loyda et al. [4]. Serial sections were made from the received blocks and were stained by hematoxylin and eosin (HE). Prepared histological material was placed to “ProgRes CT3” digital camera of “Axioskop 40” (ZEISS) for taking serial photography.
4. Results
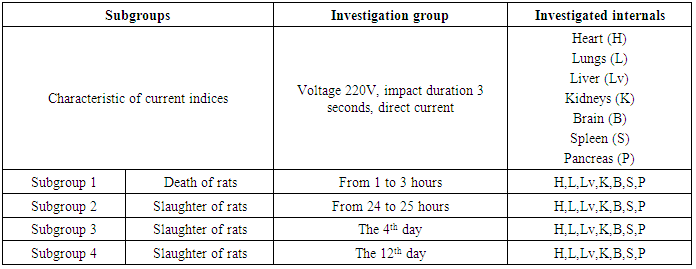
According to the terms of trial the rats were divided to the subgroups subject to the death time (table 1). Material sampling for histologic investigation was conducted in accordance with the plan and it allowed to reveal dynamic changes taking place in the internals. Table 1. Animals randomization subject to the death time
 |
| |
|
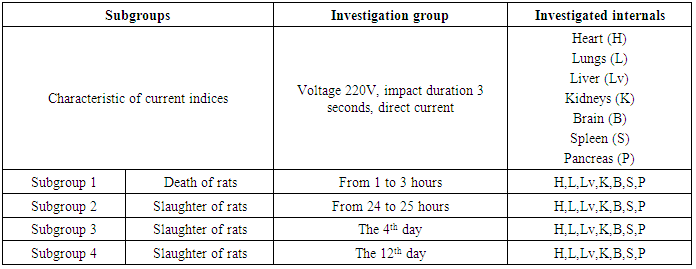
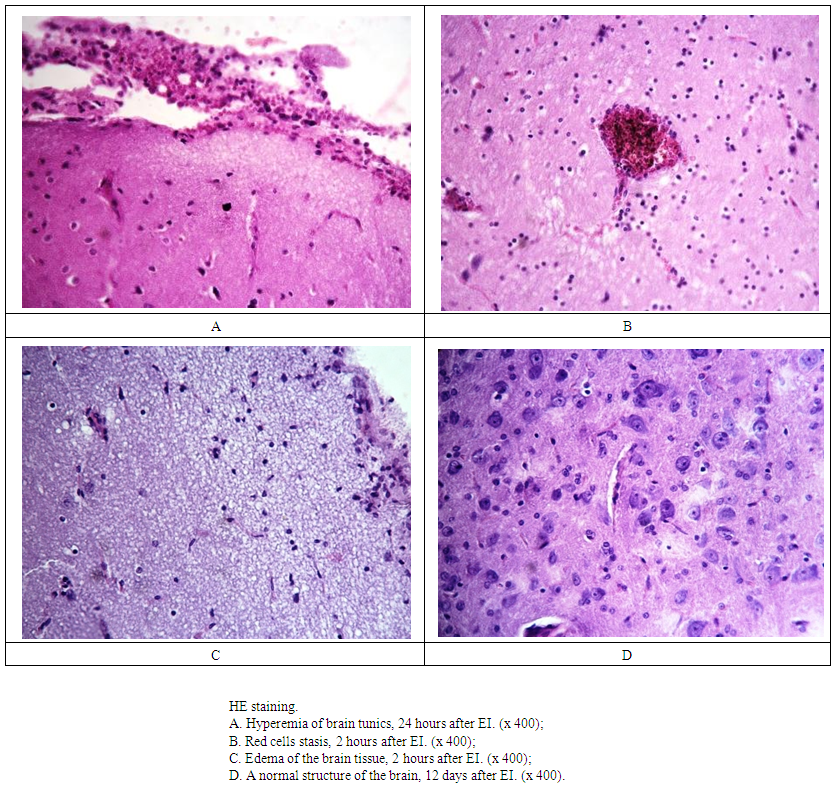
Within the first two hours after getting EI the edema began to develop in the brain tunics, the development of vessels hyperemia grew, there were extensive perivascular hemorrhages in some parts. The signs of edema were kept up to 4 days and then the pathologic process was diminished. Evident vessels hyperemia showed itself by the 1st day and histopathologic finding of hyperemia was more large-scaled in the tunics than in the brain tissue (Fig.1A). Lymphocytic infiltration had appeared round separate blood vessels by the 12th day of the investigation. There were not any gross violations in the red blood cells structure. There was an edema which grew from the first hours which was progressing and had revealed by the 1st day as a wide longitudinal stripe in the brain cortex adjacent directly to the soft brain tunics. There were also single perivascular hemorrhages in this area but the red blood cells structure kept safe. By the 4th day we had registered the beginning of edema regression which was moderate in the brain tissue. The edema was determined in some separate areas and looked as narrow light line by the 12th day of investigation. There were fixed the signs of perivascular and pericellular spaces dilatation in the subcortical parts of the brain. The vessels of microcirculation channel were marked out in histological sections by the lumen dilatation and hyperemia, the red blood cells stasis was observed in the lumen of separate vessels (Fig.1B). This pattern had been stable by the first day and regressed by the 4th day of investigation. Pathologic changes had focal character to the 12th day. The structure of cerebral cavity vascular plexus was kept and there were no pathologic changes neither in initial stage nor in the dynamics. Two hours after performing EI vessels lumen dilatation and their hyperemia with perivascular hemorrhages appeared in the brainstem vessels of microcirculation channel. There was an edema of brain tissue in the subshell area passing in the form of wide longitudinal stripe. We observed dilatation of perivascular and pericellular spaces in the brain tissue. The edema in the brainstem was more evident in compare with histological pattern of hemispheres (Fig.1C). The same pattern was observed 24 hours later. There was pointed a presence of focal hemorrhages in the brain tissue around which small sites of necrotic tissue were appeared. The phenomena of hyperemia, edema of tunics, cortical areas of subshell space, brain subcortical parts substance were kept safe. Pathologic processes had regressed by the 12th day (Fig.1D).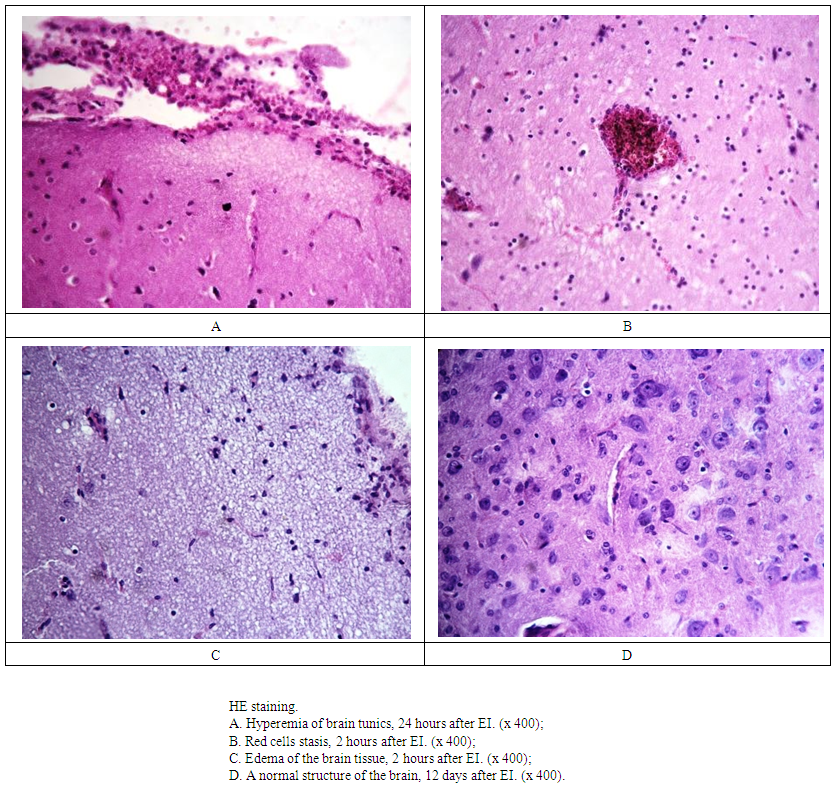 | Figure 1. The dynamics of pathologic processes in the brain at EI |
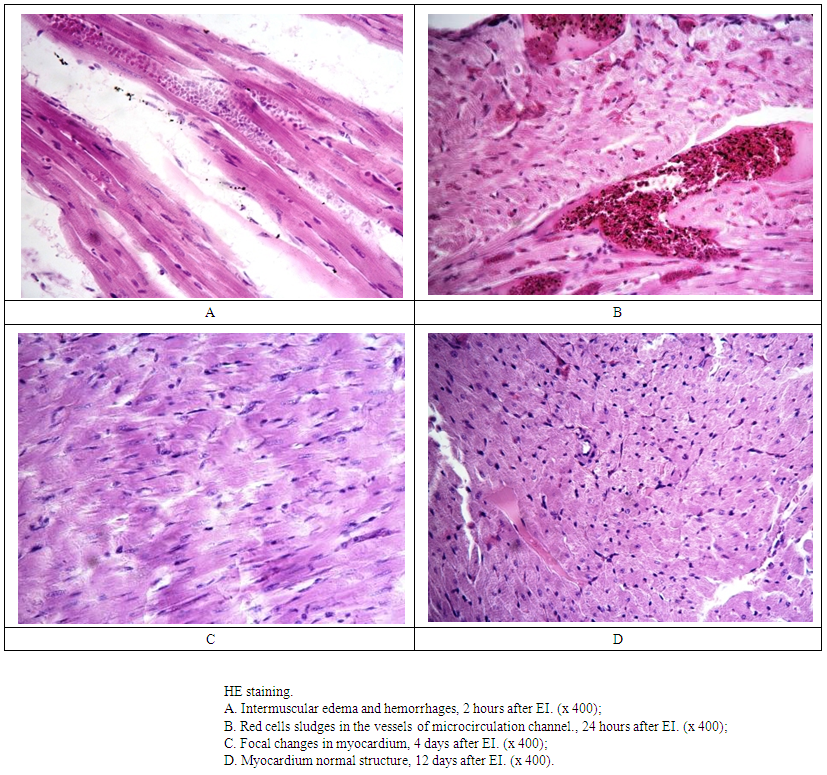
Within 2 hours after EI there was pointed the increase of stromal edema which was spread to bigger area and reached its maximum by 24 hours in cardiac muscle. Intermuscular edema was manifested unevenly on the whole area of investigated tissue with a tendency to its reduction in the 4th day. The same pattern was kept in the 12th day. By 2 hours from EI starting the structure of cardiac hystiocyte was kept, the signs of fragmentation and contractile degeneration were revealed only in separate areas, this process dominated from the side of interventricular septum. There were both focal and extensive confluent hemorrhages in the intermuscular space by the first day of investigation (Fig.2А). Small areas of tissue with the death of myocytes and with occurrence of singular leukocytes along periphery appeared in the zones of fragmentation and contractile degeneration. On the 4th day after EI the structure of myocytes was mainly kept, but in some parts of investigated tissue we observed small zones of myocardium with the signs of cardiac hystiocytes fragmentation (Fig.2С). Only some separate cardiac hystiocytes had the signs of dystrophic changes by the 12th day of the reserach. Two hours after the experiment starting the vessels of microcirculation channel looked dilated and plethoric. There was a stasis of red cells in the vessels lumen, a part of red blood cells had the signs of membrane destruction with sludges formation (Fig.2В). Hemorrhages of different sizes were formed in the perivascular and intermuscular spaces. Morphologic pattern did not significantly change within the first day but by the 4th and the 12th day it was pointed only selective hyperemia of vessels with red cells stasis in the lumen of separate ones. The changes in the cardiac muscle of the left ventricle and interventricular septum had practically equivalent character and manifested by stromal edema of tissue, changes in microcirculation channel and cardiac hystiocytes changes. The exception was in the area of injured tissue which was bigger in the interventricular septum than in the left ventricle muscle. Small foci of cardiac hystiocytes loss were dominated in the interventricular septum by 24 hours and at the same time dystrophic changes dominated in the left ventricle myocytes. Stabilizing of pathologic processes was pointed by the 4th and 12th days and they were focal dystrophic changes (Fig.2. D).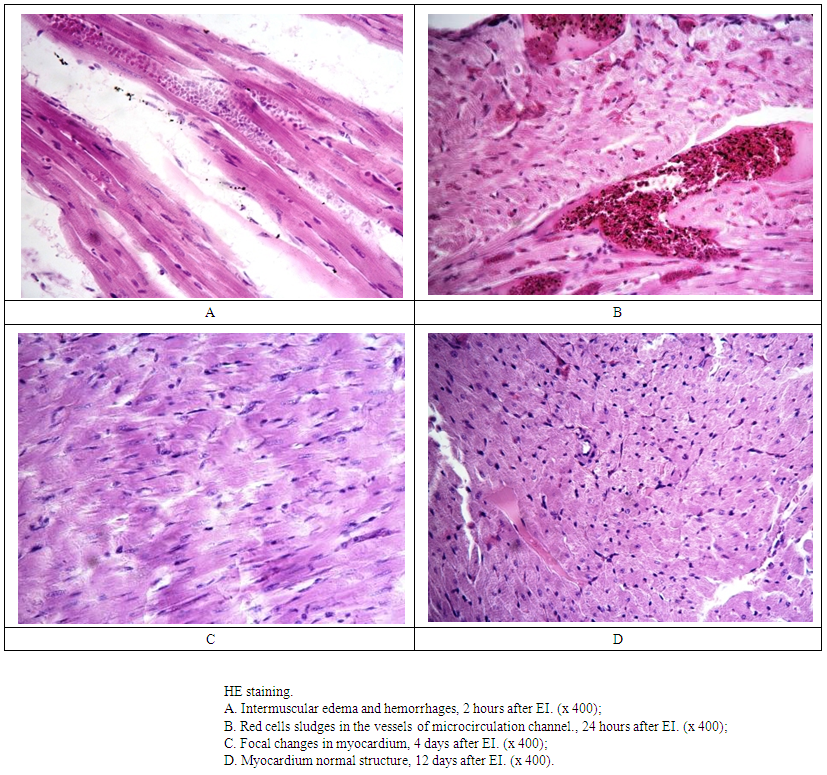 | Figure 2. The dynamics of pathologic processes in the heart at EI |
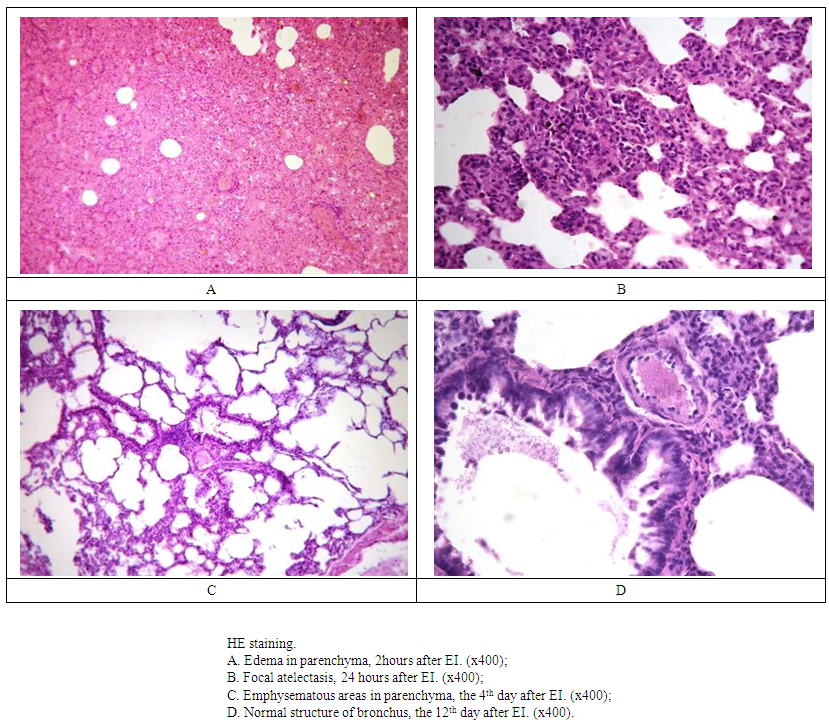
In the lungs parenchyma 2 hours after getting EI there was observed a hydropic fluid accumulation in the interstitial tissue of the lungs and around the vessels (Fig. 3А). Lumen dilatation and vessels hyperemia was observed not only in intersticium but in the alveolus wall which caused the development of alveolar septum thickness. In the lumen of alveolus bigger part (up to 90% of the whole investigated tissue) there was determined an exudate of hydropic fluid and diapedesis of red blood cells. The rest part of alveolus was compensatory undergone emphysematous dilatation. The edema reduced 24 hours after EI and the foci of distelectasis were observed in the tissue (Fig.3В). A morphologic pattern had approached to the norm by the 4th day except those parts of pulmonary tissue where bronchial obstruction by mucous mass led to the development of focal distelectasis (Fig.3С). The main part of investigated tissue had a normal morphologic structure by the 12th day – the alveolus were filled by air, the walls of alveolar septum were thin, the vessels were selectively plethoric. There were no rough pathologic failures connected with bronhial tree from the first hours up to the 12th day (Fig.3D). Bronhial tree structure was not disturbed, bronchi lumen was moderately dilated, mucous membrane was presented by epithelium of cylinder type and in separate bronchi we observed desquamation of mucous membrane cells to the lumen. We revealed reactive changes manifested by light wide foci in the medullary substance of lymphatic follicles in the lymphoid tissue associated with bronchi.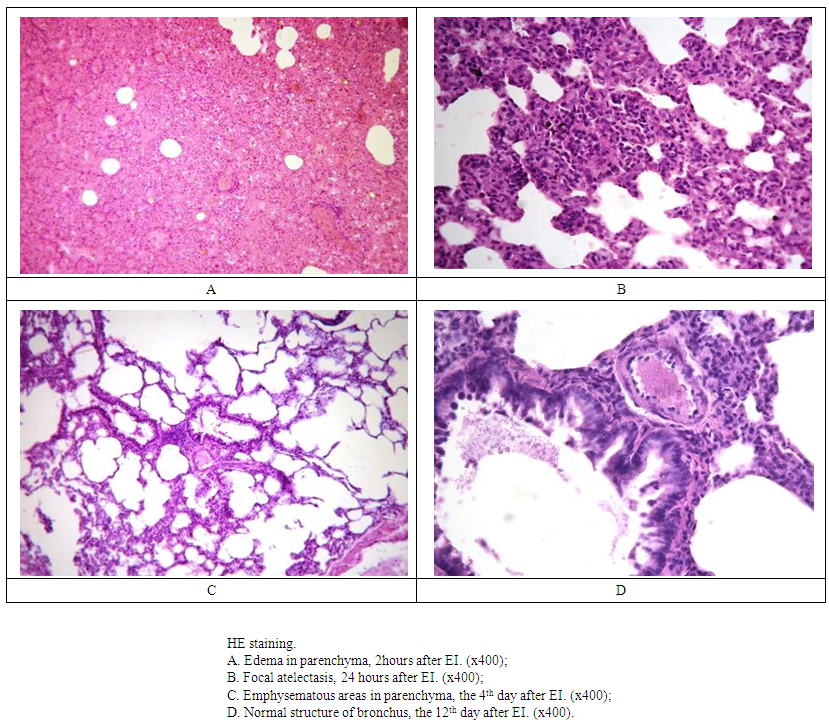 | Figure 3. The dynamics of pathologic processes in the lungs at EI |
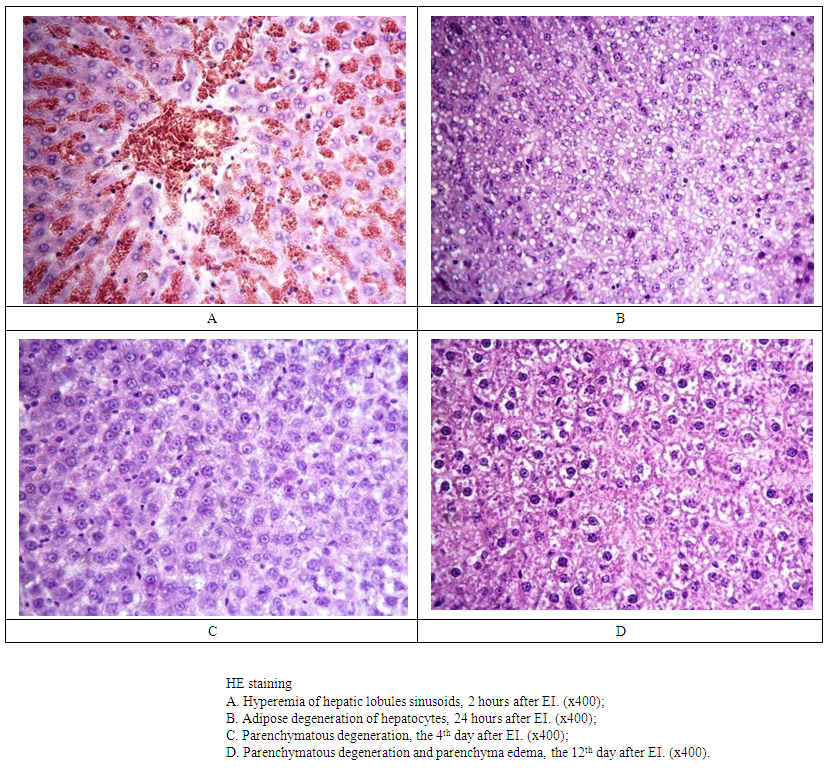
Two hours after current effect we observed paretic dilatation and evident hyperemia of the vessels in the wide areas of pulmonary tissue. Perivascular and big confluent hemorrhages were pointed in the lungs parenchyma. By the end of the first day arterioles and venules were plethoric and bigger vessels had a selective hyperemia. This pattern gradually regressed on the 4th and 12th days. ПриAt studying pulmonary tissue we did not find significant morphologic differences between the right and the left lungs.In central parts of the hepatic tissue 2 hours after EI a big quantity of seeds having protein nature appeared in hepatocytes cytoplasm - this process was predominately developed in the lobules central parts. We observed hyperemia, aggregation and sludge formation in the sinusoids, central veins and in the interlobular area (Fig. 4А). By the end of the 1st day a parenchymatous degeneration was evident not only in the central but also in the peripheral parts of the hepatic lobules and in some separate cases of investigation we pointed not only the pattern of parenchymatous degeneration but adipose degeneration too (Fig.4В). Parenchymatous degeneration of hepatocytes was observed in the central parts of the hepatic lobules mainly round central veins (Fig.4С) and in majority of cases the same pattern was pointed on the 12th day. But in some isolated cases by the 12th day of investigation the pattern of parenchymatous degeneration and parenchyma edema was evident in the liver (Fig.4.D). The hepatic lobules structure in the peripheral parts of the liver was kept during the whole experiment. The morphologic pattern in the central and peripheral parts of the lobules was the same by the end of the first day. We pointed the increase of parenchymatous degeneration signs in the peripheral part which were more evident than in the central part by the 4th day. There was no significant difference between morphologic pattern of the central and peripheral parts by the 12th day of investigation, except an evident hyperemia of the vessels in the peripheral parts of the liver.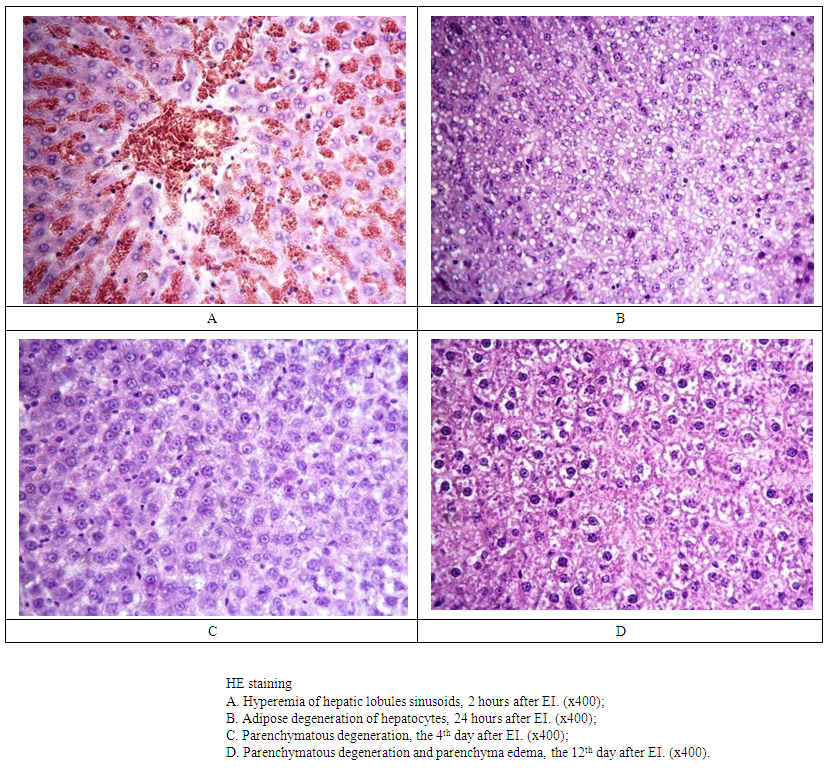 | Figure 4. The dynamics of pathologic processes in the liver at EI |
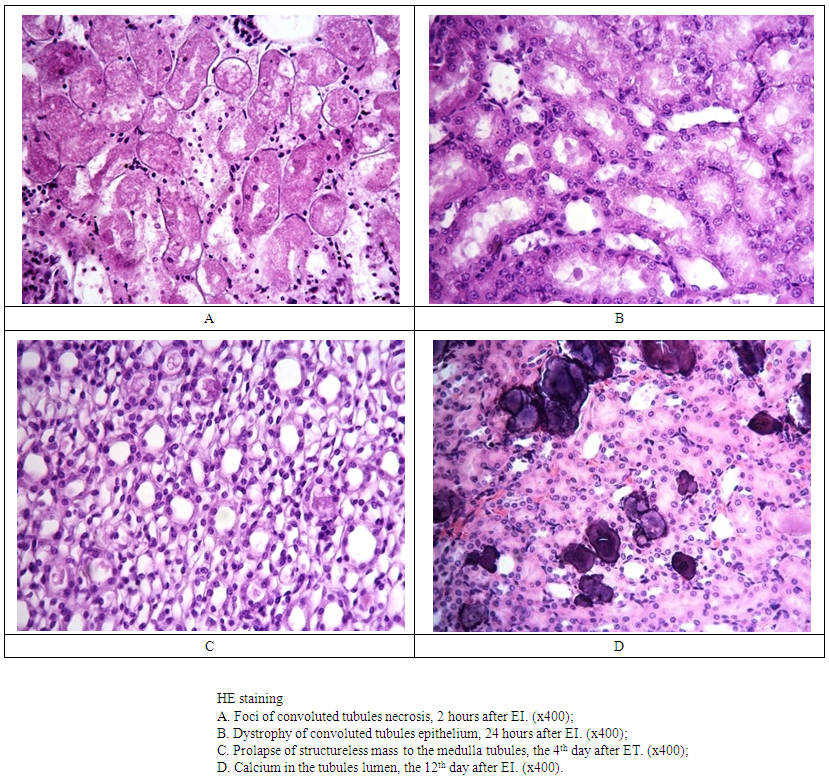
Within first 2 hours after EI in 50% of glomerules there were the signs of capillary dilatation in the renal parenchyma with red blood cells stasis in their lumen. Such changes in the glomerules were not long and had disappeared by the first day of the research. Beginning from 2 hours after experiment starting in the cortical zone of the kidneys, in the lumen of convoluted tubules we pointed an occurrence of dystrophic processes – the signs of epithelium swelling and appearance of seeds in the cytoplasm. The signs of parenchymatous degeneration were progressing and were kept up to the first day of investigation (Fig.5В). The formation of convoluted tubules necrosis was focal and did not have a mass spread (Fig.5А). Parenchymatous degenerations had decreased by the 4th day of the research and such histologic pattern was revealed only in some isolated parts and had a focal nature, though the signs of edema were kept. Epithelium became light, the signs of its desquamation to the tubules lumen were observed – this pattern was kept up to the 12th day of the experiment. From the time of getting EI in the kidneys tubules epithelium (proximal, straight, ascending distal, discharging tubules) situated in the medullary substance there were fixed the signs of parenchymatous degeneration. In the lumen of some of them there were formed erythrocytic sludges which were closing the tubules lumen. By the end of the first day of the experiment in the tubules lumen of kidneys medullary substance we were able to distinguish a focal prolapse of amorphous, hyaloid, structureless mass which continued to be distinguished on the 4th day of the research (Fig.5С). On the 12th day in the lumen of kidney excretory tubules we detected calcium salts (dense dark-blue formations) which were situated focally (Fig.5.D). The structure of cup-pelvic system during the whole investigation did not changes, only on the first day of the experiment we pointed hemorrhages to the adipose tissue.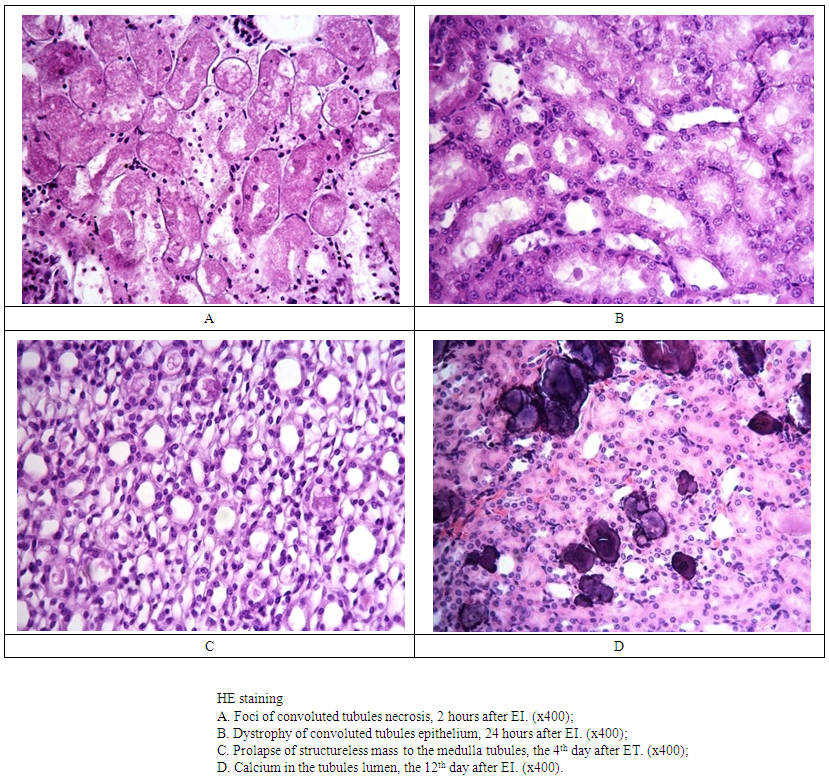 | Figure 5. The dynamics of pathologic processes in the kidneys at EI |
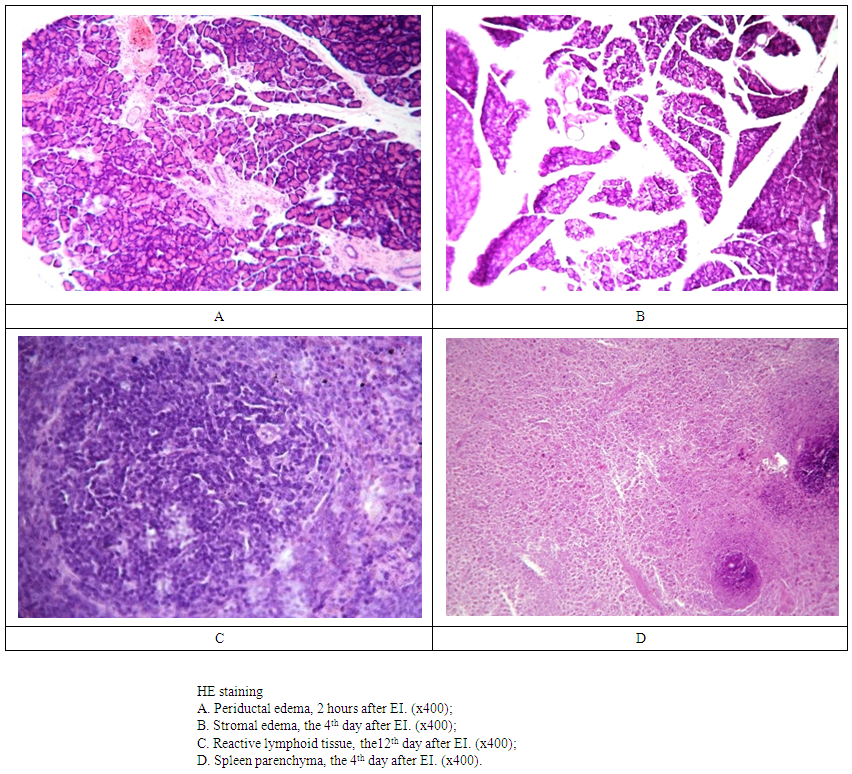
At different periods of the experiment in the kidney tissue parenchyma we fixed the signs of stable hyperemia of microcirculation channel vessels, arteries and veins. There were observed perivascular hemorrhages of the isolated areas and there was a cluster of lympho-and plasmocytes round some isolated vessels.After two hours and to the end of the first day after the effect of current we observed the signs of stromal edema in the pancreas tissue with a dilatation of interlobular spaces (Fig.6А,В). There were the signs of dilatation and hyperemia of blood vessels in the investigated areas. To the 4th day of the research, besides above mentioned changes, we revealed a focal dystrophy of parenchimatous cells. This pattern had regressed by the 12th day of the experiment. Morphologic structure of spleen tissue taken from portal area and marginal zone did not differ from each other. At all periods of investigation we pointed the hyperemia of sinusoids, focal hemorrhages in the stroma, reactive changes of lymphoid tissue follicles (Fig.6 С, D).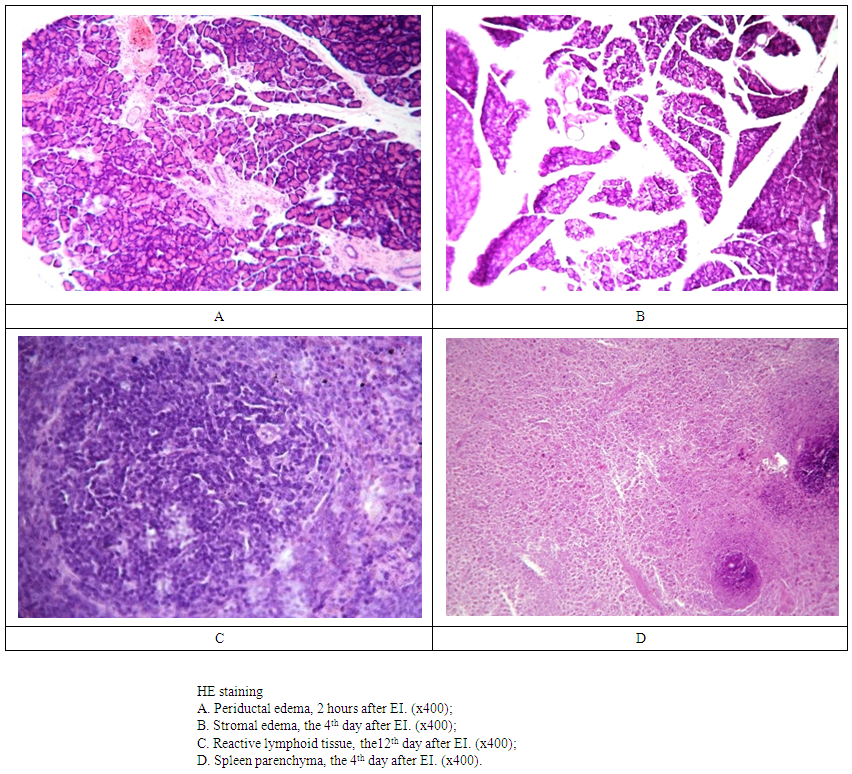 | Figure 6. The dynamics of pathologic processes in the pancreas and spleen at EI |
5. Conclusions
At the impact of current (220Volt) the development of pathologic processes in the rats was manifested by: stromal and cellular edema, dystrophic changes in the cells, focal necrotic changes. Those processes were reversible; they began to be evident 2 hours after electric injury with augmenting of the process to the first day, stabilization and limitation of spread to the 4th day and with regress to the 12th day of the experiment. The reaction of the blood cells and vascular channel to the impact of the current was manifested by hyperemia, stasis development sludge syndrome. Hereby, the development of pathologic processes was connected with circulation failure, thermal and biochemical reactions which stipulated the decrease of oxidation process intensity, testified to the cells energy shortage with accumulation of acid products and denaturation of cytoplasm proteins.
References
| [1] | Koumbourlis, A. C. Electrical injuries / A. C. Koumbourlis // Crit Care Med. –2002. – Vol. 30, № 11. – P. 424–430. |
| [2] | Stewart C. 2001. Electrical injuries. Pediatr Emerg Med Rep 6:1–10. Wright RK. 2001. Electrical injuries. eMedicine 2: 1–13. |
| [3] | Fish RM. 2004. Electrical injuries. In Emergency medicine: a comprehensive study guide, pp. 1231–1235. Ed JE Tintinalli, GD Kelen, JS Stapczynski. New York: McGraw-Hill. |
| [4] | Z. Loyda, R. Grossrau, T. Shibler. Histochemistry of ferments. - М. Mir.- 1982.- p.270. |
| [5] | Vecherkin V.A., Koralev P.V., Neyno N.D. The features of high-voltage electric injury in school-aged children. //Children’s surgery. – 2007.- №1. p.28-31. |
| [6] | Yakovlev S.V., Korostelev M. Yu., Antonov S.I., Bondarenko O.O. The experience of the use of external fixation devices in the treatment of patients with severe electric injury.// Medical science and education of Ural.– 2009.-№1. p.122-125. |
| [7] | Gupta BP, Mehta RA, Tragedia MM. Profile of deaths due to electrocution: a retrospective study. J Indian Acad Forensic Med. 2012; 34(1): 13–5. |
| [8] | Hussmann J., Kucan JO., Russell RC, et al. Electrical injuries – morbidity, outcome and treatment rationale. Burns. 1995; 21(7): 530–5. |
| [9] | Jensen PJ, Thomsen PE, Bagger JP, Nørgaard A, Baandrup U. Electrical injury causing ventricular arrhythmias. Br Heart J. 1987; 57(3): 279–83. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML