Kamilova U. K., Rasulova Z. D., Ibabekova Sh. R., Masharipova D. R., Nuritdinov N. N., Utemuratov B. B.
Specialized Scientific-Practical Medical Center of Therapy and Medical Rehabilitation, Tashkent, Uzbekistan
Correspondence to: Rasulova Z. D., Specialized Scientific-Practical Medical Center of Therapy and Medical Rehabilitation, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Background: To study the effect of lisinopril and losartan on the diastolic function of the left ventricle in patients with chronic heart failure (CHF), depending on the degree of renal dysfunction (RD). Materials and methods: A total of 223 patients with I-III FC of CHF were examined, initially and after 6 months. The first group consisted of 118 patients taking lisinopril as part of standard therapy; the second group - 105 - losartan. All patients were distributed depending on the estimated of the glomerular filtration rate (eGFR): 30 < eGFR ≤60 - 67 patients and eGFR > 60 ml / min / 1,73m2 -156 patients. Results: The analysis of baseline diastolic function in patients with CHF revealed diastolic dysfunction in 81,8% of patients with CHF, with a predominance of delayed relaxation in 59,3% of patients and an increase in the number of patients with a restrictive type of diastolic dysfunction in patients with III FC of CHF. The dependence between the parameters of the diastolic function - the rate of E and eGFR was revealed. Patients of the first and second groups with I-III FC of CHF after 6 months of treatment had an improvement in diastolic left ventricle function with advantage in patients in the group of losartan with I and III FC of CHF. On the background of treatment in patients with CHF with eGFR≤60 ml/min/1,73 m2 there was a significant increase in the rate of E in both groups of patients without statistically significant differences. Conclusion: Patients of the first and second groups with I-III FC of CHF after 6 months of treatment had an improvement in diastolic function left ventricle.
Keywords:
Chronic heart failure, Diastolic dysfunction of the left ventricle, Renal dysfunction
Cite this paper: Kamilova U. K., Rasulova Z. D., Ibabekova Sh. R., Masharipova D. R., Nuritdinov N. N., Utemuratov B. B., Diastolic Function of the Left Ventricle Depending on the Degree of Renal Dysfunction in the Background of Treatment, American Journal of Medicine and Medical Sciences, Vol. 8 No. 9, 2018, pp. 241-245. doi: 10.5923/j.ajmms.20180809.05.
1. Introduction
The attention of scientists has long been drawn to the connection of cardiac and renal pathology. Reduction of the glomerular filtration rate (GFR) is a prognostically unfavorable factor in chronic heart failure (CHF), while heart failure can lead to a decrease in kidney function or aggravate existing disorders [3]. According to the data of a number of authors, the change in the structural and morphological parameters of the myocardium of the left ventricle (LV) depends on the functional class (FC) of CHF and renal dysfunction manifested by an increase in the final systolic and final diastolic dimensions and volumes of the heart [2]. With the increase in renal dysfunction (RD), size decreases, the most significant changes occur in the left ventricular mass index (LVMI), increased left ventricular dilatation and increased eccentric hypertrophy of the myocardium, and aggravated by the development of CHF symptoms. Eccentric hypertrophy was associated with a higher level of creatinine compared with patients with normal geometry [4]. In recent years the results of studies have shown that aimed at improving and maintenance of renal function therapy can improve the forecast in patients with CHF [1, 5, 6] comparative studies of various drugs from the groups recommended for the treatment of patients with CHF, taking into account the kidney function for this category of patients has not previously been conducted and is an urgent task.The results of numerous studies (SAVE, SOLVD, CONSENSUS, SMILE) demonstrated the ability of ACE inhibition to reduce the risk of death, cardiovascular complications, morbidity, improve clinical symptoms, slow the progression of CHF, and improve the prognosis of the disease. The nephroprotective properties of ACE inhibitors are due to a decrease in increased intraluminal pressure and an antiproteinuric effect, which, according to clinical studies, is realized in preventing and slowing down the rates of glomerular filtration rate decline and the development of terminal renal failure [1, 3, 6].The nephroprotective properties of losartan have been demonstrated in large randomized trials of RENAAL, ELITE II, HEAAL in terms of their ability to prevent irreversible impairment of renal function, a positive effect on overall mortality, prognosis, risk of sudden death and severe complications of CHF [9, 15].According to the ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure, the high risk of further impairment of renal function in CHF causes monitoring of renal function and dose of drugs in the administration of ACE inhibitors and ARA [11].The aim of this study is to study the relationship between the indices of left ventricular diastolic function and GFR and to evaluate the efficacy of lisinopril and losartan in the left ventricular dysfunction, depending on the degree of CHF and RD.
2. Material and Methods
A total of 223 patients with ischemic heart disease (IHD) with I-III FC of CHF were examined (the mean age of patients was 62,3±5,6 years), initially and after 6 months of treatment. The first group (I) consisted of 118 patients with I FC (28), II FC (51) and III FC of CHF (39 patients) were treated with standard therapy - lisinopril; the second group (II) -105 patients with I FC (22), II FC (49) and III FC of CHF (34 patients), taking for 6 months against the standard therapy – losartan, (the average dose of lisinopril was 7,8±2,6 mg per day, losartan – 76,3±25,6 mg per day). Patients in the complex of therapy included: statins, antiaggregants, bisoprolol, spironolactone 25 mg per day, loop diuretics according to indications. All patients underwent echocardiography (EchoCG) with dopplerography, determination of serum creatinine (Cr), and the glomerular filtration rate (eGFR) was calculated using the MDRD formula [15]. Echocardiography was performed with an assessment of the diastolic function of the LV with an estimate of the maximum early filling rate of the LV (E), the maximum late atrial filling rate (A), the E / A ratio, and the elongation of isovolytic LV relaxation (IVRT) [14].Also, all patients were divided into 2 groups depending on the estimated glomerular filtration rate (eGFR): 302 – 67 patients (29 in the I group, 38 patients in the II group) that correspond Stage 3 chronic kidney disease (CKD), and eGFR>60 ml/min/1,73 m2 – 156 patients (89 patients in I group, 67 in II group).Statistical method of data processing. For statistical data processing, the Microsoft Office Excel 2013 software package was used, including the use of the built-in statistical processing functions with the STATISTICA-6.0 program. The methods of variation parametric and nonparametric statistics were used to calculate the mean arithmetic mean of the studied index (M), the standard deviation (SD), the standard error of the mean (m), relative values (frequency, %), the statistical significance of the measurements obtained by comparing the mean values was determined by the criterion Student (t) with calculation of probability of error (p) for checking the normality of the distribution (by the kurtosis criterion) and the equality of general variances (F-Fisher test). For statistically significant changes, a confidence level of p<0,05 was adopted. To study the relationship between quantitative variables, the correlation analysis was used to calculate the Pearson linear correlation coefficient.
3. Results
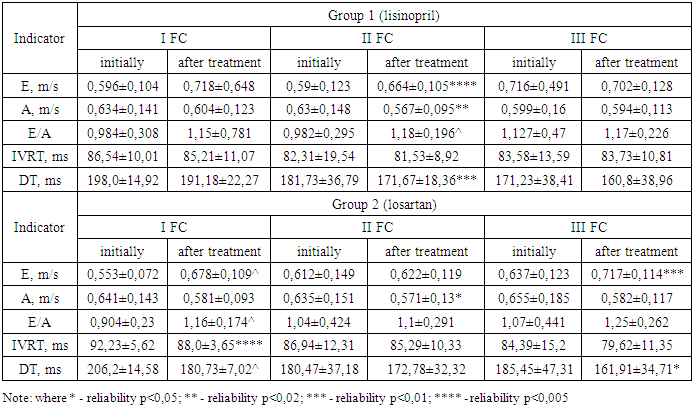
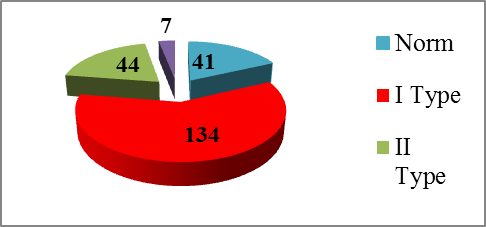
Analysis of the initial diastolic function in patients with CHF revealed diastolic dysfunction in 81.8% of patients with CHF with a decrease in E, an increase in A (p<0,05), deviation from the norm of the E/A ratio, an increase in IVRT (p<0,05) in compared with the indicators of the control group. Disturbances of diastolic function were initially determined in 81,8% (185 patients) of patients of both groups. In this case, type I (delayed relaxation) was recorded in 59,3% (134 patients), type II (pseudonormal) in 19,5% (44), type III (restrictive) in 3,1% (7) patients (Fig. 1).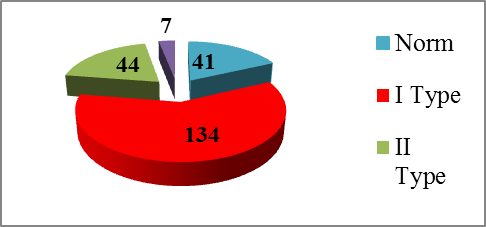 | Figure 1. Analysis of diastolic LV disturbances in patients with CHF (type I – delayed relaxation, type II - pseudonormal and type III - restrictive) |
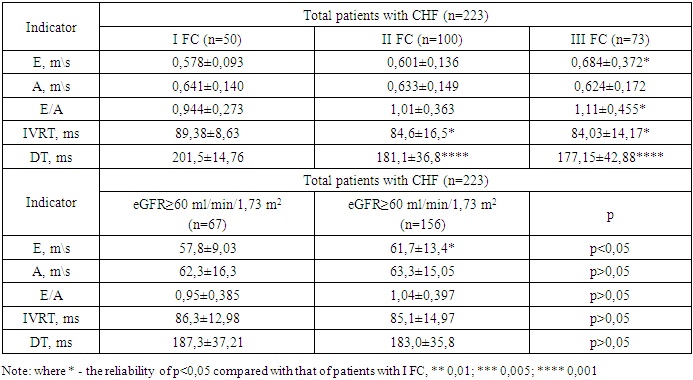
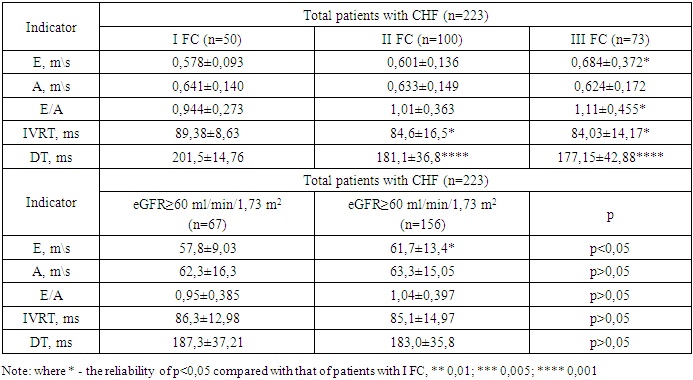
The initial indices of LV diastolic function in patients with I-III FC of CHF in both groups are presented in Table 1. The maximum early filling rate of E LV from I, II, III FC was 0,578±0,093; 0,601±0,136 and 0,684±0.,372 m/s, respectively with a significant increase in patients with III FC of CHF by 15,5% (p<0,05) compared with the I FC CHF; the time of isovolymetric relaxation of the LV – IVRT was 89,38±8,63; 84,6±16,5 and 84,03±14,17 ms with a significant decrease in patients with II and III FC of CHF by 5,7% (p<0,05) and 6.4% (p<0,05), respectively, compared with the values of I FC CHF. The slowing down of the flow velocity into the early filling phase of the LV (DT, ms) in patients of the first group with I, II, and III FC was 201,5±14,76, 181,1±36,8 and 177,15±42,88 ms respectively, with a significant decrease in patients with II and III FC CHF by 11,3% (p<0,001) and 13,7% (p<0,001), respectively, compared with the I FC of CHF.Table 1. Initial indices of LV diastolic function in patients with I-III FC of CHF
 |
| |
|
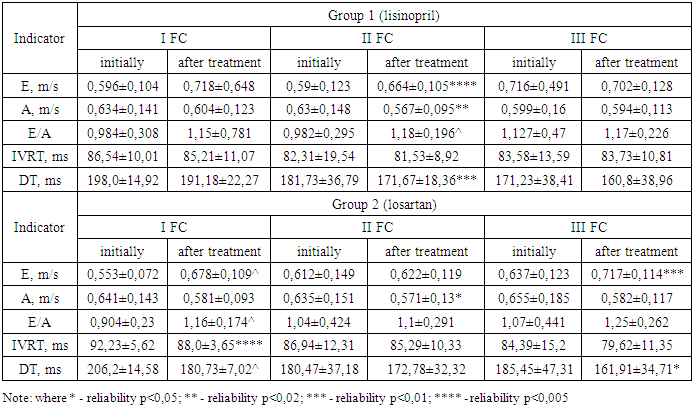
Analysis of the types of diastolic dysfunction in both groups, depending on the FC of CHF, showed that in patients with I FC of CHF, diastolic dysfunction was diagnosed in 76% (38) of both groups, with only type I (delayed relaxation) 58% (29 patients) and type II - (pseudonormal) in 18% (9 patients). In patients with II FC of CHF, diastolic dysfunction was determined in 80% (80 patients) of patients of both groups: type I (delayed relaxation) in 60% (60 patients), type II (pseudonormal) in 19% (19 patients), III type (restrictive) – in 2% (2 patients). In patients with III FC of CHF, diastolic dysfunction was determined in 81,2% (60 patients) of patients of both groups: type I (delayed relaxation) in 60,3% (44 patients), type II (pseudonormal) in 21,9% (16), type III (restrictive) in 6,8% (5 patients).In patients of the first and second group with eGFR≤60 ml/min/1,73 m2, GFR was – 50,9±8,8 and 52,7±7,3 ml/min/1,73 m2, respectively; with eGFR≥60 ml/min/1,73 m2 – 79,6±14,8 and 76,96±14,1 ml/min/1,73 m2, respectively. In terms of the level of eGFR, patients were referred to stages 1-3 of CKD. Stage 3 CKD: 54 (80,6%) patients with stage 3A CKD, 13 (19,4%) patients with stage 3B CKD. The dependence between the diastolic function and eGFR indices was revealed: in patients with eGFR≤60 ml/min/1,73 m2 – the rate of E by 6,8% (p<0,05) was significantly lower in comparison with this index in patients with eGFR>60 ml/min/1,73 m2; the mean positive correlation was observed in the groups of patients with CHF with eGFR 60< and eGFR>60 ml/min/1,73 m2 between eGFR and speed E - r=0,38 and r=0,46, respectively.In Group I patients with I and III FC of CHF after treatment with lisinopril, the diastolic function values tended to improve these indicators without achieving reliable values; with II FC CHF - a significant increase in E and E/A - by 12,6% (p<0,005) and 19,6% (p<0,001), a decrease of A - by 10,1% (p<0,02), respectively in comparison with the initial indicators. In Group II patients with I FC CHF, after treatment with losartan, there was a significant increase in the E and E/A peak by 22,7% (p<0,001) and 28,4% (p<0,001), IVRT and DT truncation by 4,6% (p<0,01), and 12,4% (p <0,001); with II FC decrease A - by 10,1% (p<0,05); with III FC of CHF, an increase in E and a decrease in DT by 12,6% (p<0,01) and 12,7% (p<0,05) compared to baseline (Table 2).Table 2. Dynamics of indices of LV diastolic function in patients with I-III FC of CHF (M ± SD) against the background of 6-month treatment
 |
| |
|
Against the background of treatment there was an improvement in the E peak in both groups with eGFR≤60 and eGFR>60 ml/min/1,73 m2. In patients with eGFR≤60 ml/min/1,73 m2 of the first and second group, the rate of E increased by 14,8% and 15,7% (p<0,02), respectively, in the background of treatment; in patients with eGFR>60 ml/min/1,73 m2 there was a tendency to increase E by 2,7% and 7,5%, respectively, compared with baseline.The results of our studies in patients with CHF showed that renal dysfunction appeared at the subclinical stage, when most patients have no clinical signs of renal insufficiency. It is believed that with CHF – renal dysfunction develops as a result of a decrease in cardiac output, followed by a decrease in the filling of the arterial bed, renal hypoperfusion, increased resistance of renal vessels, and decreased renal blood flow [10]. However, a number of studies have shown a lack of a clear link between the indices of myocardial contractility and diastolic dysfunction markers in CHF [15]. A number of authors have established that the type of delayed relaxation is the predominant type of diastolic dysfunction in elderly and senile patients with diastolic heart failure [7]. At the same time, the features of structural and functional heart disorders, depending on the presence of anemia and chronic kidney disease, were also determined. It has been established that the adverse effect of decreased renal function on the course of chronic heart failure is due to worsening diastolic function, in particular, an increase in the time of isovolumeic relaxation in patients with I-II functional class of CHF.According to many studies, the positive effect of ACE inhibitors and AAR is due to the fact that they reduce the initially high blood pressure in glomeruli of the kidneys, which stops the development of glomerulosclerosis [9, 10]. The increase in intraglomerular pressure is the result of hypertension of efferent arterioles, i.e. Their spasm due to the high activity of angiotensin II. Raising RAAS is a characteristic feature of the course of CHF [8].The results obtained by us are confirmed by the results of a number of studies conducted in patients with CHF. Organ protective and anti-remodeling effects of ACE inhibitors and AAR are known from the results of studies [8, 11]. These positive properties of ATII receptor blockers have been the subject of a special discussion for the first time after the publication of the results of the LIFE study, the RENAAL study, which included patients with essential hypertension with maximal cardiovascular risk [13]. Thus, in patients with CHF it is very important to evaluate the relationship between the clinical course of the disease, structural and geometric parameters, with the evaluation of diastolic functions of the left ventricle and renal function parameters for early screening and predicting cardiovascular risk and optimizing treatment. Involvement of the kidneys can be considered as an important determinant of the progression of CHF, that requires a timely diagnosis and treatment of CHF [10, 12].
4. Conclusions
The analysis of baseline diastolic function in patients with CHF revealed diastolic dysfunction in 81.8% of patients with CHF, with a predominance of delayed relaxation in 59.3% of patients and an increase in the number of patients with a restrictive type of diastolic dysfunction in patients with III FC of CHF. The dependence between the parameters of the diastolic function – the rate of E and eGFR was revealed. Patients of the first and second groups with I-III FC of CHF after 6 months of treatment had an improvement in diastolic function LV. On the background of treatment in patients with CHF with eGFR≤60 ml/min/1,73 m2 there was a significant increase in the rate of E in both groups of patients without statistically significant differences.
References
| [1] | Arutyunov A.G.. 2014, ACE inhibitors in CHF: the validity of therapy when changing its goals. Difficult patient, 5: 1-8. |
| [2] | Marinina O.S., Efremova O.A., Kamyshnikova L.A., Logvinenko S.I., Pridatchina L.S.. 2014, Diastolic dysfunction of the myocardium in patients with chronic heart failure of different genesis. The scientific result, 20-23. |
| [3] | Mejonov E.M., Vyalkina Yu.A., Shalaev S.V. 2017, The prevalence of renal dysfunction and its effect on prognosis in patients with acute heart failure. Heart failure, 18 (2): 87-93. |
| [4] | Moiseev S., Strijakov L.. 2013, Efficacy of lisinopril in chronic kidney disease. Doctor, 4: 32-36. |
| [5] | Moiseeva V.S., Mukhina N.A. 2014, National recommendations. Cardiovascular risk and chronic kidney disease: strategies for cardio-nephroprotection. Ed. Russian Cardiology Journal, 8 (112): 7-37. |
| [6] | Polonsky V.M. 2016, LIFE: new prospects for losartan. Family Medicine, 6 (68): 70-74. |
| [7] | Solovyov DA. 2015, Features of the geometry of the left ventricle in patients with metabolic syndrome and diastolic dysfunction by the type of relaxation disturbance. Young Scientist, 20: 142-145. |
| [8] | Tereshenko S.N., Jirov I.V., Narusov O. Yu., Mareev Yu.V. and others. 2016, Diagnosis and treatment of chronic and acute heart failure. Clinical recommendations. Cardiologic Herald, 2: 23-33. |
| [9] | Akbari A., Clase C.M., Acott P., Battistella M. et al. 2015, Canadian Society of Nephrology Commentary on the KDIGO Clinical Practice Guideline for CKD Evaluation and Management. Am J Kidney Dis, 65(2): 177-205. |
| [10] | Damman K., Masson S., Hillege H. et al. 2013, Tubular damage and worsening renal function in chronic heart failure. J Am Coll Cardiol Heart Fail, 1: 417-424. |
| [11] | ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2016. European Heart Journal, 2016; 37 (27): 2129-2200. |
| [12] | Inker L.A., Astor B.C., Fox C.H., Isakova T. et al. 2014, KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis, 63(5): 713-735. |
| [13] | Levey A.S., Bosch J.P., Lewis J.B. et al. 2010, A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med, 461-470. |
| [14] | Nagueh S.F., Smiseth O.A., Appleton C.P. et al. 2016, Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. European Heart Journal – Cardiovascular Imaging, doi:10.1093/ehjci/jew082. |
| [15] | Stevens L.A., Li S., Kurella Tamura M. et al. 2011, Comparison of the CKD Epidemiology Collaboration (CKD-EPI) and Modification of Diet in Renal Disease (MDRD) Study equations: risk factors for and complications of CKD and mortality in the Kidney Early Evaluation Program (KEEP). Am J Kidney Dis. 57: S9–S16. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML