-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2018; 8(8): 204-212
doi:10.5923/j.ajmms.20180808.07

Pain Mechanisms and Pharmacological Pain Relieving Interventions in Rheumatic Diseases
Edit Vereckei, László Hodinka
2nd Department of Rheumatology, National Institute of Rheumatology, Budapest, Hungary
Correspondence to: Edit Vereckei, 2nd Department of Rheumatology, National Institute of Rheumatology, Budapest, Hungary.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Effective management of pain is one of the greatest challenges among medical interventions. Pathological pain arises most frequently in the musculoskeletal system. The first obligatory step is the localisation of the source and to identify the dominant mechanism, as mechanical, infectious, auto-inflammatory or central. Most musculoskeletal pain by type are nociceptive, however also neuropathic components may be present in acute and chronic painful conditions. Immediate and consequent pain relief in acute pain is essential to prevent the development of chronic pain and pain behaviour. The first alerts for an infectious or auto-inflammatory danger are the alarmins, molecules induced by pathogens or tissue destruction in the cells of the innate host defense. They are activated via their receptors expressed and the signaling cascades producing and secreting their bioactive mediators and pro-inflammatory cytokines. These molecules bind to the respective receptors on the peripheral terminal of the nociceptive neuron and elicit neurotransmitter and action potential response as pain signal for the central nervous system. These repeated signals sensitize the peripheral terminal and the central junctions, causing an increased and persistent pain sensation even in higher nuclei and cortical areas. Most frequent conditions causing mechanical locomotor pains are vertebral joint dystorsions, discogen radicular compressions, osteoporotic vertebral fractures, hip and knee osteoarthritis. Neuropathic mechanisms are dominant in the complex regional pain syndrome as hip algodystrophy or the shoulder-hand syndrome. Inflammatory pain mechanisms, including cytokine effects operate in septic arthritis, rheumatoid and psoriatic arthritis, idiopathic juvenile arthritides, spondyloarthritides, and in acute and chronic gout. The most effective pharmacological tools of pain management are the classical and innovative molecules with special reference to bioproteins and synthetic molecules targeting the key points on the pain pathway. Considerations of recent recommendations may promote the right therapeutic decisions in the care of rheumatic patients suffering from musculoskeletal pain.
Keywords: Musculoskeletal pain, Mechanical pain, Inflammatory pain, Pain mediators, Cytokine-inhibition
Cite this paper: Edit Vereckei, László Hodinka, Pain Mechanisms and Pharmacological Pain Relieving Interventions in Rheumatic Diseases, American Journal of Medicine and Medical Sciences, Vol. 8 No. 8, 2018, pp. 204-212. doi: 10.5923/j.ajmms.20180808.07.
Article Outline
1. Introduction
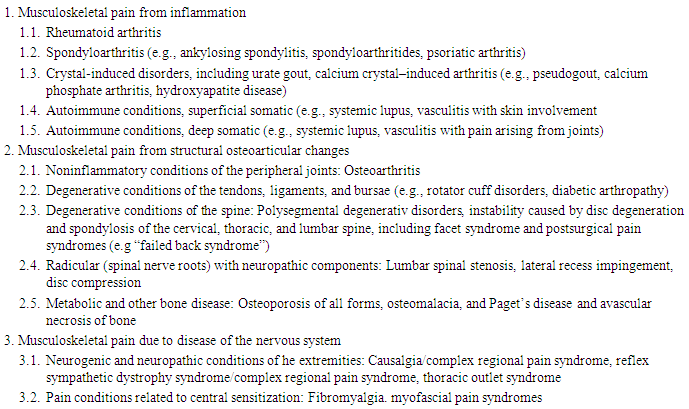
- After several phrasings, the original definition of pain was formulated in 1974 and this was adopted by the International Association for the Study of Pain (IASP) in 1975. The first version has been analysed, discussed, explained and re-constructed in the interim years, however it became more complicated [1, 2]. Attempts have been made to sublimate it into a less sophisticated wording but to retain the original substance) as: Pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage”. This definition seems to be accurate and simple and is valid for any type of pain. It is easily applicable into every context and for use in research and clinical practice [3]. The basic classification of acute and chronic pain is usually based on the history (by recent consensus lasting more than three months) and the patient reported pain characteristics (which may vary primarily by and depend much more on the mechanism and type of pain). These may be subjective and are too simple for differentiating multi-faced and protean nature of pain sensations. We think this is particularly true for musculoskeletal pains. Musculoskeletal (MSK) pain occurs along a continuum from sudden and strong pain impulses as an acute gouty attack through the undulating remissions and flares of systemic inflammatory arthritides to the chronic widespread MSK pain syndromes and the purely central pain of fibromyalgia [4-6]. Pain domain is strongly weighed in all instruments measuring MSK disease severity, activity, burden and Quality of Life of MSK patients and Patient Reported Outcomes truly reflect their perceptions. The vast majority of MSK pain originates from chronic conditions. Epidemiological surveys and studies show, that MSK pain was reported from 13.5 to 47 per cent by persons in European countries and 11.4 to 24 per cent of the pains were chronic [7]. The main characteristics of chronic MSK pains are that they affect mainly older people, are very heterogeneous regarding pain experience and personal impact, regional localisation is common, majority is mechanical (osteoarthritis), lesser part is inflammatory (arthritides), dysfunctional pain is frequently present without somatic pathology, originating from central sensitization. Moreover, pain caused by rheumatic diseases represent a significant social and economic burden in general. This burden is more prominent in societies of less developed countries where inequities and disparities are present and threatens patients in poorer socioeconomic status [8]. For the effective management of MSK pain the recognition of the mechanism and the identification of type are essential. The spectrum of painful rheumatic conditions are characterized and collected by the American College of Rheumatology Task Force (ACR), re-considered according to mechanisms (i.e. inflammatory, structural damage and pain processing) [9] and re-classified according to the proposed classification for ICD-11 (WHO) [6]. These are summarized, amalgamated and shown in Table 1.
|
2. Pain Mechanisms and Types in Musculoskeletal Diseases
- Pains depending on their origin may be physiological, alerting to avoid a momentary noxious event or to initiate to discover the internal source. Pathological pains signalize a danger threatening the integrity of the body. The border between physiological and pathological may be overlapping [10]. Types of pathological pain are nociceptive, neuropathic and dysfunctional. The respective mechanisms usually may combine in different pathological conditions. This opportunity should be taken into consideration when therapeutic strategy is planned [11, 12].The MSK nociceptive pain arises in the connective tissues of articular, vertebral and soft MSK structures as joints, in the juxta articular cortical bones, bone and tendon interfaces (entheses) or cartilagineous junctions of bones, muscles, tendon sheets and bursae. They result from mechanical stress, overload or overuse (regional syndromes, osteoarthritis, osteoporotic vertebral compression) microvascular damage (algodystrophy) or inflammation. Inflammatory pain is a broad spectrum from gouty attack or chronic gout, acute septic arthritis and spondyilitis to the constant activity or flares of systemic arthritides as rheumatoid or psoriatic arthritis, spondyloarthritides as ankylosing spondylitis [13]. In the cases where radicular or neural compression complicates the nociceptive event, as in disc herniation or tunnel syndromes, neuropathic mechanisms and sensations join the “common” nociceptive pain (Baron Neuropathic LBP). Neuropathic pain is characterized by dysaesthesia and bizarre feelings coloring the pain as e.g. burning, tingling, itching, feeling painful the neutral, warm or cold touch [14]. Dysfunctional pain may develop from the continuous nociceptive trigger which decreases the threshold of the receptors on the nociceptor distal terminal (peripheral sensitization) and the repetitive action potentials and transmitters released sensitize the proximal neurons (central sensitization). Dysfunctional is the central pain which is a result of pathological processing of primarily not painful impulse and substantially belong to the psychiatric diseases (Treede Pain IASp WHO). The centrally sensitized condition lead to the activation of glial cells, creating a local inflammatory focus. As a result of the excitement of neurons and their environment, the backwards spreading of the action potential (antidrom lead), a the same inflammatory mediators and neurotransmitters are released at the peripheral terminal and sustain the inflammatory triggers (neurogenic inflammation, neuroinflammation) [15, 16].
3. The Pain Signal and the Transmission and Perception of Nociceptive Pain
- The peripheral danger signals (heat, protons, mechanical triggers and chemical mediators, as biogenic amines, substance P, oligopeptides, Nerve Growth Factor, etc) activate the nociceptive neurons which respond with opening of ion channels, resulting in the action potential and activate kinase cascades resulting in the production of excitatory neurotransmitters, primarily glutamate. Substance P, which is a potent tachykinin transmitter, acts on the NK-1 (neurokinin) receptor, while the similar neurokinin-A acts on the NK-2 receptors. By changing the amino acid sequence in the substance P chain incorportating a d-amino acid, the first generation of the competitive antagonists was developed, which inhibits selectively the NK-1 receptor. The prostaglandins, like PGE1 and prostacyclins, directly stimulate the nociceptor, while PGE2 boosts the release of substance P also from the sensory neuron and intensifies the algogenic effect of 5-HT and bradykinin. Moreover, bradykinin releases prostaglandins, thus has an intense “self-sensitizing” effect. The specific antagonist of bradykinin, icatiban may be a new perspective in analgesia. The capsaicin and the vanilloid receptors are the targets of capsaicin (the hot substance of paprika and chili pepper) selectively stimulates the nociceptive terminals. It exerts its effect by linking to the vanilloid VR-1 receptor expressed on the nociceptive neuron. Similar VR-1 agonist is the resiniferatoxin, also used as a desensitizing agent like capsaicin in clinical pain management. Among the excitatory transmitters of the nociceptor, the glutamic acid acts by linking to the AMPA-receptor, a natrium-potassium channel opener receptor, plays a role in the fast synaptic transmission to the first spinal cord synapse. AMPA (alpha-amino-3-hydroxy-5-methyl-3-oxo-1,2-oxazole-propionic acid) locates in the central nervous system and activates also glutamate receptors [17]. The pain impulses is transmitted to the dorsal horn secondary neuron of the substantia gelatinosa. The lateral spinothalamic tract ends in the thalamus, where the impulses are integrated. After switching a part of the fibres moves towards the cortex, other axons reach the subcortical structures as the putamen, caudate nucleus and pallidum. The tertiary line is a series of the thalamocortical neural connections. The exact localisation of the pain, the subjective pain sensation arise in the postcentral gyrus [18]. Here is the appreciation and processing is performed. However, this is not equivalent of the complete pain treat, because the affective emotional component is based on subjective experiences, it is influenced by mood and therefore show very heterogeneous intensity, even within the same individual [19, 20].Parallel to the ascendant connections an inhibitory descendant system operates which retards the spreading painful impulses. The periaqueductal gray (PAG) is one of the main anatomical target of exogeneous and endogeneous opioids acting on the mu receptors expressed on the neurons here [21-23]. Here is the descendant inhibitory tract activated [24]. Another key neurotransmitter of the inhibitory system is the 5-hydroxi-triptaminr (5-HT), i.e. the serotonin. Serotonin regulates sleep, wakefulness, hunger and aggressivity. The noradrenergic impulses originating from the locus coeruleus and the gamma-amino-butyric acid (GABA) as well, play another important role in the descending inhibitory tract. Noradrenalin, or norepinephrine is the regulator of mood, alertness, vigorousness and danger perception. GABA is a general inhibitory neurotransmitter, retarding the discharge of neurons [25].
4. The Inflammatory Pain
4.1. The Danger Alarm Molecules
- The inflammatory answer, including pain sensation is provoked potentially by pathogens, injury of own tissues by mechanical, physical or chemical origin, even by inert materials as crystals activating the innate auto-inflammatory mechanisms [26]. The common ancient surface molecules and toxins of the pathogens, primarily bacteria, (Pathogen Associated Molecular Patterns, PAMPs) mitochondria and nucleic acid fragments of the injured cells, their metabolic products released through the cell disruption (ATP, adenosine, urate and calcium pyrophosphate and hydroxyapatite) and other substances (heat-shock proteins, transcription factors as the High-Mobility Group Box Protein, HGMB1), in their collective noun alarmins and Danger Associated Molecular Patterns, DAMPs all indicate the threatening tissue damage for the protective mechanisms of the body [27].
4.2. The Tissue Damage-sensing Receptors
- The Pattern Recognition Pattern Receptors (PRRs) are expressed on the cells of the innate and adaptive answer, namely on the antigen presenting dendritic cells, macrophages, and on several connective tissue and epithelial cells as well. Most important receptors are he members of the Toll-like receptors, TLRs, the retinoic acid inducible gene 1 receptor (RIG-1), the receptor for glycation end products RAGE and the nucleotide-binding oligomerization domain (NOD-like, NLR) receptors. These receptors activate primarily the Nuclear Factor kappa B (NFkB) transcription factor through its kinase enzymes and the caspase-1 enzyme in the integrated system of the inflammasome, respectively. The NFkB induces the synthesis of several inflammatory cytokine (for example the COX-2 cyclooxygenase), while the caspase-1 generates the active IL-1 cytokine from the pre-formed Interleukin-1 beta.
4.3. Mediators and Cytokines Provoking and Sustaining Inflammatory Pain
- The connective tissue, myeloid and immune cells activated through the kinases of the receptor and intracellular signaling, synthesize several inflammatory cytokines (as well as chemokines and interferon), which induce a self-strengthening inflammatory cascade twisting further in the particular tissue environment. The interleukin1 family (IL-1F) represents eleven analogical interleukins. Out of them the IL-1 alpha basically has an alarmin function, the IL-12 and the IL-33 activate both the cells of the natural and adaptive immune system [28, 29]. The IL-23 primarily differentiates the T lymphocytes into Th17 direction, and thus indirectly intensifies the pleiotropic protecting and inflammatory effect of the IL-17 interleukin family [30]. The injuries of the intestinal epithelium stimulate the production of IL-17 through IL-23, in accordance with the IL-7 T Cell differentiating factor, with the mediation of the Mucosa-Associated Invariant T Cell, MAIT cell [31]. The mast cells have a determining role in raising the inflammatory pain sensation. The tissue mast cells are of myeloid origin, in their basophil granules they contain several inflammatory, allergy and anaphylaxis and pain-inducing substances, which are released into their environment partly through degranulation, partly through direct emission. They carry danger alarm receptors, at their activation they suddenly release histamine, serotonin, bradykinin, substance P and the Platelet Activating Factor (PAF) [32]. They synthesize and emit prostaglandins, TNF and interleukin-6 cytokine. In the inflamed tissue environment, neurotropic differentiating factors are also arisen, for example Nerve Growth Factor, NGF [33]. The key cytokines of the acute, chronic and neurogenic inflammation are the TNF and the IL-6 [34].
4.4. The Receptors and Neuronal Transmitters of the Nociceptor
- The receptors sensing the nociceptive pain signals, are expressed in the largest amount on the peripheral terminal of the axon of dorsal root ganglion neuron. They can be found on the whole neuronal membrane, on the proximal terminal of the neuron as well. The permanent and strong irritation intensifies their expression and reduces the threshold of the neuron. Besides the listed alarmins, in the tissue environment of nociceptor along with the listed mediators, potassium and hydrogen ions, proteinase enzymes, neurokinine and glutamate are also present in the “sensitising soup”. These lead to the continuous induction of action potentials through the respective receptors by calcium inflow. The receptors of the transient receptor potential cation channel family V and A have a central role in this (TRPV1 and TRPA1). The receptors of the listed cytokines and the prostaglandin EP4 receptor for PGE2 can be found on the nociceptive neuron and on the higher levels of the central nervous system as well [35].
4.5. The Sensitization and the Neurogenic Inflammation
- The nociceptor neuron produces itself the main inflammatory cytokines (IL-1 beta, IL-6, TNF) and emits them into the environment of its proximal terminal as well. On the higher levels of the central nervous system, the glial cells, the Schwann cells and the present macrophages create an inflammatory micro-environment producing mediators and cytokines. Here and in the neurons, further neuropeptides: cerebral, spinal cord and insulin-like nerve growth factors and calcitonin gene-related peptide (CGRP) are synthesized. Through these the neural environment is damaged and neuropathic pain is arisen. This is a significant component of the central sensitization. The antidromic impulses passes through in the dorsal root ganglion neuron, towards the periphery as well and on the distal terminal, substance P and CGRP are secreted contributing to the peripheral sensitization. The neurogenic inflammation is a part of the self-sustaining pain cycle in this way and composes the neuropathic component of chronic inflammatory pain [36]. All listed mediators, cytokines and their receptors represent potential therapeutic targets. However, the most effective ones are the inhibitory interventions acting on the key-points.
5. General Considerations for Pain Management in Rheumatology
- The pain-related medical history should be recorded in the most accurate way and the type of pain (nociceptive, neuropathic, mixed) has to be defined as far as possible. In order to record the actual intensity of pain the use of any generally accepted pain measuring scale variant (visual analogue scales, Likert scale) is recommended. Efforts should be made to identify the source and cause potential causes of the pain. The patient should be informed about the potential causes of his pain, and the patient should be informed about their connection to his illnesses, the opportunities, expected effects and risks of the therapy. The therapeutic decisions have to be shared with the adequately informed and consented patient. The patients must be classified according to their individual potential risks before starting their relevant therapy, especially with non-steroidal antiinflammatory drugs (NSAIDs), opiates and opioids, and in certain cases corticosteroids, especially when long term and/or high dose treatment is planned [37]. The undesirable effects of the NSAIDs basically relate to their mode of action which may harm the homeostatic functions of prostanoids, as circulation, renal functions, hemostasis, bronchial tone with special reference to the elderly and children. Liver and renal functions, impaired metabolisation and excretion, the toxicity of applicable analgesics and co-medication should be taken into consideration in therapy planning [38]. Topical products are recommended as first choice in cases with local, regional musculoskeletal disease pattern, primarily to treat mild and moderate pain of soft tissue origin [39]. Compared to creams and pastes, dosing is safer and absorption is better in case of patches especially those developed by Transdermal Drug Delivery System (TDDS) technology [40, 41, 42]. Topical menthol has been used as a non-opioid pain reliever since ancient times. A modern understanding of its molecular mechanism of action could form the basis for generating targets for discovery of novel non-opioid analgesic drugs. Menthol is a selective activator of transient receptor potential melastatin-8 (TRPM8) channels and is also a vasoactive compound [43]. As a topical agent, it acts as a counter-irritant by imparting a cooling effect and by initially stimulating nociceptors and then desensitizing them. topically applied menthol may also activate central analgesic pathways. At high concentrations, menthol may generate cold allodynia [44].The recommended hierarchy of analgesics to treat dominating nociceptive musculoskeletal pain is as follows. 1. In case of mild and medium acute pain – if local treatment is not applicable or it is not sufficiently effective – acetaminophen (paracetamol) is the first oral pain-killer to choose. Due to its heap-toxic effect, accumulation should be avoided, even in the short-term. To avoid this, longer periods are necessary between the particular doses (could be given at every 4 hours maximum).2. The COX-1 and COX-2 inhibitors are effective and safe pain-killers. However, the COX-2 inhibitor therapy and COX-1 inhibitors even combined with gastro-protective medicines (PPI) cause gastrointestinal side-effects in risk-patients with the same probability. It is necessary to obtain all information about the patient’s physiological conditions, co-morbidites and their medication before choosing the appropriate medicine. 3. In case of heavy pain or the inefficiency of the above therapy, strong opioid agonist should be chosen, if a weak opioid – even with acetaminophen or NSAID – is not efficient enough.
6. Therapeutic Strategy for Non-inflammatory Painful Conditions in Rheumatology
- The most common painful rheumatologic conditions are shown in Table 1. Acute painful episodes originate from shoulder periarthritis, vertebral joint dystorsion, osteoporotic vertebral compression fracture and intervertebral disc herniation with or without radicular compression. Manifestations of complex regional pain syndrome types I and II (mainly CRPS1 as hip and shoulder algodystrophy, typical hand-shoulder syndrome) may develop subacutely and are long lasting. Severe, mechanically provoked enthesites, as the hamstring syndrome, Achilles tendinitis, humeral epicondylitis, supraspinatus tendinitis of the supraspinatus muscle are typical regional soft tissue syndromes. Peripheral nerve compressions (tunnel syndromes) are areas shared with neurology [10, 45]. All of the conditions listed may persist and the acute-subacute pain evolves into chronic pain and neuropathic components may appear in any state. In acute phase of mechanical spine diseases besides temporary rest in painless position, it is recommended to give paracetamol (2-3 grams per day), until the pain is remitting along with relaxation. In case of heavy pain which may last even at rest, tramadol/paracetamol combination is recommended. The appropriate dose requires titration. Tramadol in mono-therapy 100-400 mg/day could be given orally. It can be combined with paracetamol or can be given in parenteral form as well [46].In case of pains threatening to become chronic, combinations of analgesics and muscle relaxants in mixed infusions – along with metamizole, tramadol, guaifenesine, especially if signs of radicular compression are present – methylprednisolone added with diuretic may be an alternative and a good therapeutic choice. However, the superiority of analgetic/muscle relaxant combinations over monotherapies is disputed, ready-mixed diclofenac and orphenadrine infusion combination is commercially available and are in use. For effective management of pain resistant to these modalities opioids (codein, dyhidrocodein, oxycodone) can be given. Endogeneous demetilation of codeine, oxycodone and hydrocodone is done by the CYPD6 enzyme, resulting the generation of active metabolites. The genetic polymorphism of the CYPD6 was revealed and this could correlate to the specific variations of their analgesic effect. Fentanyl is one of the strongest opioid analgetic that has gained clinical application, about 100 times stronger than morphin. This strong analgesic effect lasts for a short period (30-60 minutes), explained by its intense lipophylic nature and the fast redistribution. Lipophylity of tramadol is advantageous and practical for transdermal application to prevent the transition of acute painful conditions into chronic ones [47]. Local targeted infiltrations with soluble injections of anesthetics with or without corticosteroids may be adjuvant interventions targeting well definable painful structures. In cases of osteoporotic vertebral compression paracetamol and tramadol could be given in the above as well mentioned form. Preference of weak opioids is recommended applying the aforementioned formulations, primarily oxycodone orally. In case of inefficacy fentanyl could be considered calculating the limits of tolerance of the patient. Recently, warning dangers of overuse and addiction are emphasized. Complex regional pain syndrome types, hip and shoulder algodystrophy and the typical hand-shoulder syndrome belong to the group of disease patterns with acute and sub-acute, even chronic pain. Their main characteristics are severe pain, swelling and vasomotor changes, i.e. oedema, and skin atrophy. These illnesses can be reliably diagnosed based on the 2003 Budapest diagnostic criteria [48]. Most commonly these evolve after trauma, splinting or surgery. The irritation of sensory nerve, pathological sympathetic answer, permanent spasm of metarterioles, opening of shunts, consecutive capillary stasis are in the center of its pathomechanism. The bone catabolism is dominant and is followed by trophic disequilibrium because of the increased pressure in the affected tissues. Pro-inflammatory mediators (serotonin, histamine, bradykinin) are secreted by degranulating mast cells as a result of central sensitization and neurogenic inflammation.In the pathological cascade NSAIDs have limited effects, opioid, supported with corticosteroids should rather be given. Corticosteroids are recommended only in the early stadium, in large doses (30-40 mg/day) and could be effective for 2-4 weeks. Calcitonine blocks the osteoclast activity, also vasodilators, prazosine, antidepressants, bisphosphonates, intrathecal baclofen (a GABA receptor antagonist) can be given and sympathetic blockade may be considered (2). Based on theoretical considerations of neuropathic nature of the condition gabapentin and pregabalin are possibly effective, however convincing evidence is lacking. Another therapeutic target would be phosphodesterase inhibition e.g. with tadalafil, and blocking the N--methyl-D-aspartate (NMDA) effect on its receptor, as glutatamate antagonisation. The effective treatment of this illness is a multi-disciplinary, challenge and requires also methods of physical medicine. In cases of severe, mechanically provoked enthesitis, like hamstring syndrome, or caused by repetitive stress other tendons, as of Achilles or supraspinatus muscle tendons, per-oral or topical NSAIDs, local infiltrations or transcutaneous nerve stimulation (TENS) as adjuvant treatments may be effective [48].
7. Therapeutic Tools Targeting Inflammatory Pain
7.1. Cyclooxygenase Inhibition
- Cyclooxygenase enzymes are induced permanently in the inflammatory process, signalized via the receptors of proinflammatory monoamines, oligopeptides and cvytokines and the NFkB transcription Their prostanoid products, prostaglandine E2 first of all, acting on the EP4 receptor is among the key effectors inducing inflammatory pain along the nociceptive pathway. COX-1 and COX-2 inhibitors are in the frontline of symptomatic pain relieving antiinflammatory therapeutic strategies [49, 50].
7.2. Corticosteroids in the Management of Inflammatory Pain
- The corticosteroids - beyond their metabolic effects - are the most effective general anti-inflammatory drugs. They mitigate the inflammatory pains in a dose-dependent manner. The basis of their pain-killing effect is that they enter into the nucleus by linking to the soluble cytoplasmic corticosteroid receptor and there they block the activation of pro-inflammatory gene sections in the DNA by the transcription factor NFkB preventing the synthesis of more pro-inflammatory cytokines and enzymes. Since this gene-activation is one of the key-points of inflammatory cascade corticosteroids have a robust indirect effect on pain induction [51].
7.3. Cytokine Inhibition
- The genetic engineering or gene construction and the biotechnology made possible the targeted therapy of autoimmune inflammatory diseases. The key pro-inflammatory cytokines (TNF, IL-6, IL-1) are not only the inducers of persistent immune-mediated inflammation, but via their receptors expressed on the neurons, glial and astrocytic elements in the nervous system, the generate and modulate the pain perception along the pain pathway [29, 52]. Their neutralization by monoclonal antibodies or receptor fusion proteins inhibits not only the inflammatory activity and holds the progression of arthritides but rapidly relieve the arthritic pain. This effect may precede the decrease of inflammatory activity and is demonstrable by functional MRI of the brain [53]. Very recently, the Janus kinase inhibitor baricitinib – inhibiting I and II type pro-inflammatory cytokine signaling, first of all IL-6 – in rheumatoid arthritis was shown to exert this effect before other clinical symptoms decrease [54]. Acute gouty attack is a clear example of the acute unbearable rheumatic pain, however crystal induced inflammation (monosodium urate, calcium pyrophosphate or hydroxyapatite as inert structures activate the inflammasome and generate interleukin 1 secretion). The classical drug colchicine was shown to inhibit intracellular tyrosine kinases and so its effect corresponds to the inhibition of IL-1 and IL-6 [55]. Neutralization by monoclonal antibodies the Nerve Growth Factor NGF) for hip and knee osteoarthritis [56]. and the Calcitonine Gene Related Peptide CGRP) recently for migraine but potentially for CRPS is in the clinical trial phase [57].
8. Recommendations for Musculoskeletal Pain Management in Current Guidelines
- Recommendations for the clinical practice targeting general practitioners, specialists and rheumatology health professionals are itemised in current guidelines listed in the Table 1. with the respective source references. The short descriptions contain the relevant aspects of pain management selected for musculoskeletal conditions. The very recent recommendations of the European League Against Rheumatism (EULAR) on the approach to pain management have been developed primarily for health professionals, collecting and evaluating rheumatoid arthritis and osteoarthritis guidelines, meta-analyses and expert recommendations. The recommendations (10 items) and the “overarching principles” are fundamental for all medical professions involved in musculoskeletal pain management. The four “overarching principles” include requirements as the patient-centered framework, understanding all aspects of musculoskeletal pain, including basic knowledge and the ability to differentiate between localised and generalised pain having knowledge on the pain types and co-existing conditions [58]. Expert groups of international associations developed disease-specific guidelines for the treatment of most frequent rheumatological diseases, as osteoarthritis and low back pain including recommendations for pain management [59-69].
9. Conclusions
- Rapid and successful pain therapy is one of the most important medical challenge and obligation. If a permanent musculoskeletal pain is present the cause should be cleared and eliminated as completely as possible, because this pain harms the patient’s Quality of Life and carries the threat to develop the late consequences of deep psychic changes. The effective intervention should be individual, considering the age and health state of the patient, and the severity and dangerous nature of the cause. The medical professional should make decisions shared with the patient discussing the actual opportunities, benefits and risks. Knowledge of recent therapeutic modalities and recommendations concerning their application may help in the right and responsible decision and follow-up.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML