-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2018; 8(8): 171-177
doi:10.5923/j.ajmms.20180808.02

Results of Intra-Arterial Thrombolytic Therapy for Ischemic Stroke in Uzbekistan
Bahtiyar Gafurov, Shukhrat Mubarakov, Natalya Dadamyants, Farrukh Djalalov, Amet Seydaliev
Republican Research Center of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

A thrombolytic therapy performed in the conditions of a “therapeutic window” is one of the perspective methods of early recanalization of the occluded vessel at acute stroke. 22 patients with acute ischemic stroke admitted within 3-6 hours from the stroke starting have been examined. All the patients were performed cerebral angiography with following intra-arterial thrombolytic therapy. A complete recovery of neurologic deficit was registered in 5 (22.7%), a partial regression – in 11 (50%), no effect – in 3 (13.6%) and a lethal outcome – in 3 (13.6%) patients. Recanalization level made up 72.7%. Obtained results testify a high therapeutic efficiency of intra-arterial thrombolytic therapy.
Keywords: Acute stroke,Intra-arterial thrombolytic therapy,Streptokinase, Therapeutic window
Cite this paper: Bahtiyar Gafurov, Shukhrat Mubarakov, Natalya Dadamyants, Farrukh Djalalov, Amet Seydaliev, Results of Intra-Arterial Thrombolytic Therapy for Ischemic Stroke in Uzbekistan, American Journal of Medicine and Medical Sciences, Vol. 8 No. 8, 2018, pp. 171-177. doi: 10.5923/j.ajmms.20180808.02.
1. Introduction
- Recent achievements in refining of pathogenic mechanisms of ischemic stroke (IS) development allowed to determine a main strategy of a pathogenic therapy in the most acute period - to improve the brain tissue perfusion by means of early occluded vessel recanalization (Wardlaw and Warlow, 1996; Vereschagin et al., 2002; Suslina et al, 2005) According to the last guidelines of the European Stroke Initiative (EUSI) and American Stroke Association a thrombolytic therapy (TT) performed within “a therapeutic window” is one of the perspective methods for early recanalization of the occluded vessel in acute stroke patients performed in the conditions of “a therapeutic window” [1-2, 4].Plenty of prospective randomized studies have demonstrated efficacy and safety of TT at the IS and gave a possibility for its wide use currently many neurovascular centers in the world widely use the intravenous thrombolytic therapy (ITT). The results of conducted meta-analysis testify the efficiency and safety of ITT at adherence of conventional clinical guidelines [3,6-8]. But intravenous thrombolytic therapy has some limitations. Particularly, the ITT is inefficient for thromboembolisms of large main arteries (thromboembolisms of internal carotid artery and M1 segment of middle cerebral artery (MCA)). The ITT is most effective method at small thromboembolisms of the second level cerebral arteries. Majority of patients with IS have contraindications for ITT associated with frequent hemorrhagic complications. Besides, among up-to-date thrombolytic agents approved as systemic thrombolytics only intravenous recombinant tissue plasminogen activator (rt-PA) is used. The rest of drugs (streptokinase, urokinase and prourokinase) are not used as systemic thrombolytic agent due to the frequent complications [9-11]. Selective intra-arterial thrombolytic therapy (IATT) with various thrombolytic agents is considered as a perspective method. According to some authors (Suslina Z.A. 1997, Furlan A. 1999, Hacke W.1998) data the IATT has the following advantages:1. A high efficiency in achieving recanalization of occluded vessels (up to 80%).2. IATT is more reasonable at the occlusion of high caliber vessel.3. IATT is performed by introduction of less quantity of thrombolytic agent – it leads to the reduction of hemorrhagic complications occurring at IATT [5].
2. Materials and Methods
- 22 patients with IS (12 males and 10 females) were examined. The age range was 22 to 85 years. All the patients were taken to the Republican Research Center of Emergency Medicine within 6-hours “therapeutic window”. Clinical-neurologic symptoms testified acute ischemic stroke in MCA basin from the right – in 14 patients and from the left – in 7 cases and in 1 patient – in vertebrobasilar basin. At admission all patients were performed multi-sliced computer tomography (MSCT) with “Brilliance 40” (Philips, Netherlands). All patients were carried out complex ultrasound investigation methods to determine IS subtype. Color duplex sonography (CDS) of brain main arteries was done on EUB-600 (Hitachi, Japan) with a 7.5 Hz transducer. Cerebral blood flow was estimated by clinical routine transcranial Doppler (TCD) ultrasound examination on MT-1010 apparatus (Mindray, China) with a 2 MHz transducer via temporal acoustic window. Sonoline-Omnia, a digital ultrasound system with 2-D, color flow, and Doppler imaging modes (Siemens, Germany) completed with a 4.0 MHz transducer was used to perform echocardiography. MSCT angiography was performed with the help of “Brilliance 40” (Philips, Netherlands) according to the standard methods using automatic syringe Angiomat (Illumena, Germany) by the way of intravenous bolus introduction of 80-120 ml of an X-ray contrast medium (ultravist or omnipak) in the concentration of 300-350 mg/ml at the rate of 3.0-4.5 ml/s. The data was processed by means of the EBW (Extended Brilliance Workspace) platform (Philips, Netherlands). Philips Allura Xper FD20 fixed X-ray system was used to conduct cerebral angiography and IATT following common femoral artery puncture by Seldinger’s technique. Proximal internal carotid and vertebral arteries were catheterized by introducers and 5F (1 Fr=0.32 mm) diagnostic catheters (Cordis Inc., USA). A non-ionic X-ray contrast medium omnipak 300-350 by Nycomed, Switzerland was injected manually with 10-ml syringe. Digital subtraction angiography (DSA) in majority of cases was performed in standard views - posterior and lateral, with a velocity of 2 - 3 frames per second involving arterial, parenchymal and venous phases. Additional series in various projections were taken at necessity. The obtained angiographic data were processed on Xcelera, an integrated multi-modality image management system for cardiovascular information (Philips, the Netherlands) and were jointly analyzed by an interventional radiologists and a neuropathologist. At the presence of indications for IATT, the diagnostic catheter was substituted by the conductor one (Envoy 5Fr, Cordis Inc., USA). Then under the control of Roadmapping option Cordis microcatheter Prowler 10 with the help of a micro-conductor was navigated to the occluded area. 50,000 U of streptokinase bolus dosing has been infused for 60 seconds. After a control angiography the infusion of 200,000 U streptokinase (up to 200000 U) during 30 minutes was performed. A thrombolytic therapy was performed to the patients who were selected according to the recommendations of American Academy of Neurology (American Academy of Neurology Practice Advisory, 1966; Norris J. et al., 1998; The European Stroke Initiative Executive Committee and UESI Writing Committee, 2003; Albers G.W. et al., 2004, Adams H.P. et al., 2007, Skvortsova V.I., 2007). The IATT efficacy and safety as well as the degree of recanalization were estimated by neurological status monitoring data involving NIHSS scale, by the control cerebral MSCT, MSCT angiography and TCD data 2-3 days after the procedure.
3. Results
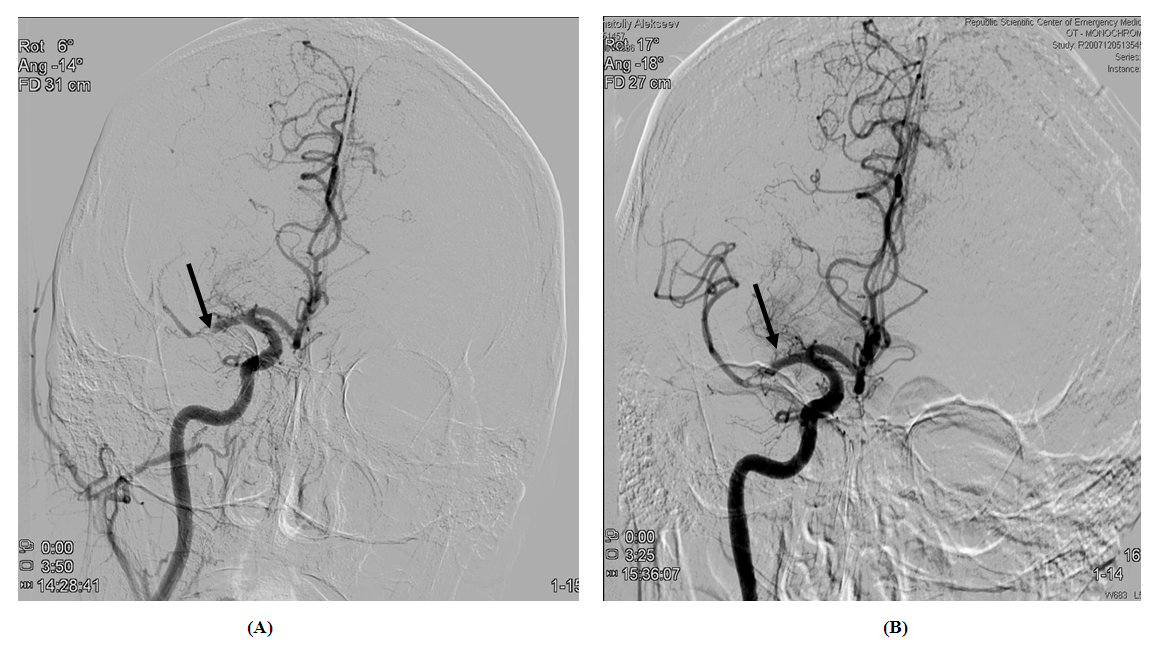
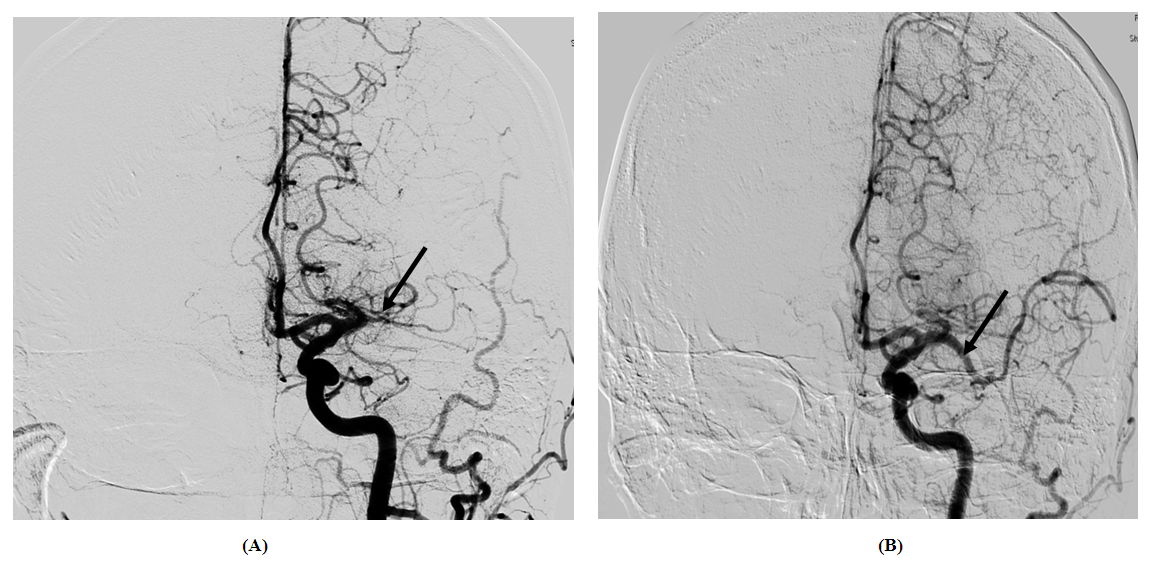
- All patients were admitted to the Republican Research Center of Emergency Medicine within 6 hours starting from the onset of IS symptoms. In all cases the admission CT registered no organic changes in the brain – it testified that all patients were admitted in the period of “a therapeutic window”. Color duplex sonography (CDS), clinical routine transcranial Doppler (TCD) ultrasound examination and echocardiography were used to diagnose atherothrombotic stroke in 16 patients. The CDS results in those patients revealed the signs of atherosclerotic lesions of main brain arteries with various degree of stenosis. TCD at admission revealed hemodynamically significant reduction of linear blood flow velocity along MCA on the side of occlusion with a coefficient of interhemispheric asymmetry exceeding 50%. Cardioembolic subtype of stroke was diagnosed and confirmed by ECG and echocardiography in 6 patients. In one of them ischemic stroke was developed due to arrhythmic form of coronary heart disease (CHD), in the rest 5 patients – due to various valvular defects, particularly in 1 case – on the background of congenital heart disease, in 1 patient – due to cardiac myxoma and in the rest 3 ones – due to acquired rheumatic heart disease with atrial fibrillation-like heart rhythm disorder. Cerebral angiography detected acute MCA occlusions in all cases (Fig.1-A, 2-A).
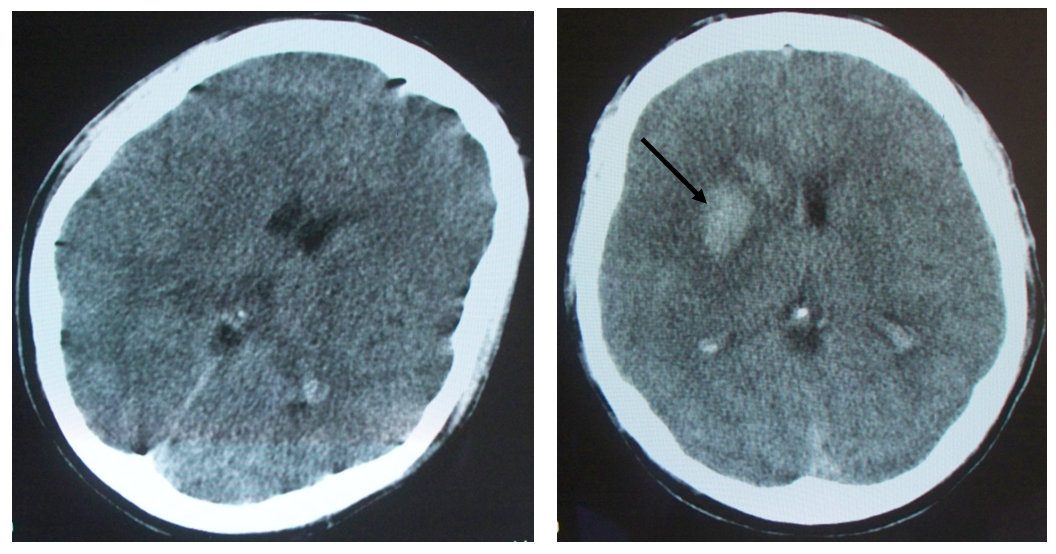
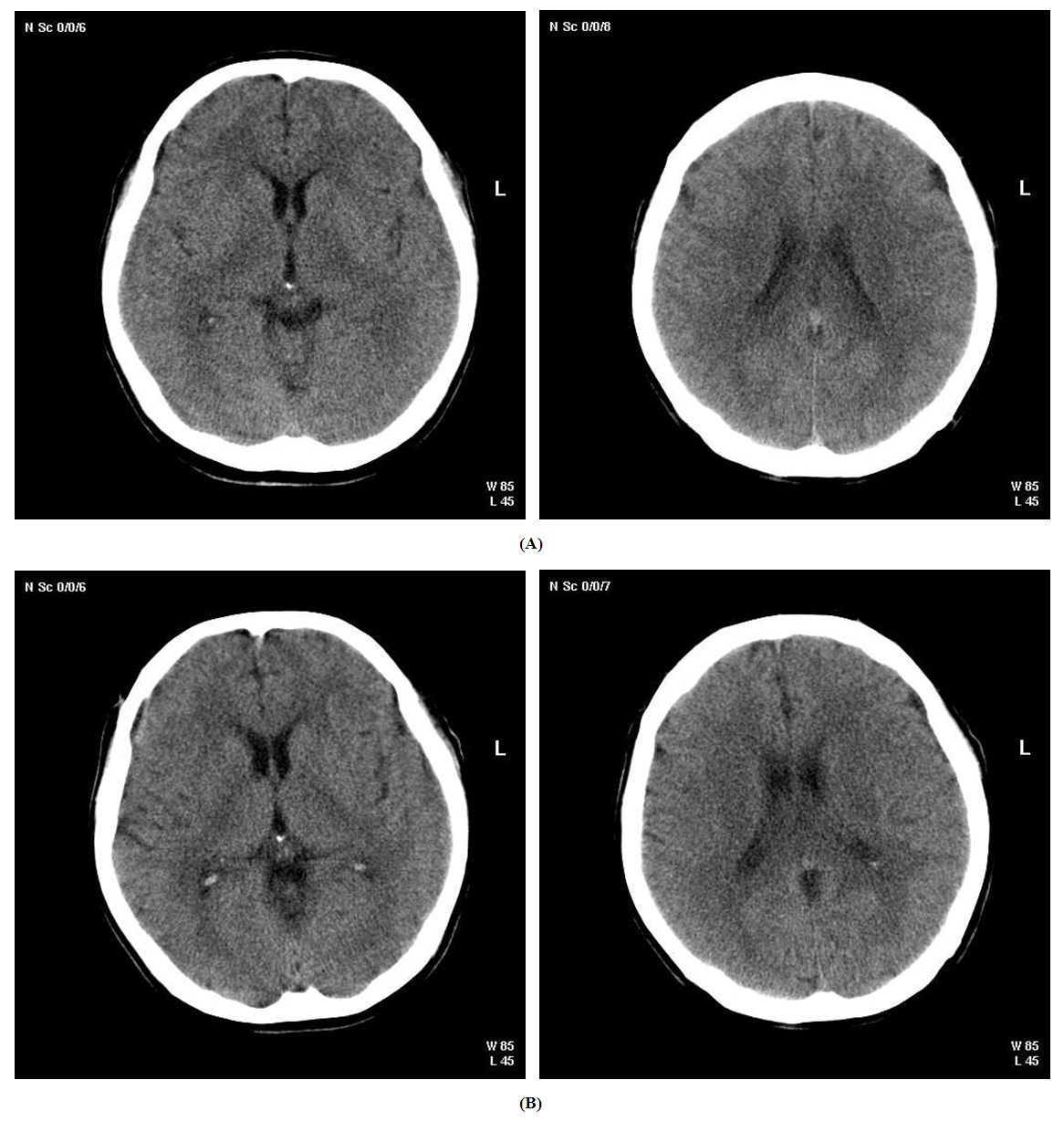 | Figure 3. (A) pre-IATT brain CT scan of 61-years old male patient with acute ischemic stroke in the left hemisphere of MCA basin, (B) brain CT scan of the same person 3 days after IATT |
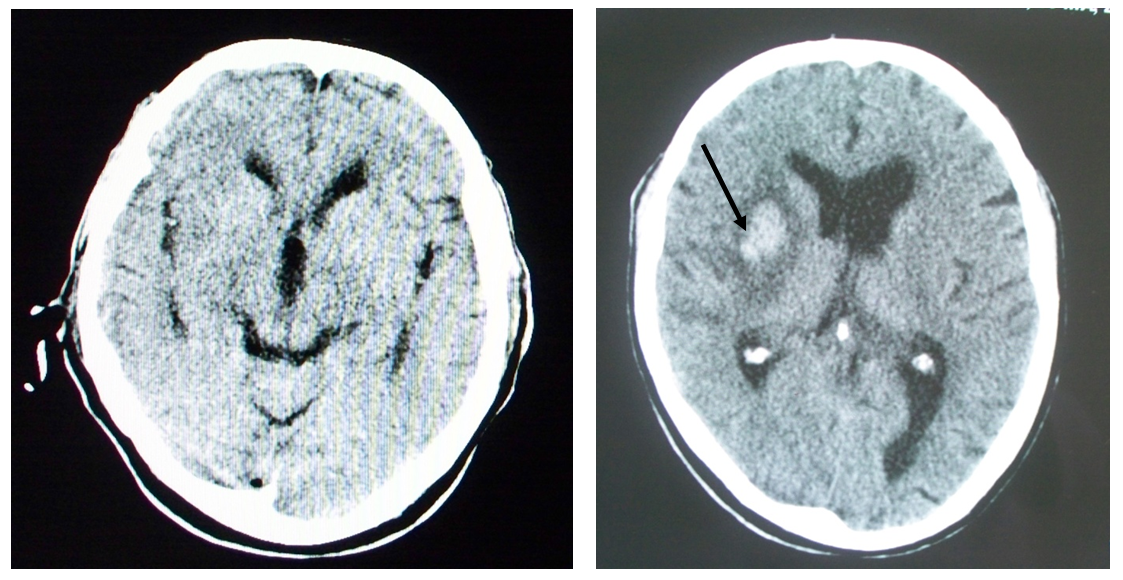
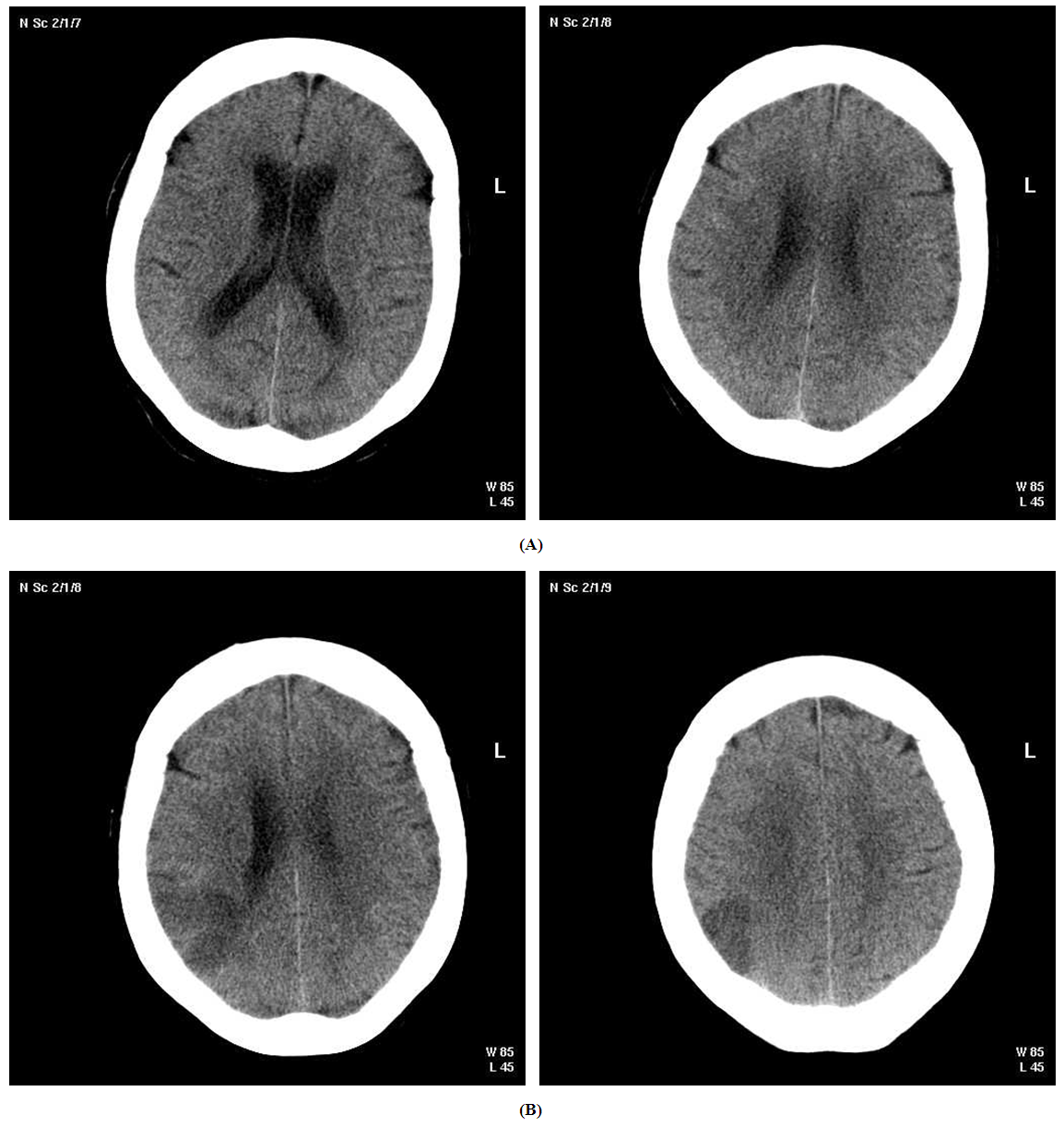 | Figure 4. (A) pre-IATT brain CT scan of 75-years old female patient with acute ischemic stroke in the right hemisphere of MCA basin, (B) brain CT scan of the same person 3 days after IATT |
4. Conclusions
- 1. Inter-arterial thrombolytic therapy with the use of streptokinase is an efficient and comparatively safe method for recanalization of occluded vessel in patients with IS;2. Inter-arterial thrombolytic therapy in ischemic stroke patients is an efficient and safe method within 6-hours “therapeutic window”, but the highest efficiency of IATT is observed within 3-hours range. 3. Asymptomatic perdiapedetic or parenchymal hemorrhagic transformation can be considered as efficient thrombolysis marker.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML