-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2018; 8(7): 132-136
doi:10.5923/j.ajmms.20180807.03

Prevalence of Acute Respiratory Tract Infection (ARI) in Paediatric Patient Attending National Hospital Abuja, Nigeria
Ajobiewe H. F.1, Ajobiewe J. O.2, Nehemiah Edem2
1Biological Sciences Department, Bingham University, Karu, Nigeria
2Imo State University Owerri, Nigeria
Correspondence to: Ajobiewe H. F., Biological Sciences Department, Bingham University, Karu, Nigeria.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study, on the prevalence of Acute Respiratory Tract Infection(ARI), spans the period of six months, from 1st January to the 30th of June, 2017, at the National Hospital Abuja, located at the central business district of the Federal Capital City of Nigeria. The data were retrospectively collected from patient’s folders and attendance register from the medical records department at the general Paediatric Outpatient department, National Hospital over the period of six months, 713(59.3%) males and 490(40.7%) females. Over the six-month period, out of 1203. The result showed that among paediatric unisex patients seen, 279 were diagnosed with ARI which is 23.19%. The overall ARI mean, µ, was 25; Standard Deviation, SD, was 12 .41 while the Standard Error, S.E. was, 6.2 with t4.7 tab ≥ t cal. 4.0 at (P≥0.05). From the study carried out, there were diseases found to be casually and confoundly associated with ARI which includes sepsis, malaria, dehydration, diarrhoeal disease, febrile convulsion, pneumonia, sickle cell anaemia, and meningitis. Our observation showed that ARI among children between the ages 0-5 years was not significantly high (P≥0.05) in agreement with popular opinion from literature search [1, 18]. Despite the devastating and fatal nature of ARI, as it starves the body of oxygen-it is suggested that the non -significance could be favoured due to the clemency of the environment/ weather which these patients were exposed to, when this research was conducted.
Keywords: Acute Respiratory Tract Infection (ARI), Environment, Paediatrics, Fatal, Clemency
Cite this paper: Ajobiewe H. F., Ajobiewe J. O., Nehemiah Edem, Prevalence of Acute Respiratory Tract Infection (ARI) in Paediatric Patient Attending National Hospital Abuja, Nigeria, American Journal of Medicine and Medical Sciences, Vol. 8 No. 7, 2018, pp. 132-136. doi: 10.5923/j.ajmms.20180807.03.
Article Outline
1. Introduction
- Acute respiratory tract infections (ARIs) are heterogeneous and complex group of diseases caused by a wide range of pathogens in which the possible anatomic site(s) extend from the pharynx to the alveoli. In conjunction with diarrheal diseases and malnutrition, ARIs constitute the major causes of mortality and morbidity among under-five children of the developing world. The percentage of deaths due to all causes for ARI is between 2 times and 6 times higher in less developed countries than in developed countries. ARI constitute one-third of the deaths in children under-five in developing countries. ARIs are not confined to the respiratory tract and have systemic effects because of possible extension of infection or microbial toxins, inflammation, and reduced lung function [2].Diphtheria, pertussis (whooping cough), and measles are vaccine-preventable diseases that may have a respiratory tract component but also affect other systems.Except during the neonatal period, ARIs are the most common causes of both illness and mortality in children under five, who average three to six episodes of ARIs annually regardless of where they live or what their economic situation is Childhood acute respiratory infection (ARI) which is a significant public health problem especially in developing countries [3, 4]. ARI is an acute infection of any part of respiratory tract and related structures including paranasal sinuses, middle ear, and pleural cavity. ARIs include a diverse group of diseases ranging from self-limiting illnesses to bronchiolitis and pneumonia that may require medical care. It includes all infections of less than 30 days duration except those of the middle ear where the duration of an acute episode is less than 14 days. World Health Organization estimates ARI causing 3.9 million deaths throughout the world every year. It is one of the important priority areas for the concerned stakeholders in the health sector especially in developing countries. The occurrence of ARI is determined by the exposure to various risk factors. Air pollution is a risk factor for both acute and chronic respiratory disease. One half of the world's population is exposed to high concentrations of solid fuel smoke that are produced by inefficient open fires, mainly in the rural areas of developing countries. Solid fuel smoke possesses the majority of the toxins found in tobacco smoke and has also been associated with a variety of diseases including ARI in children. Globally, indoor air pollution from solid fuel use is responsible for 1.6 million deaths due to pneumonia, chronic obstructive pulmonary disease and lung cancer. The highest exposures to second-hand smoke are found in Eastern Europe, the Western Pacific and South-East Asia, with more than 50% of some population groups exposed. Environmental factors such as overcrowding coupled with poor ventilation at homes and work places may make the health effects of indoor air pollution more pronounced. Exposure is particularly high among women and children, who spend most time near the domestic health [5].
2. Literature Review
- Acute respiratory tract infection (ARI) is a serious infection that prevents normal breathing function. It usually begins as a viral infection in the nose, trachea (windpipe), or lungs. If the infection is not treated, it can spread to the entire respiratory system. Acute respiratory infection prevents the body from getting oxygen and can result in death. According to the World health organization [6] acute respiratory infections kill an estimated 3.9 million children annually worldwide. Identification and early treatment can reduce the burden of ARI among children. Acute respiratory infection (ARI) is a major public health problem worldwide [7]. It is a significant cause of morbidity and mortality and main reason for utilization of health services among children. Identification and intervention of major risk factors can reduce the burden of ARI among children [8].However, in developing countries, mortality rates are up to 30 times higher (or more). The high morbidity rate makes ARI the main cause for the utilization of health services, representing in the entire world 20-40% of the appointments at paediatric services and 12-35% of the hospitalizations. According to data provided by OPAS/OMS5, pneumonias are responsible for 20-40% of the admissions of children under the age of 5 in developing countries [9].Studies have shown the importance of social factors for ARI mortality, such as family size, education level, and density of dwellers in the residence. We should emphasize the degree of maternal education as a social factor related to the infant’s survival, since the reports point out that the lower the education level is, the higher are the ARI rates and seriousness. It is known that the lack of essential nutrients interferes with the development of humoral and cellular organic defence systems. Thus, though the incidence of ARI is globally similar, the difference is that infections of the inferior airways, especially pneumonia, are more frequent and severe in developing countries due to several factors, especially malnutrition. Smoking is still a serious public health problem, being particularly significant in childhood, since respiratory problems in children (mainly infants) who are passive smokers are more severe and often require hospitalization [10].The study of ARI in public services is justified by the difficulty in optimizing the structure of public health services for this kind of medical assistance. This difficulty in solving health problems ends up with an unsatisfactory involvement between health service agents and relatives. This leads to the negligence of basic orientations, since the natural evolution of most ARI cases is not complicated [8]. This contributes to the misuse of drugs, and to the same child going to different health service offices, which deviates from the objectives of the ARI Program, commended by the Brazilian Ministry of Health. Acute respiratory infection is a serious infection that prevents normal breathing function. It usually begins as a viral infection in the nose, trachea (windpipe), or lungs. If the infection is not treated, it can spread to the entire respiratory system. Acute respiratory infection prevents the body from getting oxygen and can result in death. [11]
2.1. Who is at Risk for Acute Respiratory Infection?
- While it is almost impossible to avoid viruses and bacteria, certain risk factors increase the likelihood of developing acute respiratory infection. The immune systems of children and the elderly are more prone to be affected by viruses and later bacteria. Those most frequently implicated are Adenoviruses, Rhinoviruses Myxoviruses and Paramyxoviruses while the bacterium is the Pneumococcus [11]. Children are especially at risk because of their constant contact with other kids who could be virus carriers. Children often do not wash their hands regularly, rub their eyes, and put their fingers in their mouths, resulting in the spread of viruses. People with heart diseases or other lung problems are more likely to contract an acute respiratory infection. Anyone whose immune system might be weakened by another disease is at risk. Smokers also are at high risk and have more trouble recovering from it [11].
2.2. Ways to Reduce the Occurrence of Acute Respiratory Infection in Children
- Most causes of an acute respiratory infection are not treatable. Therefore, prevention is the best method to ward off harmful respiratory infections. Practice good hygiene by doing the following:Ÿ Wash hands frequently, especially after having been in a public place.Ÿ Avoid touching one's face, especially eyes and mouth, to prevent introducing germs into one's system.Ÿ Always sneeze into one's arm of the shirt or in a tissue. Although this may not ease one's symptoms, it will prevent the spreading of infectious diseases.
2.3. Diagnosis of Acute Respiratory Infection
- In a respiratory exam, the doctor focuses on the patient’s breathing. Breath sounds in the lungs are checked for fluid and inflammation. The doctor may peer into the nose and check the throat. If diagnosed early, over-the-counter medications can help alleviate symptoms while the virus runs its course. However, if the infection is advanced, an X-ray or CT scan (computer tomography) may be needed to check the condition of the lungs. Lung function tests have shown to be useful as diagnostic tools and for prognosis purposes. Pulse oximetry, also known as pulse oximeter, may be used to check how much oxygen gets into the lungs. A physician may also need a sputum (material coughed up from the lungs) sample to check for the type of virus causing the disease. Some of potential complications of acute respiratory infection involve; respiratory arrest, respiratory failure and congestive heart failure.
2.4. Types of Acute Respiratory Infection
- Acute respiratory infections (ARIs) are classified as upper respiratory tract infections (URTIs) or lower respiratory tract infections (LRTIs). The upper respiratory tract consists of the airways from the nostrils to the vocal cords in the larynx, including the paranasal sinuses and the middle ear. The lower respiratory tract covers the continuation of the airways from the trachea and bronchi to the bronchioles and the alveoli. However, the proportion of mild to severe disease varies between high- and low-income countries, and because of differences in specific etiologies and risk factors, the severity of LRIs in children under five is worse in developing countries, resulting in a higher case-fatality rate. Although medical care can to some extent mitigate both severity and fatality, many severe LRIs do not respond to therapy, largely because of the lack of highly effective antiviral drugs. Some 10.8 million children die each year [12]. Estimates indicate that in the year 2000, 1.9 million of them died because of ARIs, 70 percent of them in Africa and Southeast Asia [13]. The World Health Organization (WHO) estimates that 2 million children under five die of pneumonia each year [14].
2.5. Treatment Guidelines
- Current recommendations are for Co-trimoxazole twice a day for five days for pneumonia and intramuscular penicillin or chloramphenicol for children with severe pneumonia. The problems of increasing resistance to co-trimoxazole and unnecessary referrals of children with any chest wall indrawing have led to studies exploring alternatives to the antibiotics currently used in ARI case management. One study indicated that Amoxicillin and Co-trimoxazole are equally effective for nonsevere pneumonia [15] though Amoxicillin costs twice as much as Co-trimoxazole. With respect to the duration of antibiotic treatment, studies in Bangladesh, India, and Indonesia indicate that three days of oral Co-trimoxazole or Amoxicillin are as effective as five days of either drug in children with nonsevere pneumonia [16]. In a multicenter study of intramuscular Penicillin versus oral Amoxicillin in children with severe pneumonia, [17] find similar cure rates. Because patients were treated with oxygen when needed for hypoxemia and were switched to other antibiotics if the treatment failed, this regimen is not appropriate for treating severe pneumonia in an outpatient setting. WHO (1990) [11] recommends administering oxygen, if there is ample supply, to children with signs and symptoms of severe pneumonia and, where supply is limited, to children with any of the following signs: inability to feed and drink, cyanosis, respiratory rate greater than or equal to 70 breaths per minute, or severe chest wall retractions. Oxygen should be administered at a rate of 0.5 liter per minute for children younger than 2 months and 1 liter per minute for older children. Because oxygen is expensive and supply is scarce, especially in remote rural areas in developing countries, WHO (1993) [6] recommends simple clinical signs to detect and treat hypoxemia. Despite those recommendations, a study of 21 first-level facilities and district hospitals in seven developing countries found that more than 50 percent of hospitalized children with LRI were inappropriately treated with antibiotics or oxygen [10] —and in several, oxygen was in short supply. Clearly, providing oxygen to hypoxemic babies is lifesaving, though no randomized trials have been done to prove it.
3. Methods
3.1. Population and Sample Size
- The population consists mainly of patients seen in the Out-patient Paediatric section of National Hospital, Abuja. The researcher was given access to their files to obtain all necessary information needed for the success of this research. The population size and sample size are approximately 1,300 (it could be less). This study was carried out for a period of six months (January to June 2017). The researcher found the observation method of data collection to be useful, as the researcher was able to observe the patients that were brought in for the treatment of ARI. The researcher was also granted access to some of the patients file to gather all necessary information The sources used to gather all necessary information needed in this research work was mainly secondary data; over the period in which the research work began up until its completion. Both null and researcher’s /alternative hypotheses were instruments used for the analysis of findings. HYPOTHESES H0 – Prevalence of ARI among children aged 0-5years (in/out patients) attending National Hospital, Abuja is not significantly high.H1 – Prevalence of ARI among children aged 0-5years (in/out patients) attending National Hospital, Abuja is significantly high.Where, Ho = Null Hypothesis, and Ha = Alternate or Researcher’s Hypothesis.
4. Results
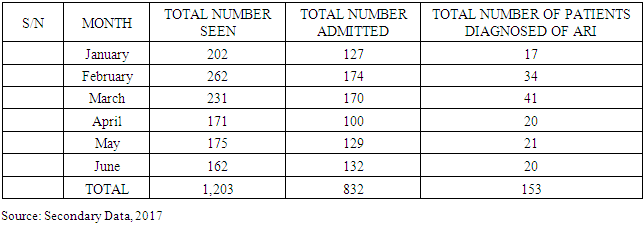
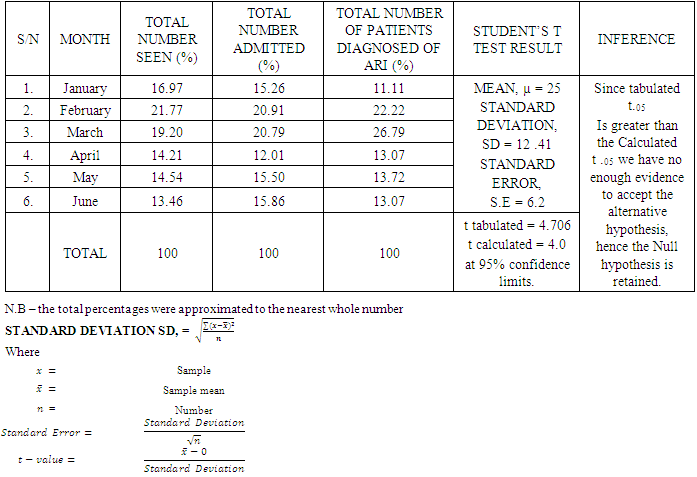
- There were a total of 1203 cases of ARI seen at National Hospital over the period of six months, 713 (59.3%) males and 490 (40.7%) females. In January, a total number of 202 (16.97%) patients were seen, 17 (11.11%) of them were diagnosed of ARI. In February a total number of 262 (21.77%), 34 patients (22.22%) were diagnosed of ARI. In March a total number of 231 (19.20%), 41 (26.79%) patients were diagnosed of ARI. In April a total of 171 (14.21%), 20 (13.07%) patients were diagnosed of ARI, 10 (13.88%). In May a total of 175 (14.54%), 21 (13.72%) patients were diagnosed of ARI. In June a total of 162 (13.46%), 20 (13.07%) patients were diagnosed of ARI. (P≥ 0.05). From the study carried out, there were diseases found to be associated with ARI which includes sepsis, malaria, dehydration, diarrhoeal disease, febrile convulsion, pneumonia, sickle cell anaemia, and meningitis. Sepsis was the highest with 42 patients (27.45%), followed by malaria with 34 patients (22.22%), dehydration with 20 patients (13.07%), diarrhoeal disease with 15 patients (9.80%), febrile convulsion with 11 patients (7.18%), pneumonia with 7 patients (4.57%), sickle cell anaemia with 6 patients (3.92), and meningitis with 1 patient (0.65%).
4.1. Table A: Showing Total No of Patients Seen, Admitted and Diagnosed for ARI
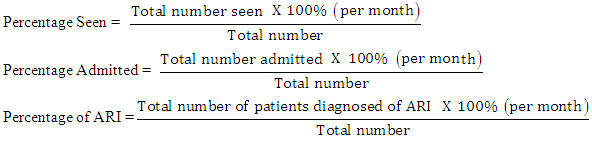
4.2. Percentage
4.3. Table B: Showing Total Percentage of Patients Seen, Admitted, Diagnosed of ARI
5. Discussion
- Subjecting the hypotheses to critical analysis revealed the following; H0 – prevalence of ARI among children aged 0-5years (in/out patients) attending National Hospital, Abuja, Nigeria is not significantly high. (P≥0.05). We have no enough evidence to reject the null hypothesis, Ho, thus it was retained instead of the alternative/researcher’s hypothesis, Ha. The research showed that within the stipulated time for the research, the occurrence of ARI among children between the ages of 0-5 years is not significantly high, (P≥0.05) and this may be due to the weather conditions in agreement with earlier researches carried out by Lucy Eberechukwu, Tochi Ada (2015) [18] and Cherian et al, (1990) [1] - their researches proved that ARI is more prevalent during the rainy season than the dry season. ARIs have remained a major contributor to morbidity among children, especially children in developing countries. In the study carried out, a total of 1203 cases of ARIs were seen over a 6-month period (during the harmattan). Most cases of ARI seen in this study were upper respiratory tract infections which is consistent with the reports by other authors. The incidence of pneumonia in developing countries is high due to the increased prevalence of malnutrition, low birth weight and indoor air pollution in these countries.
6. Conclusions
- Despite the devastating and fatal nature of ARI, as it starves the body of oxygen-it is suggested that the non -significance could be favoured due to the clemency of the environment/ weather which these patients were exposed to, when this research was conducted.”.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML