F. G. Nazirov, O. M. Gulamov, A. R. Akhmedov, B. Z. Mukhamedov
Republican Specialized Scientific-Practical Medical Centre Named after Academician V.Vahidov, Tashkent, Uzbekistan
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The article is devoted to a surgical treatment of esophageal cancer as well as discussion and the role of modern approach to this complicated pathology. The analysis of surgical interventions in esophageal cancer treatment according to the location and extent of the process has been conducted. A new type of esophageal anastomosis allowing to reduce postoperative specific complications has been offered.
Keywords:
Еsophageal cancer, Esophageal anastomosis, Limphodissection, Esophagoplasty, Gastroplasty
Cite this paper: F. G. Nazirov, O. M. Gulamov, A. R. Akhmedov, B. Z. Mukhamedov, Surgical Treatment Results in Patients with Esophageal Cancer, American Journal of Medicine and Medical Sciences, Vol. 8 No. 7, 2018, pp. 123-127. doi: 10.5923/j.ajmms.20180807.01.
1. Introduction
A surgical treatment of esophageal malignant diseases refers to the type of complicated restorative surgeries. A big amount of esophageal surgeries has been performing with successful outcomes for the recent decades. It is mainly connected with a sufficient provision of anaesthetic and resuscitation service, and also with a big practical experience having gathered by operating surgeons in this field [1-2, 4-5]. Currently esophagoplasty is performed as single-stage operation (graft formation is ended by application of cervical or intrapleural esophageal anastomosis [5, 9-10].Some issues concerning the indications for surgeries at the esophageal cancer are disputable. The matters of surgical approaches, anastomosis positions (intrapleural, cervical) and also the variants of anastomosis formation still remain opened [8, 10]. Mainly, the proponents of Lewes’s or Charlock’s surgeries use these types of surgeries in patients with esophageal cancer and they can be regarded as the correct ones due to their efficacy. But, at the same time, inefficiency of esophageal anastomosis in intrapleural position is more dangerous for patient’s life [1-2]. Extrapleural anastomosis are more safety and even at their inefficiency seldom lead to the fatal complications [1, 4-7, 9]. The arisen complications are easily eliminated by conservative methods [2, 5]. There are differences of opinions between surgeons and oncologists about the approaches. The surgeons prefer less traumatic types (abdominal-cervical approach), but the oncologists often use thoracic-abdominal one because of its radicalism [8, 11-12].According to above mentioned situations, the development of the optimal surgeries types at esophageal cancer remains actual in the esophageal surgery.
2. Materials and Methods
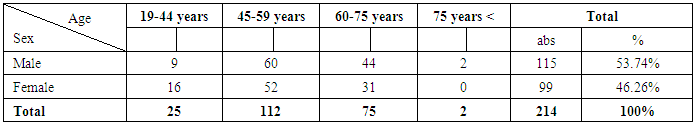
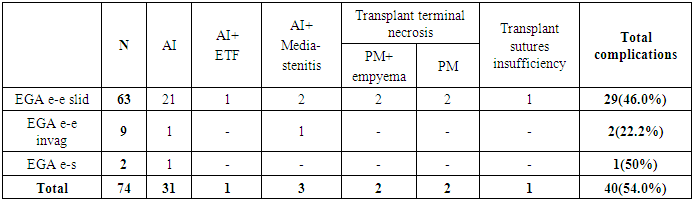
Different types of esophagectomy with esophageal anastomosis formation were performed in 214 patients between 1991 and 2015 at the department of esophagus and stomach surgery of the Republican Specialized Scientific-Practical Medical Centre named after academician V.Vahidov. All surgeries, in spite of technical difficulties while performing restorative esophageal operations were carried out simultaneously. All principles of radicalism were kept. The less traumatic approaches were chosen as far as possible. Randomizing of patients by sex and age presented in Table 1 shows that a majority of patients – 137 (54.67%) were at working-age and 75 (35.0%) were at mature age. Table 1. Randomizing of patients by sex and age
 |
| |
|
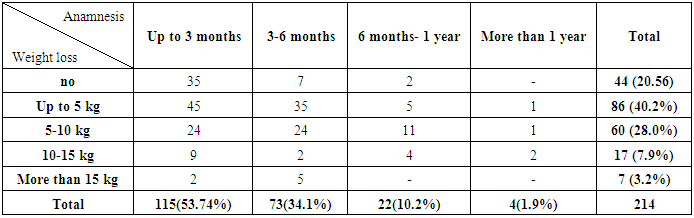
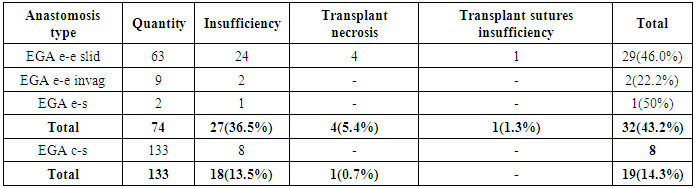
As it is seen from Table 2, a big quantity of patients admitted to our Centre in the period of up to 3 months (53.74%) and it can be regarded as prognostic favorable factor. Alimentary cachexia associated with dysphagia mostly was observed in the first half-year from disease onset.Table 2. Randomizing of patients by anamnesis and weight loss
 |
| |
|
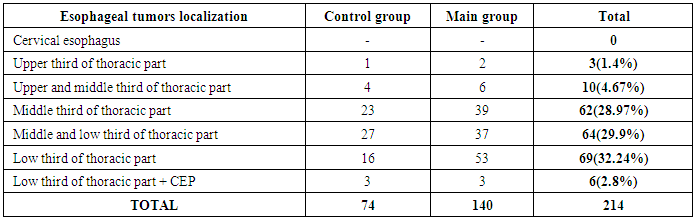
Dysphagia was a main clinical manifestation and the cause of patients visit to the hospital. According to the dysphagia rate by Chernayvskiy A.A. (1991), the patients were randomized as follows: rate I (dysphagia only to hard food) - 50(23.3%), rate II (dysphagia to hard and solid food) – 133(62.1%), rate III (dysphagia to hard, solid and fluid food) – 21(9.8%) and rate IV (full esophageal obstruction) in 5(2.3%) patients. In 104(48.6%) cases the diagnosis was identified at policlinic, in 37(17.3%) patients - at other medical institutions and in 73(34.1%) - at our Centre. Subject to the methods of preoperational preparation, postoperative management, performing limphodissection and the types of esophageal anastomosis formation 214 patients were randomized to 2 groups. There were 74 patients in the control group who were under the treatment at our Centre between 1991 and 2000. Traditional methods of preoperational preparation, abdominal limphodissection in D-I range, traditional types of esophageal anastomosis formation and standard methods of postoperative patients management were used in this group. 140 patients having been treated from 2001 to 2015 were included to the main group. The patients of this group were performed advanced methods of esophageal anastomosis formation, two-region limphodissection in D-2, D-3 ranges keeping all principles of radicalism and ablastics. Besides, a special preoperational preparation and postoperative patients management directed to the reduce of cardiovascular and bronchopulmonary complications were introduced. On the base of complex examination of patients the following localization and stage of esophageal tumors were detected (Table 3). Table 3. Randomizing of patients subject to the tumors localization
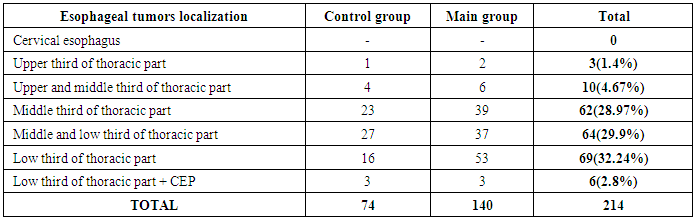 |
| |
|
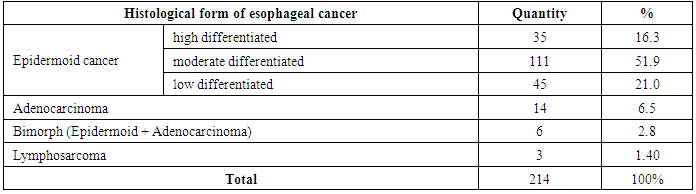
The following types of esophageal cancer were detected on the base of histological investigation (Table 4).Table 4. Types of esophageal cancer
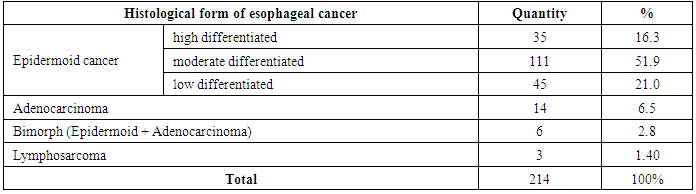 |
| |
|
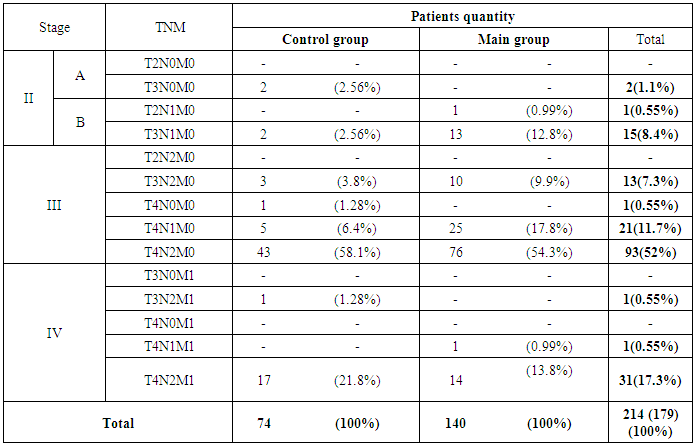
As it is seen from Table 4 the vast majority of patients was with epidermoid esophageal cancer – 191(89.2%) – of varied differentiation rate: high differentiated – in 35 (16.3%), moderate differentiated – in 111 (51.9%) and low differentiated – in 45 (21.0%). Adenocarcinoma was detected in 14 (6.5%), bimorph cancer – in 6 (2.8%), lymphosarcoma – in 3(1.4%) patients.So, esophageal cancer of various histological forms was diagnosed in 21 patients of control and main groups, the randomization of them according to ТNМ classification has been presented in Table 5. Table 5. Randomizing of patients with esophageal cancer by TNM system
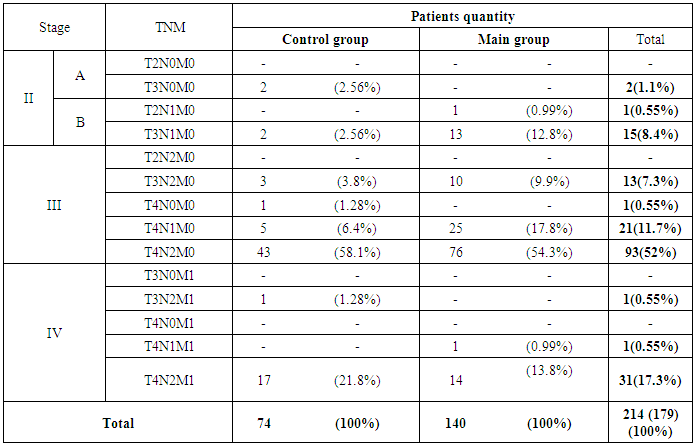 |
| |
|
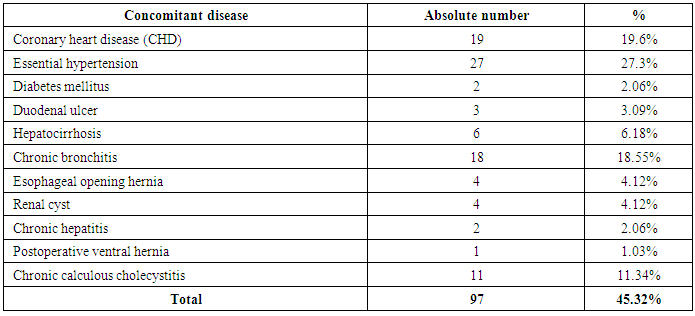
As it can be seen from Table 5 there were no patients with the stage I in our observations, but there were 18 (8.4%) cases with the stage II. This observation demonstrates extremely low early diagnostics of esophageal cancer and it is the main unfavorable success factor of any surgical treatment in patients with esophageal tumors. The majority of patients admitted with stage III – 128 (71.5%) and with stage IV – 33 (18.4%) when the surgery result was the worst from the prognostic point of view. The character of concomitant disease in the patients with esophageal cancer has been presented in Table 6. In 45.32% patients we have revealed various concomitant pathologies with different characters. We often observed 1 and more concomitant diseases in one patient. Table 6. The character of concomitant disease
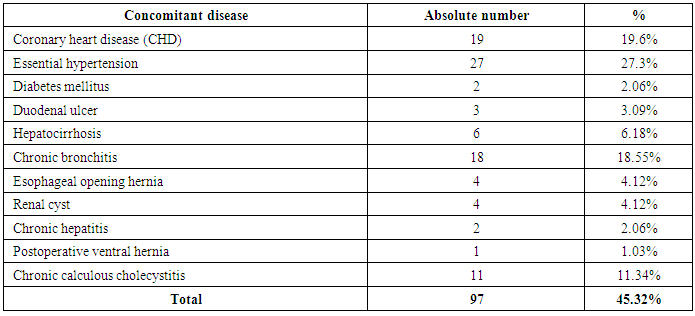 |
| |
|
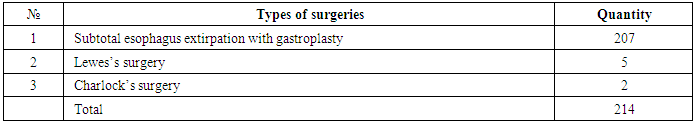
The presence of concomitant diseases affected to the character and duration of the preoperative preparation as well as to the volume of surgery. For example, the presence of chronic calculous cholecystitis meant a performing simultaneous intervention – cholecystectomy which was carried out in 11 patients. Cardiovascular diseases were also often revealed: CHD in 19(19.6%), essential hypertension in 27(27.3%) cases. According to the character of performed operative interventions the patients were randomized as follows (Table 7): Table 7. The character of performed surgeries
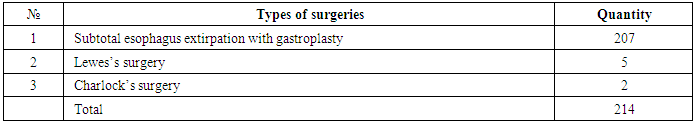 |
| |
|
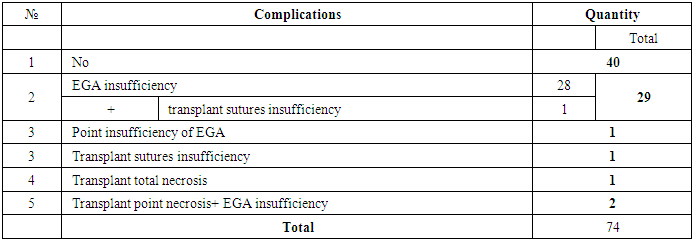
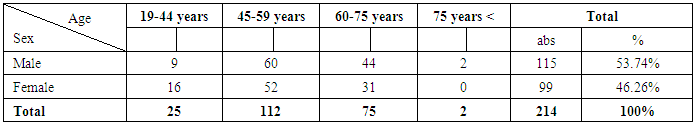
In 207 patients we performed esophagus extirpation with simultaneous esophagogastroplasty (among them abdominal-cervical approach was used in 165 patients and in 42 cases – we used thoraco-abdomino-cervical approach). Subject to the types of extra-cavitary esophageal anastomosis formation patients were divided in: control group (CG) – 74 patients in who we used traditional types of esophageal anastomosis; main group (MG) – 140 patients who were performed a developed new type of esophagogastroanastomosis (Table 8).Table 8. Specific complications after restorative surgeries in the control group of patients
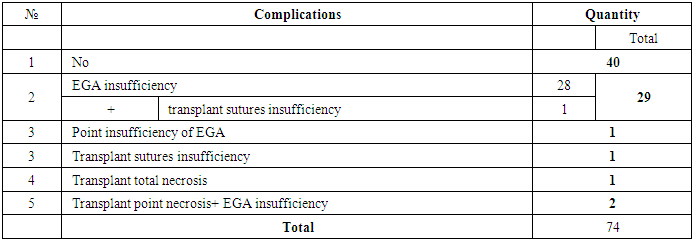 |
| |
|
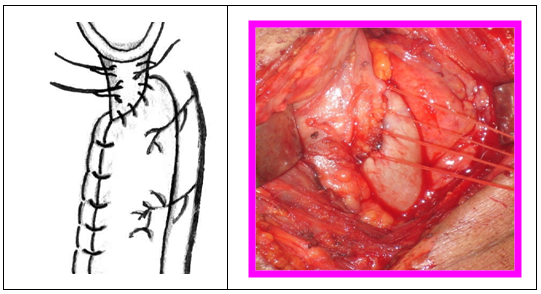
So, specific complications after esophagoplasty were developed in 40(54.0%) patients of the control group. We revealed 4 most frequent technical mistakes at anastomosis formation based on our own experience and literary data:1. Transplant blood supply abnormality; 2. Inadequacy of esophageal stump diameter and transplant;3. Excess mobilization of anastomosed organs;4. Sutures tension in the anastomosis area.A new method of “cross-skewed” esophagogastric anastomosis formation was developed and introduced at the department of esophagus and stomach surgery in 2001. An idea for creating this type of anastomosis was the fact that esophageal stump’s diameter was always less than transplant and it led to undesirable corrugating of anastomosis line with disturbance of anastomosed organs blood supply. So, anterior-left esophagus wall is dissected up in cross-skewed direction to 2-3 cm, esophageal stump’s diameter becomes close to the size of gastrotransplant proximal part with minimal mobilization of esophageal stump’s right wall (Fig.1).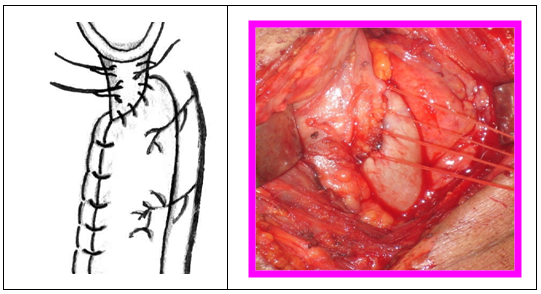 | Figure 1. The scheme of cross-skewed esophagogastroanastomosis formation |
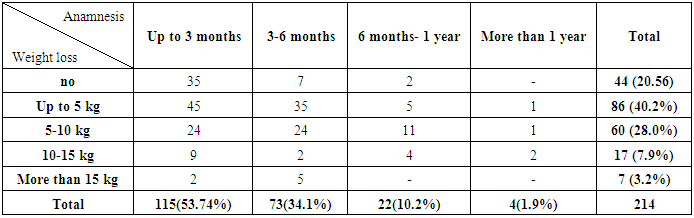
Cross-skewed esophagogastroanastomosis has got a number of advantages: 1. A wide area of formation; 2. Adequacy to the diameter of anastomosed organs – eliminates the anastomosis corrugating; 3. The anastomosis line is not situated in one area – this fact reduces the possibility of esophageal anastomosis sutures tension; 4. Minimal mobilization of esophagus right wall keeps its blood supply and improves micro-circulation of anastomosis area. Cross-skewed esophagogastroanastomosis was formed in 133 patients of the main group. The analysis of traditional and cross-slewed esophageal anastomosis is presented in Table 10. Specific complications of esophagoplasty are as follows: esophageal anastomosis insufficiency, terminal or total necrosis of esophagotransplant, its proximal part’s sutures insufficiency which leads to anastomosis insufficiency which has a secondary character. On the base of Table 10 data we can see the reduce of all specific complications quantity: - esophageal anastomosis insufficiency has reduced from 36.5% to13.5%;- transplant necrosis has reduced from 5.4% to 0.7%;- insufficiency of gastrotransplant proximal part has reduced from 1.3% to 0%.Table 9. Types of esophageal anastomosis and specific complications
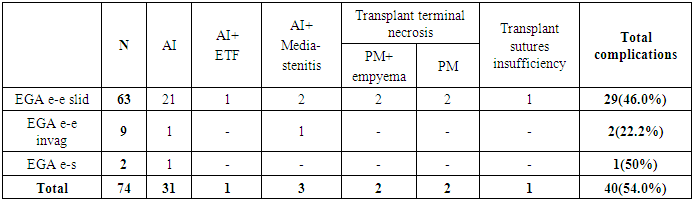 |
| |
|
Table 10. Comparative estimation of specific complications at esophagoplasty
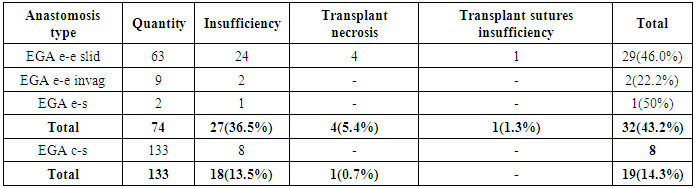 |
| |
|
3. Conclusions
A comparative analysis of esophagoplasty direct results showed that the introduction of cross-skewed EGA significantly had reduced the quantity of specific complications (insufficiency, transplant necrosis) from 43.2% to 14.3%.
Abbreviations
CG – control groupTNGT – terminal necrosis of gastrotransplant MG – main group ARF – acute respiratory failure AMI – acute myocardial infarctionET – esophagus tumors ACC – acute cardiovascular collapse EA – esophageal anastomosis EGA – esophagogastroanastomosis EE – esophagus extirpationAI- anastomosis insufficiency ETF– esophageal-tracheal fistula PM – purulent mediastenitisCEP – cardioesophageal pass EGA e-e slid – esophagogastroanastomosis end-to-end by sliding sutures EGA e-e invag - esophagogastroanastomosis end-to-end invaginated EGA e-s – esophagogastroanastomosis end-side EGA c-s – esophagogastroanastomosis cross-skewed
References
| [1] | Davidov M.I., Aksel E.M., 2011. «Statistics of malignant neoplasms in Russia and CIS countries in 2009» VESTNIK of RORC named after N.N. Blokhin. Vol. 22, №3 (85), appendix 1. July — September 2011. |
| [2] | Stillidi I.S., Ter-Ovanesov M.D. Oncology. Manual of practitioner. / I.V. Poddubnaya –М.: Medpress-Inform, 2009. |
| [3] | Chernousov A.F. «Clinical surgery: national guidance» GeotarMedia. 2010. |
| [4] | Chernousov A.F., Bogopolskiy P.M., Kurbanov F.S. П.М. – in book: «Surgery of esophagus». - М.: Medicine, 2000. |
| [5] | Belousov E.V., Baytinger V.F. The reasons of esophageal-intestinal anastomosis on the neck // Surgery.- 2012.- №10. |
| [6] | Plaksin S.A., Sablin E.E., Artmeladze R.A., Shetkina I.N. Esophagoplasty results after different types of anastomosis. //The 1st International conference on thoraco-abdominal surgery devoted to the 100th anniversary of acad. B.V. Petrovskiy. Moscow, June 5-6, 2008. Book of abstracts. p.229. |
| [7] | Fokeev Sergey Dmitrievich. Abstract of a thesis. Oncology. Barnaul 2004. |
| [8] | Braghetto M.I., Cardemil H.G., Mandiola B.C., Masia L.G., Gattini S.F. «Impact of minimally invasive surgery in the treatment of esophageal cancer» Arq Bras Cir Dig. 2014 Nov-Dec; 27(4): 237-42. doi: 10.1590/S0102-67202014000400003. |
| [9] | Heitmiller R. F., McQuone S. J., Eisele D. W. The Utility Of The Pectoralis Myocutaneous Flap In The Management Of Select Cervical Esophageal Anastomotic Complications // J. Thorac. Cardiovasc. Surg. –2014. – Vol. 115. – P. 1250-1254. |
| [10] | Thrift A.P., “Esophageal adenocarcinoma: the influence of medications used to treat comorbidities on cancer prognosis”. ClinGastroenterolHepatol. 2015 Mar 30. pii: S1542-3565(15)00362-6. doi: 10.1016/j.cgh.2015.03.028. |
| [11] | Heitmiller R. F., McQuone S. J., Eisele D. W. The Utility Of The Pectoralis Myocutaneous Flap In The Management Of Select Cervical Esophageal Anastomotic Complications // J. Thorac. Cardiovasc. Surg. –2014. – Vol. 115. – P. 1250-1254. |
| [12] | Trevellin E., Scarpa M., Carraro A., Lunardi F., Kotsafti A., Porzionato A., Saadeh L., Cagol M., Alfieri R., Tedeschi U., Calabrese F., Castoro C.,Vettor R. Esophageal adenocarcinoma and obesity: peritumoral adipose tissue plays a role in lymph node invasion. Oncotarget. 2015 Mar 14. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML