-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2018; 8(6): 108-111
doi:10.5923/j.ajmms.20180806.02

The Basic Principles of Polytrauma Patients’ Care at the Stages of Traumatic Disease
Xadjibaev A. M., Xakimov R. N., Ubaydullaev B. S.
Republican Research Center for Emergency Medicine, Tashkent, Uzbekistan
Correspondence to: Xadjibaev A. M., Republican Research Center for Emergency Medicine, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

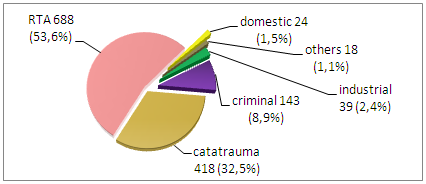
Aim of study: To describe the basic principles of polytrauma patients’ care at the stages of traumatic disease. Materials and methods: An analysis of the treatment of fractures of 1285 patients with combined and multiple musculoskeletal injuries for the period from 2012 to 2017 was carried out. The studied population consisted of men - 874 (68%) and women - 411 (32%). The average age of patients was 42.7. The number of road accidents prevailed (53.6%) over catatrauma (32.5%). Results: In order to follow damage control low invasive osteosynthesis techniques have been preferred. Such methods provided reliable bony fragments stabilization with the possibility of avoiding additional external fixation. At the same time early range of motion exercises had been allowed. In order to prevent traumatic disease reposition and osteosynthesis had been performed as soon as it was possible. The osteosynthesis for the medial femoral neck fractures was rational only in the acute period of trauma. Conclusions: When correcting the lesions of bone structures in victims with polytrauma, operational benefits differ little from those in isolated trauma.
Keywords: Polytrauma, Traumatic illness, Fractures, Surgical treatment
Cite this paper: Xadjibaev A. M., Xakimov R. N., Ubaydullaev B. S., The Basic Principles of Polytrauma Patients’ Care at the Stages of Traumatic Disease, American Journal of Medicine and Medical Sciences, Vol. 8 No. 6, 2018, pp. 108-111. doi: 10.5923/j.ajmms.20180806.02.
1. Introduction
- Treatment of patients with polytrauma is a complex and still unsolved problem. Mortality in polytrauma in both developing and developed countries of the world remains at a very high level, but in many respects its outcomes depend on the timeliness and adequacy of the applied therapeutic and prophylactic measures. Multiple and combined injuries of the musculoskeletal system in traumatological hospitals are found in 16-25% of cases [1, 2, 4, 6, 7].Studies have shown that fractures of limb bones in the structure of polytrauma range from 20 to 70%. Surgical tactics for treating bone lesions are associated with the features of the periods and the severity of traumatic disease (TD) [2-8].The aim of the study is to detail the traumatological benefit for fractures in victims with polytrauma at various periods of traumatic disease.
2. Material and Methods
- For the period of 6 years, the treatment of fractures of 1,285 patients with combined injuries of the musculoskeletal system was studied. The analysis of such a large group of patients made it possible to improve the diagnosis and surgical tactics of combined injuries. Men - 874 (68%), women - 411 (32%). The average age of patients was 42.7. The prevailing dominance was associated with road traffic accidence (RTA) (53.6%) and catatrauma (falling from the height) (32.5%).
3. Results and Discussion
- In acute and early stages of TD, assessment of the severity of the combined lesion was the main criterion for the adequacy of the treatment program and the volume of the trauma benefit was very important. The early period of TD contributed to the development of fat embolism, which in the late period contributed to the occurrence of respiratory complications, due to adult respiratory distress syndrome (ARDS). The late period is the time of planned surgical interventions, primarily of the skeletal system, when the natural regenerative capacities of the tissues are not completely lost. Immediately before the surgery and in the first 24-48 hours the prevention of fat embolism was performed. Further, such drug therapy was carried out not only by indications but also by purposeful prevention of embolic complications [4-8].Reposition and osteosynthesis in case of lesions of bone structures, if the patient's general condition allowed, was performed before the onset of toxicosis or was postponed to the end of the early or late period of TD [4, 8-10]. The exception was the medial fractures of the femoral neck, in which it is rational to perform osteosynthesis only in an acute period. It is impractical to postpone such intervention to later terms because of probable aseptic necrosis of the femoral head, since the cervix does not have a periosteum and the head is practically subjected to aseptic necrosis.Pins fixation for the femoral neck fractures have now gone down in history. Usually, osteosynthesis was performed with 2 or 3 lag screws.In case of fractures of the clavicle we used intraosseous fixation with Kirshner pins or open reduction and internal fixation with limited contact semi-tubular plate. Modern clavicle fixators allowed to conduct the postoperative period before the fusion of fragments without external immobilization, and movements in the shoulder joint start from 2-3 days.Multifragmental fractures of the shoulder head were difficult to reposition and fixation. The problem was solved by using plates with angular stability – the screws head had been locked in plate. An alternative method was a low-traumatic internal nailing without exposing the site of the fracture, but with the locking of the nail under C-Arm control. External fixation was not usually required. Complex intraarticular fractures of the distal part of the shoulder remained a serious problem in restoring the function of the elbow joint. Progress in this direction appeared with the use of a back access with a temporary cut of the olecranon, which provided exposure of the posterolateral distal parts of the shoulder with the possibility of intraoperative visual control at the time of fragments fixation. External immobilization was usually required in case of doubtful fragility stability before their adhesion or for a short period of time, so as to eliminate the pain syndrome. Fractures of the bones of the forearm, hands and fingers did not pose a serious threat to the lives of victims, so in the acute and early periods, TD was usually limited to conservative benefits or immobilized in any way. At the primary surgical treatment, the tissues were most spared. Reconstructive interventions were postponed for a late period and a period of rehabilitation.A special approach was followed in the surgical treatment of unstable fractures of the pelvis [3, 9, 10]. In surgical intervention, there was a tendency for an ideal or close reposition of fragments with reliable fixation of cortical, lag and compression screws by the plates. But this concept was followed in a deferred order. In the early period of TD, we used external fixation devices (EFD) for pelvic fractures developed in our clinic. The EFD imposed for urgent indications was used not only for the purpose of temporary re-establishment of fragments of the pelvis, but also to ensure their stabilization. However, quite often such interference proved to be quite adequate or only a perimeter installation was necessary. After the repositioning of the posterior half-ring of the pelvis (iliac bone, sacrum, sacroiliac joint, fixation of the fragments was possible with screws and plates). Fractures of the anterior half-ring, symphysis rupture, fractures of lobes and sciatic bones, including butterfly type, were fixed with plates.Quite a difficult situation occurred with fractures or a broken acetabulum, especially in combination with hip dislocations. Detailing the nature and extent of damage in the preoperative period was necessary in the planning of surgical intervention, which was assisted by a multiple computer tomography scan. The central dislocation of the femur was previously eliminated by stretching or intraoperatively on the orthopedic table. For stable stretching, we used the EFD "pelvis hip" developed in our clinic.The advantage of this device is a closed method of repositioning bone fragments and early activation of patients. with complex fractures and pronounced mixing of the bone fragments of the cavity, its bottom, columns and roof after repositioning were fixed with reconstruction plates, simulating them intraoperatively, or by special plates, allowing simultaneous fixation of the posterior half ring, acetabulum and even the anterior parts of the pelvis. With a broken depression, we tried to orient bone tissues in the region of the cavity so that in the future, usually during the rehabilitation period with hip arthroplasty, to be able to restore the supporting function of the thigh with special rings.Intraarticular fractures of the proximal femur, if not operated in an acute period, were surgically treated during the rehabilitation period. The method of choice often became total hip arthroplasty. Vertical, and sometimes basal, fractures of the femoral neck were synthesized by dynamic femoral structures or L-shaped plates (Picture 1).
 | Picture 1 |
4. Conclusions
- It was found that in correcting damage to bone structures in victims with polytrauma, operational benefits differ little from those in isolated trauma. However, definitely, low-traumatic interventions from mini-accesses, with the most limited blood loss, which provide reliable operational stabilization of fragments with the possibility of avoiding additional external fixation and allow early initiation of functional treatment are preferred1. Treatment of patients with polytrauma should be based on the tactic "Damage Control" (damage on the control and surgical interventions are carried out on a priority basis - stop bleeding and restore the integrity of hollow organs, brain decompression, stabilization of fractures).2. Early stable fixation of broken bones in patients with polytrauma, reducing the afferent impulsation has antishock action, increases the mobility of patients, facilitates the care of them, reduces the number of hypostatic complications, which ultimately increases the percentage of recovered.3. The main requirements for osteosynthesis in the treatment of victims with polytrauma are: 1) reliable immobilization of bone fragments; 2) minimal invasiveness; 3) low traumatism; 4) short time of surgical intervention.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML