-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2018; 8(5): 96-98
doi:10.5923/j.ajmms.20180805.02

The Use of Mini-Invasive Correction Methods for Iatrogenic Injuries of Extrahepatic Bile Ducts and External Biliary Fistula
F. G. Nazirov, U. N. Turakulov, M. M. Akbarov, R. R. Saatov
Republican Specialized Research Centre of Surgery Named after Academician V. Vakhidov, Tashkent Institute of Post-Educational Doctors, Tashkent, Uzbekistan
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The causes of cicatrical strictures and fistulas, by our observations, were as follows: bile ducts injuries and their inadequate drainage at cholecystectomy (9.2%), stomach resection (7.0%) and at echinococcectomy (2.8%). We have performed 47 endoscopic transduodenal stentings of extrahepatic bile ductsstenotic areas after primary surgical interventions. In all the cases we have found strictures of hepaticoholedoch which formed external biliary fisula. It has been managed to restore the patency of the hepaticoholedoch lumen and to perform the stenting of stenotic segment – it led to patients’ recovery and their discharge after 6-8 days. All the patients were under the permanent control in the post-operative period. There were no complication cases connected with the stenting of the external bile ducts. The stents were extracted in different periods while performing duodenoscopy (from 6 to 10 months). Thus, the methods of endobiliary stenting are one of the main methods for correctioniatrogenic injuries of extrahepatic bile ducts and external biliary fistula. They frequently prevents the patients from severe and sometimes repeated operative interventions.
Keywords: Iatrogenic injury, Bile ducts, Stent, External biliary fistula, Cicatrical stricture
Cite this paper: F. G. Nazirov, U. N. Turakulov, M. M. Akbarov, R. R. Saatov, The Use of Mini-Invasive Correction Methods for Iatrogenic Injuries of Extrahepatic Bile Ducts and External Biliary Fistula, American Journal of Medicine and Medical Sciences, Vol. 8 No. 5, 2018, pp. 96-98. doi: 10.5923/j.ajmms.20180805.02.
1. Background
- The issues of diagnostics and treatment of iatrogenic injuries of extrahepatic bile ducts (IIEBD) and external biliary fistula (EBF) are very topical in the field of abdominal surgery [1-2]. As a rule, the following complications are developed at IIEBD and EBF: the duration of clinical course, the development of chronic obstructive jaundice and biliary cirrhosis, purulent cholangitis, portal hypertension and hepatargia. Such patients have to be performed repeated surgeries. According to the data of the latest international congresses of the Association of hepatopancreatobiliary surgeons of CIS countries, the relevance of this issue has become more actual. The frequency of extrahepatic bile ducts intra-operational injuries reaches 0.2 - 3% from the general number of abdominal cavity surgeries, the recurrences of bile ducts strictures and external biliary fistulas after reconstructive interventions varies in the range of 10-12%. The lethality at these complications makes up from 8 to 40% [3-4].According to various authors data, 90% of IIEBD are observed at cholecystectomy: at performing cholecystectomy by laparotomic approach – from 0.8 до 1% and at laparoscopic methods – from 0.3 to 3% of cases [3-4]. Concerning to the laparoscopic interventions on extrahepatic bile ducts it can be judged in two ways. From one side, the adoption of laparoscopic technique is an evidence of progress in medical science and practice. From the other side – the increase of laparoscopic interventions quantity at the stage of the method’s development inevitably leads to the appearance of various complications. Iatrogenic injuries of extrahepatic bile ducts are characterized by a high complicity, they require recurrent high-tech interventions. The IIEBD after surgeries on the stomach makes up 0.4-9.1%. The origin of this complication is stipulated by the following criteria: 1. the level of the surgeon’s qualification, his skills in anatomic-topographic interrelations of extrahepatic bile ducts; 2. extensiveness of a destructive process in the gallbladder extending to the elements of hepatoduodenal ligament. The approaches to the different surgeries at such pathology are disputable and they cannot be regarded as satisfactory ones. The abilities of such a new method in the bile ducts surgery as endobiliary stenting remain little-studied.[5-6]. That is why the issue of the further enhancement of the diagnostics and surgical treatment of iatrogenic injuries of hepaticocholedoch and EBF still remain arguable. GoalTo improve surgical treatment results of iatrogenic injuries of extrahepatic bile ducts and external biliary fistula with the use of mini-invasive endoscopic technologies in the surgery.
2. Materials and Methods
- The main role in the diagnostics of intra-operative injuries, cicatricial strictures and EBF belongs to the endoscopic retrograde cholangiopancreatography (ERPCG). The ERPCG has been performed with the use of duodenofiberscope with lateral optics JF-B(B2), JF-10 by “Olimpus” (Japan). We have performed 196 ERPCG. From this amount the ERPCG with further endoscopic papillosphincterotomy (EPST) was performed in 91 patients. The control ERPCG was carried out after the EPST in 44 cases. The bouginage of the stenotic segment by bioptic forceps in the open and closed types in combination with local diathermo-coagulation of hardly dilated cicatricial segment has been carried out. Then we performed the stenting of the stenotic area with the use of standard endobiliary stents. Inclusion criteria:1. Patients with iatrogenic strictures of extrahepatic bile ducts.2. Patients with the stricture of papilla duodeni major.3. Patients with external biliary fistulas.4. Patients with a combination of hepaticoholedoch stricture and external biliary fistula.Exclusion criteria:1. Patients with high stricture of hepaticoholedoch who were performed percutaneous transhepatic cholangiostomy. 2. Patients who cannot be performed ERPCG due to anatomic variants and anomalies. 3. Patients who initially were planned to be performed radical reconstructive interventions.
3. Results and Discussion
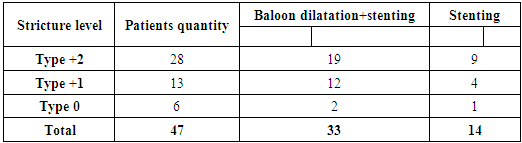
- The causes of cicatricial strictures and fistulas formation by our observations were: bile ducts injuries and their inadequate drainage at cholecystectomy (9.2%), the stomach resection (7.0%) and at echinococcectomy (2.8%).We have performed 47 endoscopic transduodenal stentings of the extrahepatic bile ducts stenotic areas after primary surgical interventions (Table 1). In all the cases we have found strictures of hepaticoholedoch which formed external biliary fisula. In 6 cases the stricture was located in the confluence zone and it was critical as it provoked the progressing of obstructive jaundice. Conjugated bilirubin in this patients group was from 200 to 300 mcmol/l. The initial signs of hepatic failure as encephalopathy manifestation, a reduction of albumin level below than 30 g\l, prothrombin index below than 82% were observed in 1 patient. In 13 cases the obstacle was located in the fusion area of cystic duct with common bile duct. In 17 cases the obstacle of bile outflow was located in the distal part of the choledoch. Conjugated bilirubin in those patients was from 300 to 390 mcmol/l.
|
4. Conclusions
- Thereby, the causes of intra-operative injuries, cicatricial strictures and external biliary fistulas are tactical and rough technical mistakes at performing primary interventions (more often at carrying out cholecystectomy). The methods of endobiliary stenting are one of the main methods for correction iatrogenic injuries of extrahepatic bile ducts and external biliary fistula. They frequently prevents the patients from severe and sometimes repeated operative interventions.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML