-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2018; 8(4): 66-70
doi:10.5923/j.ajmms.20180804.03

Modified Stone Benson’s Perineal Proctoplastics in Low Forms of Anorectal Malformation in Children
TT Narbaev, UX Tilavov, NN Turaeva, BA Terebaev, MS Chuliev, MM Nasirov
Department of Pediatric Surgery, Tashkent Pediatric Medical Institute, Uzbekistan
Correspondence to: MM Nasirov, Department of Pediatric Surgery, Tashkent Pediatric Medical Institute, Uzbekistan.
| Email: |  |
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

After Stone-Benson’s operation in early period 18,9% complications were occurred, after perineal proctoplasty by modification of TashPMI clinic (patent # IAP04799 17.12.2013y.) – 9,5%. In long-term period after Stone-Benson’s operations complications occurred in 22,8% of cases, after perineal proctoplasty by modification of TashPMI clinic – 12,3%. In recommended method of perineal proctoplasty by modification of TashPMI clinic successful results were noticed.
Keywords: Anorectal malformations, Stone-Benson’s operation modification, Perineal proctoplasty, Early and long-term results
Cite this paper: TT Narbaev, UX Tilavov, NN Turaeva, BA Terebaev, MS Chuliev, MM Nasirov, Modified Stone Benson’s Perineal Proctoplastics in Low Forms of Anorectal Malformation in Children, American Journal of Medicine and Medical Sciences, Vol. 8 No. 4, 2018, pp. 66-70. doi: 10.5923/j.ajmms.20180804.03.
1. Introduction
- The problem of surgical correction of anorectal anomalies remains relevant. Despite some successes in this field [2, 3, 6, 13, 15] there is no method that would provide reliable anatomical and functional results providing social adaptation of patients, many of whom remain severely disabled. Studies aimed to improve the tactics and methods of treatment of anorectal pathology in childhood are continuing.The methods proposed by A. Rena, Rizoli, termed posterosagittal anorectoplasty (PSARP) and anteroposterior perineal proctosanosphincteroplasty (APPSP), widely implemented by the authors and their followers [1, 7, 11, 12] find application practically in all types of anorectal anomalies. However, with the collecting experience, certain negatives of these techniques have also emerged, which requiring to search for new, more sophisticated and less traumatic methods of correcting ARM.H. Stone (1936) in the modification of Benson (1949) proposed perineal proctoplasty, which was designed to maintain the integrity of the external sphincter. A horseshoe-shaped incision was made between the vestibule of the vagina and the proposed place of the anus. After dissection of soft tissues, the rectum was isolated to such an extent that it could be moved without tension. A second incision was then made according to the location of the putative anus, and mobilized gut was moved into the outer sphincter ring, with two rows of sutures applied to the perineal tissues.The disadvantages of the Stone-Benson operation were:- Insufficient vision in the narrow and deep wound of the fissure, which made it difficult to isolate the walls of the rectum - often the wall of the rectum and vagina was damaged in the allocation of the latter;- the inability to form an adequate rectal obturation;- recurrence of fistula in the reproductive system, secondary ectopia of the newly formed anal opening anteriorly (towards the vaginal vestibule);- formation of the tunnel for pull-through was performed "blindly", so the gut was often pulled-through outside the sphincter apparatus- impairing of aseptic seam lines with intestinal contents and retraction of the stump of the rectum with the formation of rough scars on the perineum. (Sulaimanov AS 1983, Heinen FL 1997, Shchitinin VE, Povarnin O. Ya. and others 2001, Holschneider A. M. 2006).
2. Material and Methods
- The article presents the collected experience of treating 150 patients with low forms of anorectal malformations. Observations cover the period from 1995 to 2015. The age of children ranged from 3 months up to 14 years. Of these, the overwhelming majority of 122 were girls, 28 boys.Of the 122 girls, primary perineal proctoplasty was performed in 105, ventral-perineal - in 17.As a result of examination of patients, a low form of anorectal malformation like atresia of the anus with recto-vestibular fistula was noted in 92 patients, in 13 patients with recto-fissure fistula. 58 patients underwent Stone-Benson's operation, 47 patients with perineal proctoplasty (PPP) in the modification of our clinic (patent No. IAP04799 dated December 17, 2013).Preoperative preparation included slag-free diet (5-7 days before surgery), cleansing of the distal intestine with enemas, elimination of intestinal intoxication, metabolite therapy and stabilization of the homeostasis system.All children, along with general clinical methods of examination underwent: fistulourigography, intravenous pyelography, cystography, perineal ultrasound (pelvis), sphincterometry, measurement of pressure in the ampulla of the rectum, morphological studies of the distal parts of the rectum and sphincter apparatus.In 67 (40%) patients, concomitant anomalies were found, among which the developmental defects of the genitourinary system prevailed (27%).The modified version of the Stone-Benson operation is most suitable for cases of atresia of the anus with rectovestibular fistula in girls (Fig. 1).A small oval incision of the skin was made at the place of the proposed anus at the level of the established label. Further, the needle electrode of the monocauter with a current intensity of 0.1-0.2 mA refined the topic of the external sphincter and its inner ring. At the center of the contracted muscular ring-sphincter with the help of a direct clamp, the muscle fibers were bluntly moved apart, trying not to damage them. Blunt dissector was injected inside the fistula to a depth of 0.5-0.6 cm, then, pressing on the back wall of the fistulous duct, seized it on the turnstile (Fig. 2).After subcutaneous cutting of the fistulous duct, the front wall of the lowered intestine was initially mobilized, separating it from the back wall of the vagina. This manipulation, which is different from the classical perineal proctoplastic methods, when the posterior wall of the gut is initially mobilized, allows the morphologically mature blind end of the atresized intestine to efficiently skeletonize to the level of the posterior Douglas space.Later, easier and less mobilization of the posterior wall of the intestine ensured the preservation of the main component of the sphincter apparatus of the loop of the puborectal muscle and less smoothing of the recto-anal angle. The latter largely reduced incontinence in the postoperative period. Controlling the safety of the back wall of the vagina, bluntly separated the back wall of the rectum from surrounding tissues to visualization of the m.puborectalis loop.Excision of the fistulous duct was performed at the level of subcutaneous layer. After the separation of the posterior wall of the rectum from the surrounding tissues, it was started retrograde bluntly by separating the anterior wall of the rectum from the posterior wall of the vagina to the posterior arch. Further, subcutaneously, excised the anterior wall of the fistulous duct (Fig. 3).After mobilization of the intestinal wall, usually to a depth of 5-7 cm, it was fixed with 4-5 nodal sutures to the muscles of the sphincter and to the skin leaving a loose hanging stump 2-3 cm (Fig. 4). At the same time, a slight tension is permissible and even desirable, due to which the edge of the previously mobilized skin is drawn into the anal fossa, which provides a good cosmetic effect. In the lumen of the lowered intestine an intestinal tube was left. The bladder was catheterized. Clipping of the stump and anoplasty was performed in the second stage after 12-14 days. (Fig. 5). The abandonment of the free-hanging stump had the advantage, mainly, in the formation of a seamless anastomosis and prevention of divergence of the edges of the wound and subsequent scarring of the anus. After 1 year after the operation, it was possible to obtain not only a satisfactory functional result, but also an aesthetic appearance of the perineum (Fig. 6).
 | Figure 1. Patient P. 6 months. Ds: Anal atresia with rectovestibular fistula. Before surgery |
 | Figure 2. After the dissection of the posterior wall of the fistulous duct, the front wall is mobilized. The clamp inserted through the fistula is projected in the lumen of the rectum |
 | Figure 3. After separation of the anterior and posterior walls of the intestine. Tension free stump up to 3cm |
 | Figure 4. One nodal suture is applied to the skin of the fistula. The pulled-though stump is fixed to the perineal skin by nodal sutures. An intestinal tube is left in the lumen |
 | Figure 5. Condition after stage 2 of surgery - excision of stump (2 days after surgery) |
 | Figure 6. Status of the perineum and anus in 1 year after the operation. The anal canal is covered with a retracted protoderm and the normal appearance of the perineum remains |
3. Results and Discussion
- In patients operated by Stone-Benson’s method, we noted in the early postoperative period neoanus deficiency, which is inherent in all patients, constipation, dystopia and neoanus disposition outside the anal pulp with partial or complete destruction of the latter. All this in the long-term postoperative period was usually layered with scar deformation, prolapse of the mucous membrane, etc. Sometimes, several mutually related consequential complications were observed in the same patient.The frequency and nature of complications of the nearest postoperative period, depending on the type of perineal proctoplasty, are presented in Table 1.
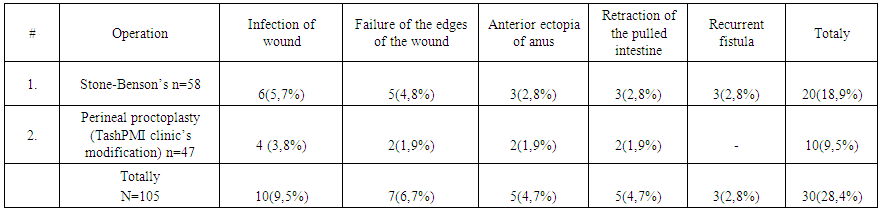 | Table 1. Complications of the nearest postoperative period |
 | Table 2. Complications of the long-term postoperative period |
4. Conclusions
- Based on the results of the research, a number of advantages of using the proposed modification of the perineal proctoplasty comparing with Stone-Benson’s operation were noted:- Integrity of the perineum with its innervation is maintained. This contributes to the obtaining of good cosmetic and functional results.- As a result of the retrograde separation of the anterior wall and the excision of the fistula from the inside, a defect of the size of the fistula is formed on the fistula's anus, which prevents deformation and the presence of a scar on the side of the vagina.- Infection of the wound was not observed, which was achieved by the removal of fecal matter by a distance, as a result of leaving the free hanging intestinal stump with a preserved muscular wall and excising it after the formation of a seamless anastomosis.- The preservation of the integrity of the perineum, the muscular structures of both the sphincter and the puborectal loop prevented the shift of the newly formed anus anterior to the vestige of the vagina, and also eliminated the possibility of recurrence of the fistula in the reproductive system.As a result, the creation of an adequately functioning barrier device, the prevention of stool incontinence and the normal restoration of the appearance of the perineum promotes adequate social adaptation of children and an improvement in the quality of life.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML