-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2018; 8(2): 31-36
doi:10.5923/j.ajmms.20180802.03

The Probability of Applying Splenosuprarenal Anastomosis Subject to Angio-architectonics of Lineal and Left Renal Basin Vessels
F. G. Nazirov, A. V. Devyatov, A. Kh. Babadjanov, S. A. Sultanov, L. L. Mardonov
«Republican Specialized Research Centre of Surgery named after Academician V. Vakhidov» State Unitary Enterprise, Tashkent, Uzbekistan
Copyright © 2018 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Investigation results of 189 patients with portal hypertension have been carried out. All patients were performed a portosystemic shunting: splenosuprarenal anastomosis – in 123 patients; Н-shaped splenorenal anastomosis with an insert from internal jugular vein to the right – in 66 patients. The variants of splenic and the left renal veins anatomy at portal hypertension (PH) have been analyzed. A histologic structure of porto-caval basin’s vessels certain parts in patients with PH has been studied. The efficiency of splenorenal anastomosis with the use of the left renal vein flow for the prophylaxis of esophageal varices hemorrhage and the post-shunting complications in the nearest and long-term periods has been assessed.
Keywords: Liver cirrhosis, Portal hypertension, Esophageal varices, Splenorenal anastomosis
Cite this paper: F. G. Nazirov, A. V. Devyatov, A. Kh. Babadjanov, S. A. Sultanov, L. L. Mardonov, The Probability of Applying Splenosuprarenal Anastomosis Subject to Angio-architectonics of Lineal and Left Renal Basin Vessels, American Journal of Medicine and Medical Sciences, Vol. 8 No. 2, 2018, pp. 31-36. doi: 10.5923/j.ajmms.20180802.03.
1. Background
- At present, the only method which significantly improves a prognosis of patients with liver cirrhosis (LC) and portal hypertension (PH) is the liver transplantation. But it is not available to the overwhelming majority of patients due to the deficiency of donor organ, a high cost and technical complicacy and also due to the imperfection of a legislative base in the field of transplantology [1-4].In this connection, a portosystemic shunting (PSS) in the modern surgery of PH remains as one of the priority lines of prophylaxis against variceal hemorrhage. But in patients with LC a decompressive effect of shunting surgeries promotes not only the portal pressure dropping but also a forming of hepatofugal portal blood flow against the background of which the development risk of the hepatic failure and encephalopathy can reach up to 25-40% [5, 6].At present time the majority of surgical schools dealing with the issues of prophylaxis against variceal hemorrhage in patients with LC adhere to the concept of the central partial decompression which was offered by К. Johansson in 1989. This original method competing with selective types of shunting provides not only an adequate decompression of the portal system but guarantees a long-term preservation of liver portal perfusion [7-11].The occurrence of such unsatisfactory effects as thrombosis of intervascular insert, the recurrences of variceal hemorrhages, a sharp progressing of the hepatic failure, encephalopathy make to use the natural flows of the left renal vein for the forming “false H-shaped shunts”. From one side, it reduces the risk of anastomosis thrombosis (as unicameral shunt is formed), and from the other side, it does not require an additional intervention on the neck to intake venous insert from internal jugular vein. The flows of the left renal vein can be also used at the formation of anastomosis with splenic vein. But its wide use is limited by anatomic-morphologic features, technical difficulties at the applying of anastomosis conditioned by small diameter or a thin wall of vessel and also by the absence of stated indications to this type of shunting [12-16].So, it is necessary to have a complex, detailed estimation of the porto-caval basin vessels regional angio-architectonics and histologic structure with a definition of indications to the use of the left renal vein flows to apply splenorenal anastomosis.
2. Materials and Methods
- In our center splenosuprarenal anastomosis (SSRA) in the surgery of PH in patients with LC first was performed in 1992. 123 SSRA were carried out up to 2016 inclusive. As this type of shunting refers to the false “H-shaped” variants of decompression, a comparison group (66 patients) was consisted of patients with the true “H-shaped” shunting (an intake of venous insert from the right internal jugular vein for applying “H-shaped” splenorenal anastomosis (H-SRA) with a necessity of forming two cameras – a venous insert with a splenic vein and the other end of the insert with the left renal vein. The mean age of all the patients was 27.6 ± 1.1 years (SSRA) and 27.3 ± 1.6 years (H-SRA). In the majority of cases young patients and teen-agers were performed the surgery – 175 (92.6%), males were in 1.6 times more than females.The cause of PH in 166 (87.8%) cases was LC and in 23 (12.2%) patients with anhepatic form of PH – the portal vein thrombosis. An old omphalitis was the main factor of the portal vein thrombosis development.The review of LC development factor showed that 161 (85.2%) patients had HBV, HCV in the anamnesis, 2 (1.1%) patients – malaria, 15 (7.9%) – abused alcohol and 3 (1.6%) – contacted with weed and pest-killer chemicals. In the rest 8 (4.2%) patients the etiological factor was not specified, but at the survey of 6 (75%) patients we defined the markers of viral hepatitis.The following instrumental ways of investigation were performed in all patients: fibroesophagogastroscopy, hepatoscintigraphy, echography, splenoportography. We also used optical and electron microscopy for morphometric estimation of the vessels histological structure.
3. Results and Discussion
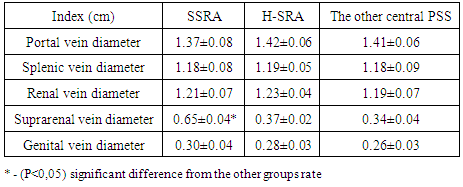
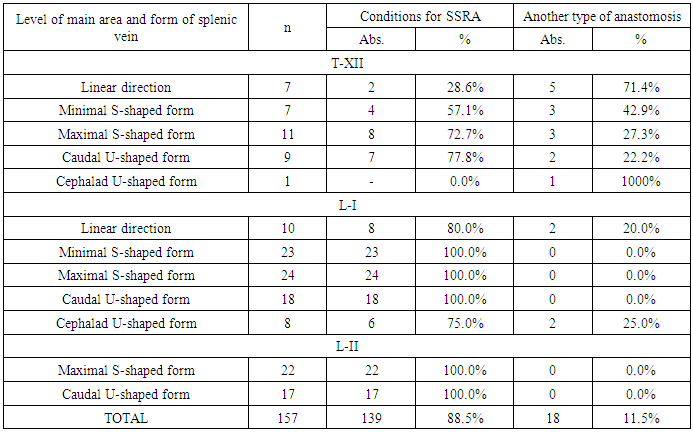
- The probability of using vein afference of the left renal vein system depends on many factors: a diameter of suprarenal flow, its wall thickness, variant anatomy of the left renal artery and transformation of the splenic vein in PH conditions – does not always create optimal conditions not only for SSRA but also for the other types of PSS.The main indications for the central decompression are portal hypertension and the old variceal hemorrhages, but the primary assessment for applying anastomosis belongs to the ultrasound investigation (USD). At the absence of contraindications from the side of hepatocytes functional status, permissible changes of blood red cells (HB higher than 80 g/l), a compensated condition of the hemostasis system and concomitant pathology – decompressive interventions are the privileged direction in the surgery of PH. But there is a small group of patients who cannot be performed PSS in the conditions of the planned surgery and that is why they are carried out surgeries which disconnect gastro-esophageal venous collector.The main cause of the PH in our country is intrahepatic block (LC) which reaches 95% in the general structure of all etiologic causes, the simple USD with dopplerography allows to assess a vascular permeability of the portal basin, veins diameter and blood flow rate, the evidence of splenomegaly syndrome and etc.Patients were randomized to 3 groups: the 1st (SSRA) and the second group (H-SRA) were compared between each other due to the similarity of decompression type; the 3rd group - with other types of anastomosis.In the condition of PH due to LC, the efficiency of USD with dopplerography on visualization of the portal basin basic veins makes up 100% and it is not complicated for the qualified specialist. The same statement can be refered to the left renal vein. But the flow system of the mentioned veins is often inaccessible for the objective assessment by USD. So, the left gastric vein is succeeded to be visualized approximately in one third of patients with PH; the flows of the left renal vein are succeeded to be assessed more often (suprarenal vein is detected in 62.3-85% of patients, genital flow – in 56.6-68.3%). The main reasons of detailed ultrasound estimation’s impossibility for the left renal vein system were splenomegaly syndrome with renal allotopia and the existence of compensatory dilated retroperitoneal vessels making difficult to identify the veins of the second order. The indices of vessels diameter between groups are presented in the Table 1.
|
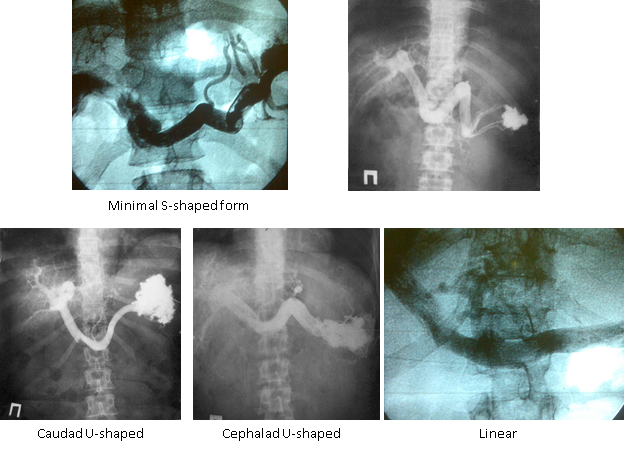 | Figure 1. SPG. The splenic vein forms |
|
|
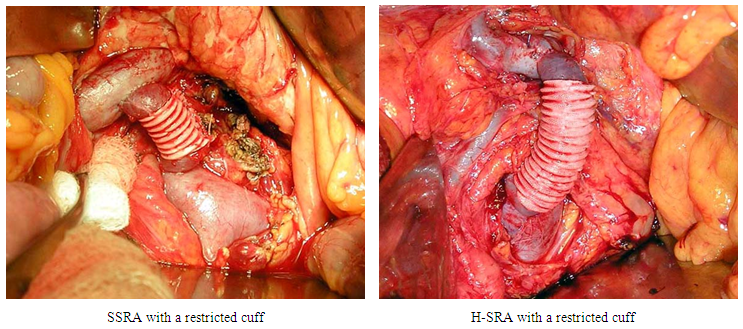 | Figure 2. H-shaped anastomosis with a restricted cuff |
4. Conclusions
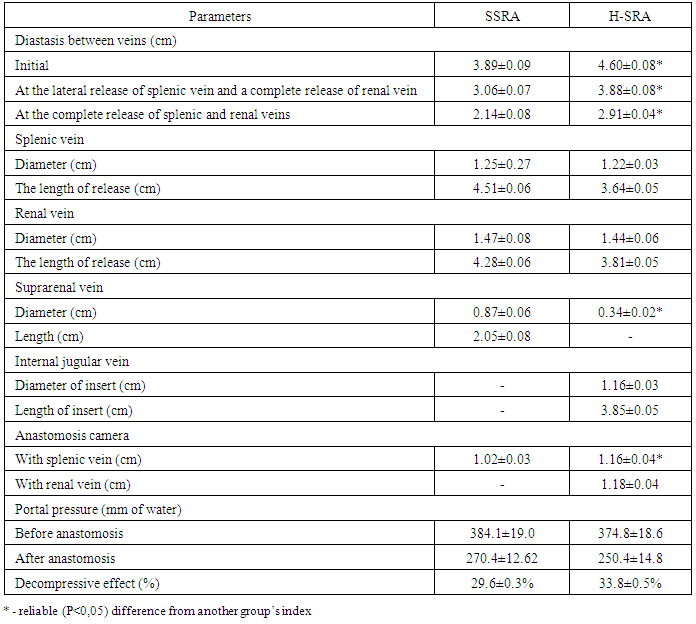
- Subject to the peculiarities of splenic vein’s angio-architectonics (the form and the level by SPG data), the optimal conditions for applying SSRA are revealed only in 60% of cases at the high location of the vessel (Т-XII) and in 95.2-100% of patients with a low variant anatomy (L-I-II). The probability of applying SSRA subject to the diameter of the suprarenal vein made up only 64.3% and the presence of a lengthy diastasis between anastomosed vessels or unfitness of the venous wall thickness reduces this index up to 47.1%. A comparative analysis of the technical levels of performing SSRA and H-SRA showed that at the use of a true venous insert the necessity in the lengthy release of the vessels made up 84.6% for the renal vein and 54.5% for the splenic vein. The release stage for SSRA is more traumatic (91.9% and 74.0%) but from the other side, the formation of H-SRA dictates the necessity of the intake of venous insert and applying of two cameras of anastomosis – it decreases the risk of thrombosis development. Decompressive effect at H-SRA makes up 33.8±0.5% and at SSRA the portal pressure decreases to 29.6±0.3% and this fact stipulates the diameter of H-insert and anastomosis camera (1.22±0.04 cm versus 1.07±0.03 cm, Р<0.05). In 60.6% of cases at H-SRA formation the necessity in the restriction of porto-caval shunt by the original method occurs in order to keep the optimal level of hepatopetal blood flow and prophylaxix of thrombosis. At SSRA only 17.9% of patients needed the restriction – it was connected both with the less length of the false H-insert and thick and dense wall of the suprarenal vein.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML