-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2018; 8(2): 25-30
doi:10.5923/j.ajmms.20180802.02

Study the Effect of Modifiable Risk Factors on Incidence and Prognostic Impact of Contrast Induced Nephropathy Post Coronary Interventions in Patients Admitted at AL-Azhar University Hospital, New Damietta, Egypt
El-Sayed El-Meghawary El-Sayed 1, Helmy Ahmed Shalaby 2, Ahmed Salama Al Adl 1, Khaled Ib. Naguib 3, Ahmed Mohammed Bayomi 1
1Internal Medicine Department, Al-Azhar University, Faculty of Medicine, New Damietta, Egypt
2Internal Medicine Department, Al-Azhar University, Faculty of Medicine, Cairo, Egypt
3Cardiology Department, Al-Azhar University, Faculty of Medicine, New Damietta, Egypt
Correspondence to: Ahmed Salama Al Adl , Internal Medicine Department, Al-Azhar University, Faculty of Medicine, New Damietta, Egypt.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Contrast-induced nephropathy (CIN) is defined as a relative (≥25%) or absolute (≥0.5 mg/dl; 44 μmol/l) increase in serum creatinine from baseline value. The aim of the work: Study the Incidence and the effect of Modifiable and non-modifiable risk factors for occurrence and prognostic impact of Contrast Induced Nephropathy post coronary interventions in patients admitted at AL-Azhar University Hospital, New Damietta, Egypt. Patients and methods: This study was conducted on 120 patients attended at the emergency unit, cardiac outpatient clinic and Internal medicine department of Al-Azhar university hospital New Damietta during the period from December 2014 and August 2015. They were presented by cardiac symptoms (chest pain, dyspnea, low cardiac output symptoms., acute coronary syndrome or chronic stable angina). They were subjected to coronary angiography and Percutaneous coronary Interventions after medical history taking, clinical examinations, and ECG findings suggestive of acute coronary syndrome, Basal serum creatinine before coronary angiography and percutaneous coronary Intervention Follow up serum creatinine 48 hours later and two weeks later, serum Na (meq/dl), serum K (meq/dl), serum uric acid (mg/dl), urine analysis, serum cholesterol, serum triglycerids, CBC, fasting and 2 hours post prandial blood glucose level, Hg A1 C. Results: 15 patients out of 120 patients developed contrast induced nephropathy (12.5%) 105 patients out of 120 patients didn’t develop contrast induced nephropathy (87.5%) so studied 120 patients divided into 2 groups: (group A) patients who developed contrast induced nephropathy (15 patients) and (group B) patients without contrast induced nephropathy (105) patients. There was a statistical significant increase of s. creatinine, follow up 48h s. creatinine after coronary interventions and follow up 2 weeks s. creatinine in group A in comparison to group B. There were statistically significant increase of D.M, HTN and congestive heart failure in group A in comparison to group B. Conclusion: Contrast nephropathy is a major cause of morbidity in patients undergoing coronary angiography or per cutaneous coronary interventions, risk factors for CIN such as diabetes mellitus, congestive heart failure, hypertension, and medications, high osmolality and high ionic content of contrast medium, large volume of contrast medium and recurrent contrast exposure all are included in increased incidence of occurrence of CIN and poor the prognosis. Proper selection of patients who undergo contrast imaging and pre-procedural preparations would be helpful to reduce the risk of CIN.
Keywords: Contrast Induced nephropathy, Acute kidney injury
Cite this paper: El-Sayed El-Meghawary El-Sayed , Helmy Ahmed Shalaby , Ahmed Salama Al Adl , Khaled Ib. Naguib , Ahmed Mohammed Bayomi , Study the Effect of Modifiable Risk Factors on Incidence and Prognostic Impact of Contrast Induced Nephropathy Post Coronary Interventions in Patients Admitted at AL-Azhar University Hospital, New Damietta, Egypt, American Journal of Medicine and Medical Sciences, Vol. 8 No. 2, 2018, pp. 25-30. doi: 10.5923/j.ajmms.20180802.02.
Article Outline
1. Introduction
- Acute kidney injury (AKI) is a clinical syndrome denoted by an abrupt decline in glomerular filtration rate (GFR) sufficient to decrease the elimination of nitrogenous waste products (urea and creatinine) and other uremic toxins. This has traditionally been referred to as acute renal failure (ARF), but in recent years an effort has been made to implement the term acute kidney injury instead, and to develop a standardized definition of AKI [1].Perrin et al., 2012 [2] explained that Contrast-induced nephropathy (CIN) is classically defined as a relative (≥25%) or absolute (≥0.5 mg/dl; 44 μmol/l) increase in serum creatinine from baseline value. CIN accounts for 10 to 15% of hospital-acquired acute renal failure and may rarely lead to irreversible renal function loss. Perrin et al., 2012 [2] explained that Contrast-induced nephropathy (CIN) is an acute renal injury due to the renal toxicity of iodinated contrast media. Functionally, CIN is considered an intrinsic acute kidney injury (AKI), usually with conserved diuresis, but in severe cases, acute tubular necrosis and even end-stage renal disease may develop [3]. Contrast Induced Nephropathy (CIN) is defined as an absolute (≥0.5mg/dl) or relative increase (≥25%) in serum creatinine at 48–72 hours after exposure to a contrast agent compared to baseline serum creatinine values, when alternative explanations for renal impairment have been excluded [4].James et al., 2013 [5] suggested that contrast induced acute kidney injury is associated with an increased risk of mortality, cardiovascular events, end stage renal disease, and prolonged hospitalization. However, the association between contrast induced acute kidney injury and mortality is strongly confounded by baseline clinical characteristics that simultaneously predispose to both kidney injury and mortality.Several risk factors for CIN have been identified; Chronic renal insufficiency, diabetes mellitus, congestive heart failure, intravascular volume depletion, the use of a large amount of contrast agent and type of contrast used either ionic or non ionic dye are considered important predisposing factors [6].
2. Aim of the Study
- Study the Incidence and the effect of modifiable and non-modifiable risk factors for occurrence and prognostic impact of Contrast Induced Nephropathy post coronary interventions in patients admitted at AL-Azhar University Hospital, New Damietta, Egypt.
3. Patients and Methods
3.1. Study Design
- This study was conducted on 120 patients attended at the emergency unit, cardiac outpatient clinic and Internal medicine department of Al-Azhar university hospital (New Damietta). They were presented with cardiac symptoms (chest pain, dyspnea, low cardiac output symptoms., acute coronary syndrome or chronic stable angina). They were subjected to coronary angiography and Percutaneous coronary Interventions after medical history taking, clinical examinations, and ECG findings suggestive of acute coronary syndrome. The coronary interventions were done at the cardiac catheter unit of Al-Azhar university hospital New Damietta in the period from December 2014 and August 2015. Serum creatinine levels were measured at baseline, every day for the following two days in the CCU and after one and two weeks of the time of admission to evaluate contrast Induced Nephropathy (CIN). All patients were assessed for risk factors either modifiable or non-modifiable, Non modifiable: major, pre-existing renal disease, diabetes mellitus, minor; age, sex, reduced ejection fraction, congestive heart failure, hypertension. Modifiable; major; ionic content of contrast medium, volume of contrast medium administrated, repeated exposure to contrast medium. Minor; low effective circulating volume (dehydration), myocardial infarction less than 24 hours before angiography, circulatory collapse and drug intake.
3.2. Ethical Aspects
- The informed consent was obtained from all participants. The research protocol did not interfere with any medical recommendations or prescriptions.
3.3. Inclusion Criteria
- Age: above 18 years, sex: both sexes, patients admitted to undergoing coronary angiography and percutaneous coronary interventions.
3.4. Exclusion Criteria
- Patients on chronic peritoneal or hemodialysis, patients presented within 18 hours after acute myocardial infarction to exclude cardiogenic shock as a pre renal cause of nephropathy, Patients with conditions that may predispose to acute renal injury as sepsis, gastroenteritis, nephrotoxic drugs.
3.5. Study Protocol
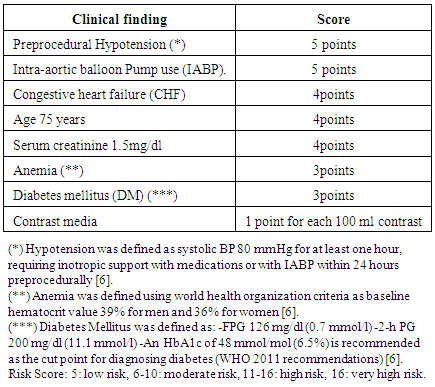
- A. Contrast Induced Nephropathy was diagnosed when rising of serum creatinine (≥0.5mg/dl) or increase (≥25%) in serum creatinine at 48–72 hours after exposure to a contrast agent compared to baseline serum creatinine values [4].B. All patients were subjected to Complete Medical History and full clinical examination with special emphasis on Risk factors for developing CIN; age, diabetes mellitus, symptoms of congestive heart failure and any degree of chronic kidney disease.C. Risk stratification for development of CIN was calculated (The Mehran risk score):
 D. Laboratory assessment: Basal serum creatinine before coronary angiography and percutaneous coronary Intervention follow up serum creatinine 48 hours later and two weeks later, serum Na (meq/dl), serum K (meq/dl), serum uric acid (mg/dl), urine analysis, serum cholesterol, serum triglycerides, CBC, liver enzymes, fasting and 2 hours post prandial blood glucose level, Hg A1 C.E. Cardiac assessment methods: In all cases, the cardiovascular disease (CVD) was assessed by: 1-ECG, finding of ischemia, including (ST-T wave changes) and arrhythmia 2-Echocardiography (ECHO) for the following parameters LV ejection fraction and regional wall motion abnormalities.
D. Laboratory assessment: Basal serum creatinine before coronary angiography and percutaneous coronary Intervention follow up serum creatinine 48 hours later and two weeks later, serum Na (meq/dl), serum K (meq/dl), serum uric acid (mg/dl), urine analysis, serum cholesterol, serum triglycerides, CBC, liver enzymes, fasting and 2 hours post prandial blood glucose level, Hg A1 C.E. Cardiac assessment methods: In all cases, the cardiovascular disease (CVD) was assessed by: 1-ECG, finding of ischemia, including (ST-T wave changes) and arrhythmia 2-Echocardiography (ECHO) for the following parameters LV ejection fraction and regional wall motion abnormalities.3.6. Statistical Methodology
- Data entry and analysis were done using SPSS version 17, Data were presented as mean, SD, NO, and percentage, Cochran Armitage Chi-square test was used to compare qualitative data between the two groups of patients, Independent samples T-test was used to compare means of both groups, Paired samples T-test was used to compare means before and after the procedure (CA or PCI) in the same group. P-value considered significant when it is < 0.05, Regression analysis was done and or was calculated for independent risk factors, all results were presented in the form of tables and figures.
4. Results
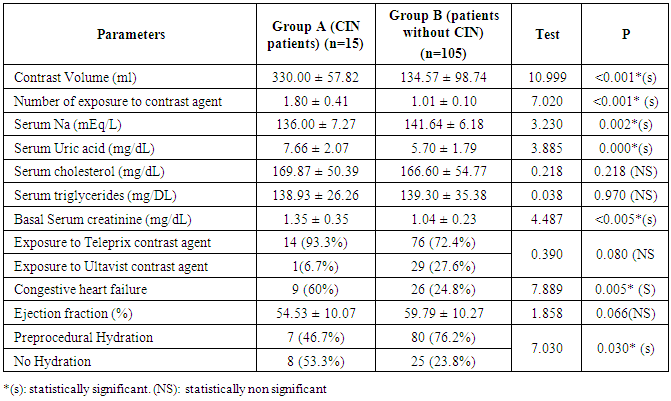
- 15 patients out of 120 patients developed contrast induced nephropathy (12.5%) 3 females and 12 males there mean age was 54.47 ± 4.47years, 6 (40%) of them underwent coronary angiography while the other 9 (60%) underwent percutaneous coronary intervention. 105 patients out of 120 patients didn’t develop contrast induced nephropathy (87.5%) 24 females and 81 males there mean age was 56.33 ± 6.63years, 54 (51.4%) of them underwent coronary angiography while other 51 (48.6%) underwent percutaneous coronary intervention. So studied 120 patients were divided into 2 groups: (group A) patients who developed contrast induced nephropathy (15 patients) and (group B) patients without contrast induced nephropathy (105) patients. There was statistical significant increase of serum creatinine, follow up 48h serum creatinine after coronary interventions and follow up 2 weeks serum creatinine in group A in comparison to group B. There was no statistical significance difference in both groups as regard to age and sex. There were statistically significant increase of D.M, HTN and congestive heart failure in group A in comparison to group B. The number of patients having diabetes mellitus was 49 patients, 10 patients (66.7%) in group A and 39 patients (37.1%) in Group B and the incidence of CIN in diabetic patients was 20.4%. The number of patients having hypertension was 43 patients, 12 patients (88%) in Group A and 31 patients (29.5%) in Group B. The incidence of CIN in hypertension patients was 27.9%. There was a statistically significant increase in volume and number of exposures to a contrast agent in group A in comparison to group B. There was no statistically significant difference in both groups as regard to type of contrast agent. There was a statistically significant increase of pre-procedural hydration percent in group B in comparison to group A. There was no statistically significant difference of Ejection fraction in both groups. There was statistically significant decrease of serum Na in group A in comparison to group B. There was a statistically significant increase of serum uric acid in group A in comparison to group B There was no statistically significant difference of serum cholesterol and Triglycerides in both groups. In this study, we found that 8 patients (53.3%) in group A and 16 patients (15.23%) in group B receive metformin, 3 patients (20%) in group A while 52 patients (49.5%) receive ACE inhibitor and 2 patients (13.3%) in group A and 27 patients (25.7%) receive beta blocker. In Group A the outcome of patients who underwent coronary angiography, there was 1 (16.67%) out of 6 patients have normal coronary angiography while others have disease one of the coronary arteries, and in Group B 5 (9.26%) out of 54 patients were normal coronary angiography angiography while others have disease one of the coronary arteries.
|
5. Discussion
- In the current study, there was no statistically significant difference in both groups (patients with CIN and patients without CIN) regarding sex, age, type of contrast agent, serum cholesterol and serum triglyceride. And there were statistically significant increase the volume of contrast agent, the number of exposures to dye, diabetes mellitus, hypertension, hydration, blood urea, low serum sodium and high serum uric acid in group A (patients with CIN) than in group B (patient without CIN).Diabetes mellitus has been established as an independent risk factor for CIN. Presence of DM is associated with a 1.5 ~ 3 fold higher risk of AKI after exposure to contrast media. Furthermore, DM amplifies the risk conferred by pre-existing renal insufficiency alone. The mechanisms include a predisposition of the host kidney to ischemic injury from vasculopathy, increased oxidative stress/free radical damage, and endothelial dysfunction. Fluid retention in DM patients also increases the use of diuretics, also a risk factor for CIN. Likewise, a pre-procedural glucose level higher than 200 mg/dL is also a risk factor for CIN [7]. In this study, the number of patients having diabetes mellitus was 49 patients, 10 patients (66.7%) in Group A (patients with CIN) and 39 patients (37.1%) in group B (patients without CIN). The incidence of CIN in diabetic patients was 20.4%. Finding was in agreement with Nikolsky et al 2004 [8]. Who found that the incidence of CIN in diabetic patients varies from 5.7 to 29.4%. On the other hand Kurnik et al 1998 [9] documented that in diabetic patients with preserved renal function and in the absence of other risk factors, the rates of CIN are usually comparable to those of a non-diabetic population, while clinically important CIN usually occurs in a subset of diabetics with underlying renal insufficiency.In this study, the number of patients with hypertension were 43 patients, 12 patients (88%) in Group A (patients with CIN) and 31 patients (29.5%) in Group B (patients without CIN). The incidence of CIN in hypertension patients was 27.9%. Findings were in agreement with Iakovou et al., 2003 [10]. Who suggested that hypertension is a risk factor for CIN.In this study, the number of patients presented by manifestations suggestive of heart failure were 35 patients, 9 patients (60%) in Group A (patients with CIN) and 26 patients (24.8%) in Group B (patients without CIN). The incidence of CIN in heart failure patients was 25.7%. This can be explained that heart failure may decrease renal blood flow. These findings were in agreement with Rihal et al., 2002 [6]. Who reported that advanced congestive heart failure (New York Heart Association class III or IV), or any history of congestive heart failure are independent risk factors for CN and contribute even greater risk in patients with diabetes or renal disease.Among the study population, the mean baseline serum creatinine level was 102.94± 26.69 µmol/L for Group A (patients with CIN) and 79.30± 17.54 µmol/L for Group B (patients without CIN). And was statistically significant increase in Group A (patients with CIN) in comparison to Group B (patients without CIN). These findings were in agreement with Hall et al 1992 [11] who stated that the higher the baseline creatinine value, the greater is the risk of CIN. They suggested that, if baseline plasma creatinine level is 1.2 mg/dl, the risk of CIN is only 2%. In patients with values of creatinine in the range of (1.4–1.9 mg/dl) the risk of CIN compared with that in the previous group increases fivefold (10.4%). As for patients with baseline creatinine level >2.0 mg/dl, more than half of them (62%) subsequently develop CIN. However, baseline creatinine is not reliable enough for identification of patients at risk for CIN. This is because the serum creatinine value varies with age, muscle mass, and gender. Since creatinine production decreases with age, a normal serum creatinine in an elderly patient generally correlates with at least moderate decrease in renal function. Also, Waybill et al., 2001 [12] reported that the incidence of CIN is variable and ranges from 5% to 50% in various series. The likelihood of developing CIN increases with worsening of the baseline renal function. Several studies provided evidence that older age is an independent predictor of CIN. The reasons for higher risk to develop CIN in the elderly were not studied specifically and probably are multi-factorial, including age-related changes in renal function (diminished glomerular filtration rate, tubular secretion, and concentrating ability). The presence of multi-vessel coronary artery disease, necessitating complex PCI, coupled with more difficult vascular access resulting from tortuosity and calcification of the vessels frequently requires a greater amount of CM, and therefore represents additional factors of increased CIN in elderly [6] In this study, the mean age of CIN patients was 54.47 ± 4.47 years while the mean age of without CIN patients 56.33 ± 6.63 years. And the difference was statistically non-significant between both may be explained by a small number of the study population. In this study, the volume of dye was a statistically significant increase in group A (330 ± 57.82 milliliters) than in group B (134.57 ± 98.74), in addition the patients underwent percutaneous coronary intervention in group A were 9 (60%) as there are larger volume of dye in these procedures than coronary angiography, this was in agreement with Marenzi et al., (2009) [13] who reported that the higher volume of contrast medium is deleterious in the presence of other risk factors. Even relatively low doses of contrast (less than 100ml) can induce permanent renal failure and increase the need for dialysis in patients with chronic kidney disease. As contrast volume increases, the risk of developing CIN sharply increases. As a general rule for patients with chronic kidney disease, a diagnostic catheterization should plan to use < 30 ml of contrast, and < 100 ml if percutaneous coronary intervention, this should be a reasonable goal.The structure of radio-contrast agents has been modified over the last several decades, yielding compounds with significantly less chemotoxicity [12] Contrast agents lead to increased osmolarity that may lead to medullary ischemia this ischemia will likely cause damage to the kidney, and that damage is mediated by oxygen-free radicals [14] The contrast agents may also have a direct toxic effect on the kidneys, which may be mediated through the production of oxygen-free radicals [15]. Aspelin et al., 2003 [16] reported that despite the still existing uncertainty regarding the degree of nephrotoxicity produced by various contrast agents, in practice iso-osmolar contrast media is a prefered agent in patients with renal impairment. On the other hand Rudnick et al., 1995 [17] reported that patients receiving HOCM (diatrizoate) were 3.3 times as likely to have nephropathy induced as those receiving LOCM (iohexol). In this study, Non-ionic dye was used in 1 patients (6.7%) in group A and in 29 patients (27.6%) in group B, while ionic dye was used in 14 patients (93.3%) in group A and in 76 patients (72.4%) in group B, and there was no statistically significant difference between both group regarding to the type of dye this may explained by a small number of study populations.In the present study there was statistically significant deference between both groups as regard to pre-procedural hydration percent as there were 8 patients (53.3%) in group A and 25 patients (23.8%) in group B don't receive hydration before the procedure while 7 patients (46.7%) in group A and 80 patients (76.2%) in group B received hydration this was in agreement with Gruberg et al., 2000 [18] who reported that the incidence of CIN was about 11% in patients who received hydration compared to the 22% to 37% in patients who did not receive hydration in a standardized fashion. However, our results were against Merten et al, 2004 [19] who showed that the patients with preexisting renal insufficiency undergoing diagnostic or interventional procedures requiring low-osmolar contrast media the CIN occurred in 1 of 60 patients (1.7%) receiving intravenous hydration with normal saline but in 8 of 59 patients (13.6%) who received placebo.In this study there was statistically highly significant decrease of serum sodium in group A (136.00 ± 7.27 mmol/L) than in group B (141.64 ± 6.18 mmol/L). And there was statistically highly significant increase of serum uric acid in group A (455.66 ± 123.13 µmol/L) than group B (339.06 ± 106.48 µmol/L) this was in agreement with Rich and Crecelius 1990 [20] who stated that low serum sodium and high serum uric acid levels were predictors of contrast nephropathy after coronary angiography.In this study it was found that contrast-induced nephropathy occurred in 15 cases (12.5%) among the study population, and of those only 2 patients required renal replacement therapy in the form of two sessions of hemodialysis and then there was a gradual improvement of renal function within 3 weeks. The other 13 patients were kept on conservative medical therapy 7 patients were improved within 2 weeks, however, another 6 patients had more prolonged and complicated clinical course than other patients and were followed up for another 3 weeks at the outpatient clinic and then discharged after normalization of renal function. It was noticed that 2 patients who required renal replacement therapy have a moderate risk according to Mehran risk score. Marenzi et al., 2004 [21] reported that dialysis as a result of CIN was required in 0.3% - 0.7 of patients on the other hand McCullough et al., 2003 [22] showed that the serum creatinine typically peaks 3–5 days after contrast administration and returns to baseline or near baseline within 1–3 weeks. In this study, Mehran risk score was calculated for the 15 patients who developed CIN and it was a moderate risk in 2 patients, which carried the highest pre-procedural predicted risk for CIN and it was low risk in 13 patients, this means that the Mehran risk score is very important for detection of prognosis of CIN and should be done for all patients undergoing coronary interventions. In this study the change in serum creatinine levels among the patients in whom CIN had occurred, the mean was 102.94± 26.69 µmol/L at baseline, it rose to reach 223.41± 52.61 µmol/L forty-eight hours after intervention, and then it declined to reach 160.89± 86.92 µmol/L two weeks after intervention. In our study in Group A the outcome of patients who underwent coronary angiography, were 1 (16.67%) out of 6 patients have normal coronary angiography while others have diseased one of the coronary arteries, and in Group B 5 (9.26%) out of 54 patients were normal coronary angiography while others have disease one of the coronary arteries this means that many patients not indicated for coronary angiography and underwent the hazards of dye exposure this is agree with Curhan et al., 2003 [23] who reported that management of contrast nephropathy is mainly by prevention; this can be achieved by assessment of the risk-benefit ratio prior to performing the procedure, as well as the patient's receiving adequate hydration and having normal electrolyte levels. Also use of the new low osmolar contrast agents should be undertaken in patients with higher serum creatinine levels. In this study, we found that 8 patients (53.3%) in group A and 16 patients (15.23%) in group B receive metformin, 3 patients (20%) in group A while 52 patients (49.5%) receive ACE inhibitor and 2 patients (13.3%) in group A and 27 patients (25.7%) receive beta blocker. This means that receiving medications such as metformin, ACE inhibitor, may considered as risk factor for CIN and should be stopped before the procedure as possible. Katzberg., 1997 [24] stated that the introduction of questionnaires to be included with outpatient appointment cards may have the additional benefit of highlighting other relevant information such as history of anaphylaxis to the dye or treatment with metformin that may accumulate if renal function is impaired and may predispose to CIN.
6. Conclusions
- Contrast nephropathy is a major cause of morbidity in patients undergoing coronary angiography or per cutaneous coronary interventions, risk factors for CIN such as diabetes mellitus, congestive heart failure, hypertension, and medications, high osmolality and high ionic content of contrast medium, large volume of contrast medium and recurrent contrast exposure all are included in increased incidence of occurrence of CIN and poor the prognosis. Proper selection of patients who undergo contrast imaging and pre-procedural preparations would be helpful to reduce the risk of CIN.
Abbreviations
- CIN
 Contrast induced nephropathyDM
Contrast induced nephropathyDM  Diabetes MellitusAKI
Diabetes MellitusAKI  Acute kidney injury
Acute kidney injury Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML