-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2018; 8(1): 1-6
doi:10.5923/j.ajmms.20180801.01

Outcomes of Azygoportal total Dissociation for Complicated Portal Hypertension: Comparison of Two Techniques
F. G. Nazirov , A. V. Devyatov , A. Kh. Babadjanov , U. R. Salimov , D. M. Khakimov
JSV «Republican Specialized Centre of Surgery named after acad.V.Vakhidov», 10, Kichik Xalqa str., Tashkent, Uzbekistan
Copyright © 2018 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

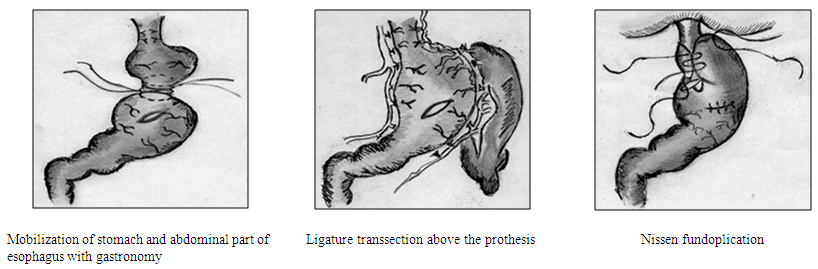
The aim of the research was to study the efficiency of different types of azygoportal collector total dissociation in patients with clinically significant portal hypertension. Material and methods: Depending on the procedure, the patients were divided into two groups. The first group consisted of 63 patients. Azygoportal dissociation was performed according to an original method. In the second group a modified version of azygoportal dissociation was performed. Patients were comparable in the main pathology and course of the disease. Results and discussion: Edematous ascitic syndrome; liver failure; insufficiency of gastro-gastral anastomosis and haemorrhagic syndrome were observed in 28.6%; 23.8%; 11.1%; and 14.3 against 16.5%; 7,7%; 0%; and 4.4% for patients of the I and II groups, respectively. Conclusion: proposed method of azygoportal collector dissociation on a prosthesis is a more effective method for hemorrhagic syndrome control and also allows to significantly reduce the incidence of severe complications in the nearest postoperative period.
Keywords: Liver cirrhosis, Portal hypertension, Dissociative surgeries, Ligature transection method, Bleeding from esophageal varices
Cite this paper: F. G. Nazirov , A. V. Devyatov , A. Kh. Babadjanov , U. R. Salimov , D. M. Khakimov , Outcomes of Azygoportal total Dissociation for Complicated Portal Hypertension: Comparison of Two Techniques, American Journal of Medicine and Medical Sciences, Vol. 8 No. 1, 2018, pp. 1-6. doi: 10.5923/j.ajmms.20180801.01.
1. Introduction
- Portal hypertension (PH) is one of the most frequent complications of liver cirrhosis. PH can lead to many complications such as development of esophageal varices (EV), hardly-controlled hemorrhagic syndrome, hepatic failure and edematous-ascitic syndrome [3, 5, 9, 12].Nowadays a lethality level at the peak of hemorrhage in the developing countries still remains high – up to 60%. At the same time, for the countries with highly developed hepatology service this index also remains high – up to 10- 20% [6, 18, 21, 7, 10]. The efforts of conducting a primary prevention with the help of endoscopic methods significantly reduce the risk of hemorrhagic syndrome development, but remain unsuccessful in 17-37% of patients [18]. Liver transplantation (LT), a surgical portosystemic shunting (PS), transjugular intrahepatic portosystemic shunting (TIPS) and dissociative interventions are used for the prevention and treatment of hemorrhage from EV. It is known, that LT is the only curative treatment method for the patients with hepatocirrhosis. At the same time the quantity of patients in the waitlists is significantly higher than the quantity of donor organs – it significantly decreases the correlated indices of survival rate for such type of patients [8].As it has been registered for the last decades, a surgical PS is not so popular as the TIPS. But the wide popularization of the TIPS, by the number of authors’ opinion, is not often reasonable due to some significant lacks of the method [6, 14]. At the same time, performing a surgical PS which is the most effective treatment and prevention method of hemorrhagic syndrome cannot be possible in all patients. A wide group of patients is out of the possibility for performing PS subject to the presence of an evident decompensation of hepatic function due to the hemorrhage or anatomic peculiarities of the portal system. Dissociating procedures still remain the only method of aid in patients with extrahepatic form of PH (also known as extrahepatic portal obstruction or EHPVO) against the background of development risk or at the peak of hemorrhage [16].
2. Material and Methods
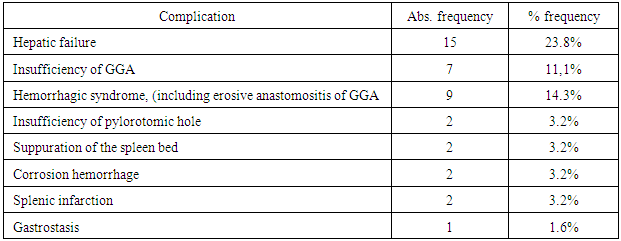
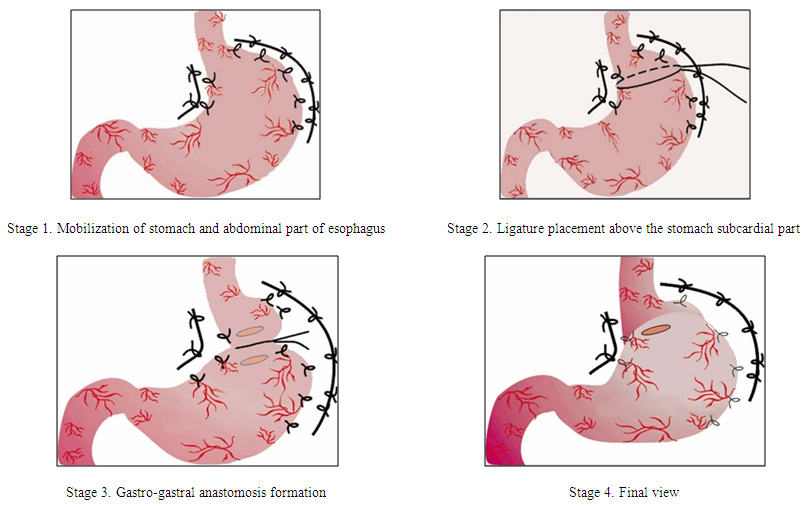
- A comparative investigation of two azygoportal collector dissociation methods in patients with PH syndrome has been carried out. Treatment results of 155 patients who were operated at the Republican Specialized Centre of Surgery (RSCS) named after academician V. Vakhidov from 1997 to 2017 were analyzed. With the accordance of the total dissociative method, patients were randomized to 2 groups. The original disconnection method of azygoportal collector was performed for the patients of the 1st group. Dissociation of the gastroesophageal collector in the modified version was performed in the patients of the 2nd group. There were 63 patients with PH syndrome in the 1st group: 40 (63.5%) of them had liver cirrhosis and 23 (36.5%) patients were suffered from extrahepatic form of PH. In 19 (30.2%) cases surgery was performed at the peak of the hemorrhage. Dissociation of the azygoportal collector in combination with splenectomy was carried out in 19 (11.9%) patients. There were 92 patients with PH in the 2nd group. 57 (62.6%) of them had liver cirrhosis, 33 (36.3%) - extra hepatic form of PH. One patient (1.1%) was admitted with Budd-Chiari syndrome. In 28 (30.7%) cases the surgery was performed at the peak of the hemorrhage. Dissociation of the azygoportal collector in combination with splenectomy was carried out in 12 (13.2%) cases. In other 7 (7.7%) patients the azygoportal disconnection was supplemented with the ligation of a splenic artery. F.G.Nazirov’s original method (the 1st group)Devascularization of the stomach is carried out after upper laparotomy up to the abdominal part of the esophagus along both parts of the stomach. The organ blood supply is kept due to right gastric and two gastroepiploic arteries. Left gastric artery is ligated and dissected out of the organ. Double circular suture is formed at the subcardial level and the ligature is tightened. The next stage is the formation of anterior gastro-gastral anastomosis between the upper and the lower parts of the stomach which were formed by the ligature transsection.The size of anastomosis camera is up to 3 cm. The important advantage of the surgery is in keeping the cardioezophageal connection and in the prevention of reflux esophagitis in the postoperative period (Fig.1).
 | Figure 1 |
|
 | Figure 2 |
3. Results
- From 63 patients of the 1st group and 91 patients of the 2nd we observed a complicated nearest postoperative period in 25 (39,7%) and 18 (19,8%) patients respectively. The structure of complications was as follows: edematous ascitic syndrome; hepatic failure; insufficiency of GGA and hemorrhagic syndrome the frequency of which made up 28.6%; 23.8%; 11.1%; and 14.3% versus 16.5%; 7,7%; 0%; and 4.4% for the 1st and the 2nd groups respectively. Liver cirrhosis vs extra hepatic portal hypertension (EHPVO)As it is known, any surgical intervention in patients with chronic diffuse diseases of liver is interfaced with the risks of hepatic decompensation. The frequency of this complication which was manifested by edematous ascitic syndrome and hepatic failure also predominated in the group of patients with liver cirrhosis (LC) in compare with the patients who suffered from extra hepatic portal hypertension (EPH). So, in patients group with LC the symptoms of the hepatic failure were registered in 15 (38.5%) and 7 (12.3%) patients of the 1st and the 2nd groups. There were no laboratory data indicating hepatic failure among the patients with EHPVO. At the same time in 4 (16.7%) and in 3 (9.1%) patients with EHPVO of the first and the second groups we registered the presence of the medium or evident edematous ascitic syndrome. In our opinion, this complication which was easily treated by therapeutic correction could not be regarded as a manifestation of the hepatic failure in patients with a safe function of hepatocytes, but it is an effect of cachexia of the native protein-synthetic compensatory reserves due to hemorrhagic syndrome or the operative intervention. Recurrent hemorrhagic syndrome due to the LC was also observed in 7 (17.9%) and 4 (7.0%) patients of the 1st and the 2nd groups, but this index in patients with EHPVO was 2 (8.3%) and 0%. Besides, a general frequency of complications in patients with LC predominated over the patients with extra hepatic block of portal blood flow and indicated the deep abnormalities of patients’ general homeostasis due to diffuse lesions of the liver. Liver cirrhosis In consideration of the severity of PH syndrome course in patients with LC we have analyzed the frequency of complications development in this group of patients who were performed the original and modified methods of the surgery. In the nearest postoperative period the frequency of the hepatic failure predominated in both groups and it complicated a restorative period course in 15 (38.5%) patients of the 1st group and in 7 (12.3%) patients of the 2nd group. The recurrence of hemorrhagic syndrome was in 7 (17.9%) patients (the 1st group) and in 4 (7.0%) patients of the 2nd group. The edematous-ascitic syndrome rarely occurred in the group of patients who were performed the original method of surgery – 35.9% vs 21.1%. The mentioned results are explained by the direct correlation of edematous-ascitic syndrome with the rate of hepatic dysfunction. In connection with the reduction of the liver protein-synthetic function, both volume and adiaphoria of ascitic syndrome are risen. The frequency and resistance of the edematous-ascitic syndrome is decreased due to significantly less traumatism of the original method of the surgery and the less rate of hepatocellular failure. We registered the development of dissociative zone’s failure in 2 (3.5%) cases of the 2nd group. In 1 case the mentioned complication was developed in the patient who was performed the surgery having an active hemorrhage and a severe form of diabetes mellitus. In the second case that complication was developed in the patient with a total thrombosis of the portal vein and massive collateral circulation of cardioesophageal transition and retroperitoneal space (that case required a total devascularization of the stomach). In both cases the complication was solved by conservative procedures. There were 18 (46.2%) patients with different complications (the 1st group) and 15 (26.3%) patients in the 2nd group. Extra hepatic form of portal hypertension (EHPVO)It is known that the prognosis of the disease in patients with EHPVO is more favorable then in patients with a compromised liver. But according to some literary data, only in 12% of patients recanalization of the portal vein is observed – in the rest of cases a clinically significant PH syndrome is formed and it is required a surgical correction. The operative treatment results of the patients with the safe liver function who were performed original and modified surgeries were studied. We did not observe the laboratory manifestations of hepatic failure in patients of both groups. But an occurrence of the edematous-ascitic syndrome was observed in 4 (16.7%) cases of the 1st and in 3 (9.1%) patients of the 2nd groups. The recurrence of hemorrhagic syndrome was registered in 2 (8.3%) patients of the 1st group. There was no hemorrhage recurrence in the 2nd group. The postoperative period was complicated in 7 (29,2%) and 3 (9.1%) patients with EHPVO. The lethality of patients who were undergone original and modified methods of the surgeryThe patients lethality also differed in both groups - it proves that a modified method of the surgery is more effective. The lethality of the 1st group (original method) made up 10 (15.9%) cases, in the 2nd group - 10 (11%) patients. At the same time, even a lethality rate reaching 15.9% significantly differs from the stated rate which is typical for many other methods used in the world today. For example, by different authors data, a hospital lethality of the nearest postoperative period is observed in (35-75%) cases after a surgery offered by I. Boerema and in 20-55% - after the Sugiura’s surgery [1, 2, 4, 14]. The hospital lethality after the M.D.Patsiora’s surgery does not exceed 15% vs 11% for the patients who were performed F.G.Nasirov’s modified surgery. According to a comparatively low postoperative lethality which is typical for M.D.Patsiora’s surgery the frequency of the hemorrhagic syndrome recurrence in the nearest postoperative period reaches 20% vs 4.4% of F.G.Nasirov’s modified surgery. In our investigation the causes of the hospital lethality in the 1st group were: the hemorrhagic syndrome; hepatic failure; insufficiency of pylorotomic hole, corrosion hemorrhage which made up 4 (6%), 4 (6%), 1 (2%) and 1 (2%). In the 2nd group the causes of the hospital lethality were the hemorrhagic syndrome; hepatic failure; insufficiency of pylorotomic hole; corrosion hemorrhage and intestinal perforation which were observed in 3 (3.3%); 3 (3.3%); 2 (2.2%); 1 (1.1%); and 1 (1.1%) patients.
4. Discussion
- An evident advantage of azygoportal dissociation methods in patients with PH due to liver cirrhosis is a less risk of hepatic failure and encephalopathy development in comparison with the other methods due to PH conservation in the sine curves of cirrhotic liver. Dissociative procedures applied at the peak of hemorrhage are comparatively easy to perform and they are widely available in the remote districts where the access to high tech shunting interventions is limited. But, in spite of a big quantity of such surgeries, almost all of them are followed by either early hemorrhage recurrence, or high operative trauma and low survival rates. So, the frequency of hemorrhage recurrence at the N. Tanner’s surgery is 35-45% [1, 17]. At the M.D.Patsiora’s surgery which is the most popular methods among CIS countries this index can make up to 20% and more. Besides, in 8-14% of cases it is impossible to achieve bleeding control during the surgery [1, 17].The M.A. Hassab’s surgery which is widely-spread among the Asian-Pacific countries allows to reliably control the hemorrhagic syndrome. At the same time, a negative peculiarity of this method is a conservation of plethoric intramural veins of esophagus and stomach which also stipulates a high frequency of the hemorrhage recurrence (up to 25-34%) up to 5 years of observation [1, 11, 16].One of the well-known and inconsistent methods of azygoportal total dissociation is the Sugiura’s and S. Futagava’s surgery. A.K.Eramishantsev comments a Japanese method: «….each disconnection surgery has defects, but, in our opinion, the Sugiura’s surgery has a huge of them…...» [2]. The method has been upgraded many times with the aim of saving hemorrhage control results, the reduce operative injury and high rates of postoperative lethality [1, 19]. Though more than 20 modifications of the surgery has been offered till nowadays which are mainly directed to the minimization of the operative injury – the postoperative lethality still remains high and can reach 50%. The development and adoption of TIPS seemed to be a perspective method [14, 20]. But the recent wide randomized control investigations showed that this method also had serious disadvantages. A number of the late researches give significant defects of TIPS vs porto-systemic shunting. Hosokawa I. (2017) states that a frequency of the hepatic encephalopathy was observed by them 1.5 times more frequent in patients performed TIPS vs traditional interventions (39% vs 26%) [13]. Shunt occlusion was developed in 26% of patients after TIPS and was not observed in patients after the surgical portosystemic shunting. But, as it is mentioned above, in spite of the advantages of surgical shunting interventions it is not always possible to perform them. Thereby, nowadays there is no operative technique in the world which can be called “a golden standard” in the treatment of bleedings from esophageal varices. In this connection we have developed an original type of the operative intervention in our Centre which combines pathophysiologically substantiated elements of several nonshunting surgical methods. The method provides a positive long-term prophylaxis of the hemorrhagic syndrome in patients with PH who cannot be performed the alternative operative interventions. Hereby, the results of our investigation allowe to regard the F.G.Nazirov’s surgery as a competitive prevention and treatment method for hemorrhagic syndrome in patients with the PH in the conditions of impossibility of performing surgical shunting and at the ineffective endoscopic hemostasis both during a planned surgery and at the peak of hemorrhage.
5. Conclusions
- The advantages of the modified method: giving-up of performing gastro-gastral anastomosis allows to save a physiology of gastrointestinal tract and to reduce a duration of the surgery; an extensive intramural area of gastric veins disconnection achieved by ligature transsection allows to reach a sclerosed zone preventing a venous neovazation. The frequency of hemorrhagic syndrome development is reduced due to the achieving of more effective dissociation according to the probability of the erosive anastomositis. In conclusion, it can be said that deep analysis of the early postoperative complication rates and lethality showed a significantly lower rates in the modified technique group than in any of known analogues. A modification of the original method of gastroesophageal collector dissociation allowed to reduce the frequency of such complications as edematous-ascitic syndrome; hepatic failure; insufficiency of GGA and hemorrhagic syndrome from 28.6%; 23.8%; 11.1%; and 14.3 typical for the original method up to 16.5%; 7,7%; 0%; and 4.4% for the modified method.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML