-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2017; 7(2): 385-392
doi:10.5923/j.ajmms.20170712.01

Barriers to Adenoid and Tonsil Surgeries in Ekiti, Nigeria
Adegbiji Waheed Atilade 1, Gabriel Toye Olajide 2, Shuaib Kayode Aremu 2, Sulyman Biodun Alabi 3
1ENT Department, Ekiti State University Teaching Hospital, Ado Ekiti, Nigeria
2ENT Department, Federal Teaching Hospital, Ido-Ekiti, Nigeria/ Lecturer, College of Medicine & Health Sciences, Afe-Babalola University, Ado-Ekiti, Nigeria
3ENT Departments, University of Ilorin Teaching Hospital, Ilorin, Nigeria / Lecturer University of Ilorin, Nigeria
Correspondence to: Gabriel Toye Olajide , ENT Department, Federal Teaching Hospital, Ido-Ekiti, Nigeria/ Lecturer, College of Medicine & Health Sciences, Afe-Babalola University, Ado-Ekiti, Nigeria.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

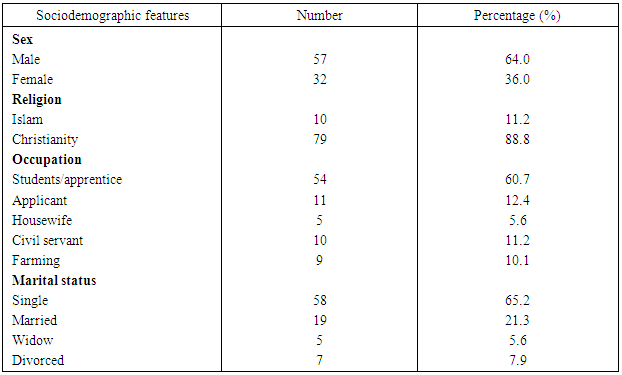
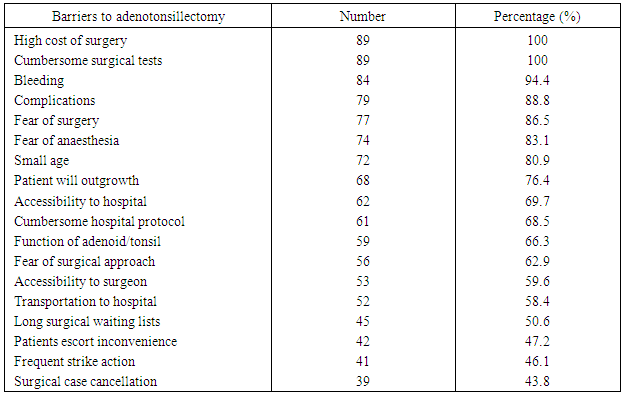
Aim and Background: Different form of barriers prevented or delayed patients from undergoing adenoid and tonsillar surgery in low-income countries. This study aimed at determining the prevalence of patients with barriers, types of barriers, identified affected individuals and possible way out to receive required adenotonsillar surgical care. Materials and Methods: This was a prospective hospital based study of patients scheduled for surgical procedures of adenoidectomy, tonsillectomy or both in the Ear, Nose and Throat department of Ekiti state university teaching hospital, Ado Ekiti, over a period of two years between July 2015 and June 2017. Results: A total of 172 patients were scheduled for adenotonsillectomy out of which 89 patients had surgery done over the study period. This represented 51.7% of patients that had surgery done. Majority (59.6%) with barriers were in the age group (1-10) years. There were 64.0% males and 36.0% females with a male: female ratio of 2:1. Majority (60.7%) of the study population were students/apprentice. Among the participants, 34.8% resided in Ado Ekiti, 55.1% live outside Ado Ekiti and within Ekiti state, while 10.1% were from outside Ekiti state. Major indications for the surgeries were obstructive adenotonsillar hypertrophy in 71.9% patients, recurrent tonsillitis in 19.5% while 4.5% were due to otitis media. About 43.8% patients accepted the surgical option. For one reason or the other 23.6% patients’ differed date for the adenotonsillectomy while 19.1% patients preferred to wait for patients to outgrowth the condition. 13.5% of the patients preferred alternative to surgery. In the findings 43.8% patients had both adenoidectomy and tonsillectomy (adenotonsillectomy) done, 24.7% patients had only adenoidectomy done while 31.5% patients had only tonsillectomy done. No barrier was experienced in 15.7% patients, 58.4% patient’s encountered hospital based barrier, 38.2% encountered patients based barrier, and 48.3% of the studied patients encountered barriers from the hospital staffs. High cost of surgical service and cumbersome preoperative surgical tests were barriers in all (100%) patients. Other major barriers to adenotonsillectomy were fear of bleeding in 94.4%, 88.8% are due to fear of complications and 86.5% were due to fear of surgery itself. Conclusions: Close to half of the patients with adenoid and tonsils disorder did not have the scheduled surgery. They were mainly due to patients based barriers, hospitals based barriers and hospital workers based barriers in these study patients.
Keywords: Adenotonsillectomy, Adenoid, Tonsils, Surgical barriers, Acceptability
Cite this paper: Adegbiji Waheed Atilade , Gabriel Toye Olajide , Shuaib Kayode Aremu , Sulyman Biodun Alabi , Barriers to Adenoid and Tonsil Surgeries in Ekiti, Nigeria, American Journal of Medicine and Medical Sciences, Vol. 7 No. 2, 2017, pp. 385-392. doi: 10.5923/j.ajmms.20170712.01.
1. Introduction
- Adenotonsillectomy is one of the commonest otorhinolaryngological surgical procedures performed worldwide and in the United States annually [1]. American Academy of Pediatrics (AAP) and the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) recommended this as first-line treatment for obstructive adenotonsillar hypertrophy with obstructive sleep apnoea syndrome in their guidelines [2, 3]. In a survey of practice patterns by otorhinolaryngologists in the United States there was non-mutually exclusive increase in indications for the surgery included obstructed breathing of any type in 59% of cases, recurrent infections in 42%, and OSA in 39% of children [4]. There were different obstacles to perform adenotonsillectomy.Global improvements in general health care services over the last few decades have resulted in increasing lifespan [5]. Otorhinolaryngological disorders including other surgical diseases constitute about 16% of the global disease burden [5]. Adenotonsillectomy with other surgery for upper airway obstruction has been associated with excellent relief of life threatening otorhinolaryngological disorders. In Nigeria, there are over 200 Otorhinolaryngologists spread across the country, although they are not evenly distributed; the mega cities and state capitals have greater proportion while they are few in the rural communities. In contrast, the rural communities have high prevalence of surgical conditions which are amenable to essential otolaryngological surgical care and they are not able to access required surgical care [6-8]. Despite all the safety measure taken in these procedures, all the assurance given and the magnitude of the disease condition different barriers to surgical uptake have been documented worldwide, especially in our environment. Adenotonsillectomy is not excluded in these barriers. In a surgical survey in Nepal, 31% of the studied population had one or more barrier to access to surgery [8]. Therefore, there is a need to investigate factors which tend to reduce access to affordable and accessible adenotonsillectomy in otorhinolaryngological practices in this part of the world. Community utilization of health care services is influenced by a range of psychological, cultural, socioeconomic and other factors [5, 9]. Otorhinolaryngological surgical care services are no exception. Barriers to any surgical and adenotonsillectomy uptake are multifactorial and are divided into 3 main groups [10-13].Firstly, Hospital-based barriers such as accessibility of hospital, long waiting hour to access surgeon, lack of modern equipment, high cost of services, lack of accommodation for accompanying person during surgery, cumbersome surgical tests, and cancellation of operations [13]. Secondly, Patient-based barriers includes: fear of surgery, fear of the outcome of surgery, socio-economic factor, dislike of hospital protocols and so on [13]. Finally, hospital-worker based barriers includes: lack of confidence in surgical team, bad attitude of hospital workers, and fear of health workers [5, 13].Countries with middle and high income account for 30.2% of the world population and had 73.6% of operations [14]. Low income countries including Nigeria accounted for 34.8% of the population but only 3.5% of all had required surgical procedures [14]. The objective of this study was to determine the prevalence of patients with barriers, types of barriers, identified affected individuals and possible way out to receive required adenotonsillar surgical care in Ekiti State University Teaching Hospital, Ado Ekiti. This is to strategies to improve the care of the patients scheduled for adenotonsillectomy in Nigeria.
2. Material and Methods
- This is a prospective hospital based study carried out among patients seen and worked up for surgical procedures of adenoidectomy, tonsillectomy or both in the department of ear, nose and throat of Ekiti state university teaching hospital, Ado Ekiti, Nigeria over a 2 years period (between July 2015 and June 2017). Data were collected from consecutive consented patients and confidentiality was assured using a pretested semi structured questionnaire. Information collected included their demographic characteristics, indications for adenoid and tonsillar surgery, acceptability, the category of surgery and barriers to the surgical procedure. All patients had detailed otorhinolaryngological, head and neck history including clinical examination.All consecutive patients scheduled for adenoidectomy, tonsillectomy or both were included in the study. Three study groups were defined among the individuals who were scheduled for adenotonsillectomy. This division was based on the patient’s barriers, hospital barriers and hospital worker barriers.Data obtained were analyzed using SPSS software Version 16.0 and presented in simple tables and charts.Ethical clearance for this study was sought for and obtained from the ethical committee of the institution before the data collection.
3. Results
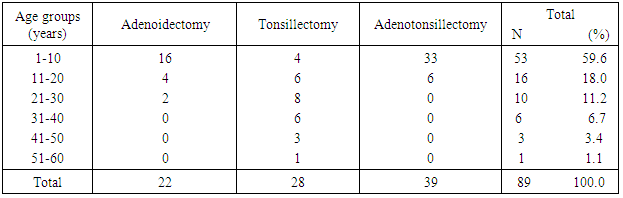
- A total of 172 patients were scheduled for adenoid and tonsillar surgeries during the study period. They consented and were enrolled into the study out of which 89 had their surgery done. This represented 51.7% of patients that had surgery done.Age group distributions of the respondents were shown in table 1. The patients in the age group (1-10) years constitute the majority 53 (59.6%) with barrier. The minority age groups were (51-60) years with only 1 (1.1%) patient had a barrier.
|
|
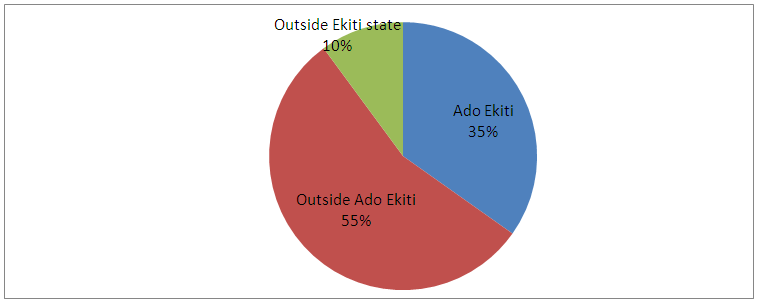 | Figure 1. Domicile of adenotonsillectomy patients |
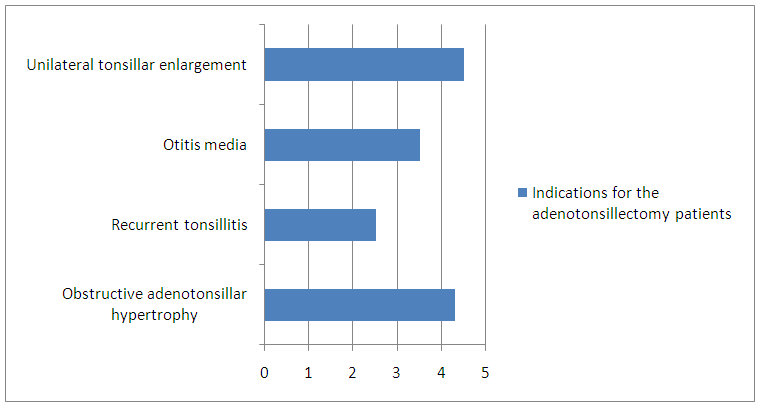 | Figure 2. Indications for the adenotonsillectomy patients |
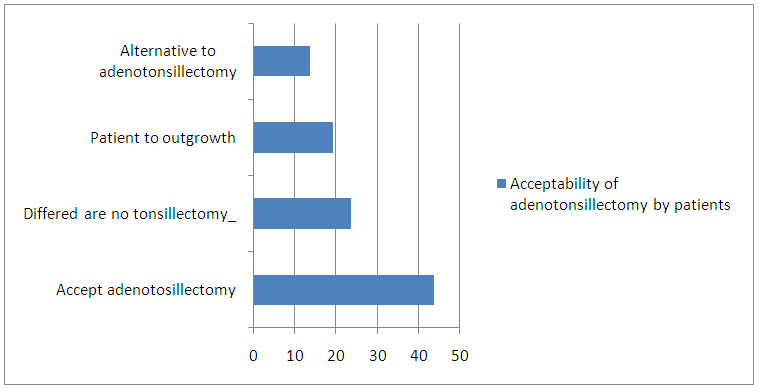 | Figure 3. Acceptability of adenotonsillectomy by patients |
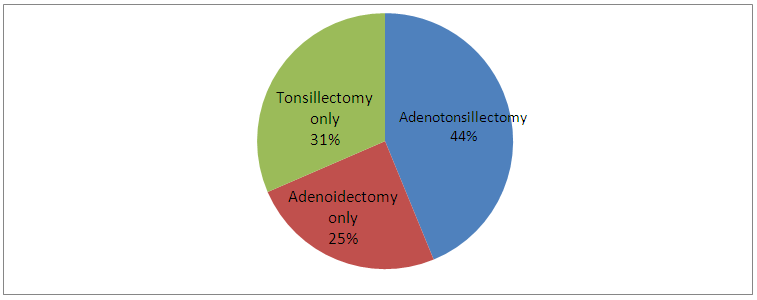 | Figure 4. Types of adenoid and tonsillar patients |
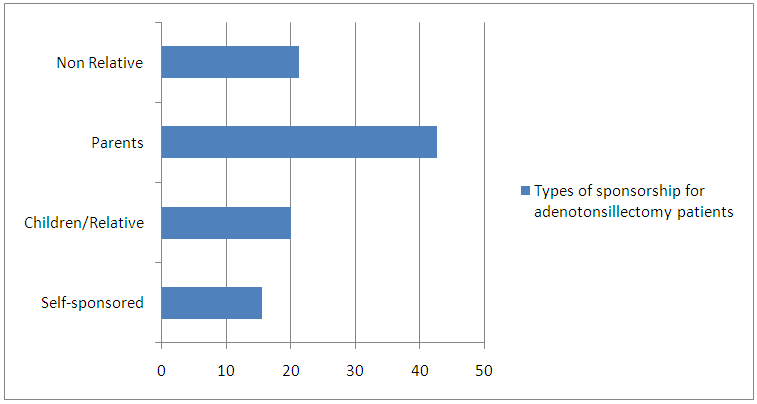 | Figure 5. Types of sponsorship for adenotonsillectomy patients |
|
4. Discussion
- The needs for adenotonsillectomy surgical care cover all the studied age group from neonate to geriatric as demonstrated in the findings of this study. Prevalence of adenoid and tonsillar disorder are high worldwide and the extent of use of surgical services is limited as demonstrated in other studies [15-18]. The surgical procedure of tonsillectomy tend to cut across all ages as shown in this study, but there need to note that adenoidectomy and adenotonsillectomy are common in children and young adult because adenoids tend to gradually atrophies as from age fifth to eighth years.Findings in this study revealed that only about half of the population scheduled for surgery had adenotonsillectomy done. This is due to various forms of surgical barriers encountered by the patients or their relations. This finding is similar to other study on barrier to surgery where financial barriers and barriers related to accessibility are even much lower [19]. In addition to surgical care like other health service utilization had been known to be greatly influenced by patients perception also their positive perceptions tend to increase utilization of the services and vice versa [19, 20]. This study revealed male were affected commoner than female counterpart. This proportional difference between the genders within the respondents further highlights the importance of systematic identification of barrier to surgical management of adenotonsillar diseases. This also address barriers to adenotonsillectomy at the study center to improve the uptake of this essential surgical care [21, 22]. Adenotonsillectomy and other surgical care in low-income countries such as Nigeria are limited by several factors. This varies greatly compared to high-income countries like USA. There are several barriers in this study that limit access to adenoid and tonsillar surgery in this low- income country. They are further classified into most importantly the financial barriers (affordability), cultural barriers (acceptability) and structural or geographical barriers (accessibility) in this study [13]. Financial barriers are the pivot to the entire barrier to adenoid and tonsillar surgeries. Differences between individuals who undergo or who do not undergo adenoid and tonsillar surgery in this study are partly due to inequalities in income among the participants [23]. Several financial-related characteristics were more prevalent in this studied group as many patients did not undergo surgery due to affordability, such as lack of money to access secondary health care facility for the treatment of their various illnesses [24]. Further documented financial barriers include costs for transport, surgical fee, preoperative investigation fee, feeding money, money for medication and so on [24]. In this study majority of the patients were dependents age categories such as paediatrics age groups, students/apprentices and applicants. Few patients were self sponsors while majority were sponsored by children, parents and non-relation. Majority of the participants resides both outside Ado Ekiti and from neighbouring state. In some cases individuals with lower financial means may have more problems in receiving surgical care than other individuals. The expenses also include cost on preoperative investigation, surgical fee, patient’s escorts and other welfare expenses. Some of the possible way out of these barriers is to provide free or subsidized surgical, feeding and transport for patients who need adenoid and tonsils surgical care for those that cannot afford these costs. This has also been suggested in another research study [25]. In addition to that, cultural barriers in low-income countries includes fear of receiving orthodox treatment or undergoing surgery in a health facility this is due to belief in spiritual causes of their illnesses as was in other studies [26, 27]. It is also important to note that inadequate access to surgical services has resulted in increased morbidity and mortality from complicated adenotonsillar disorder. Some participant’s alternatives to otorhinolaryngological surgical care were patent medicine shops, pharmacy, spiritual churches, muslim’s clergy and indigenous herbal medicine [28]. Their availability is high because of high patients patronage via unrestricted media advert are also other negative barriers against uptake of surgical services. Patients usually spent their money at the primary alternative center and presented in hospital with complicated case, end stage, terminally ill with empty handed when the alternative care failed. Further reasons for the ear, nose and throat surgical care inaccessibility include their poor perception of the hospital protocol and the hospital staff. Low proportion of the respondents accepted adenotonsillectomy as the option to treatment. Significant percentage of the studied population preferred alternative to surgery because of wrong information about surgical care from fellow patient, neighbor, or family member. This information varied with few patients perceiving ear, nose and throat surgery as a cause of mortality and disability after surgery [29]. The fear of mortality, disability after surgery, fear of bleeding, blood transfusion, pain, surgical and anaesthetic complications during or after surgery and death are major factors why most participants prefer alternative to adenotonsillectomy even if it is free surgical care [30].In this study many participants travelled long distance to reach surgical services which constitutes structural, accessibility or geographical location barriers. One of the major challenges facing health care providers in otorhinolaryngological, head and neck surgical care is the inequity in the provision and utilization of the surgical care. This is because of mal-distribution of the infrastructure necessary for the provision of surgical care between the rural and urban community. Most of the tertiary health institutions like this study center are located in state capital or city. This was also considered a major barrier from other study [23, 31, 32]. There is need for more regional facilities to deliver adenoid and tonsillar including other surgical care. There is need for more surgical centers in rural areas and posting of trained community healthcare workers to perform adenotonsillectomy and other common simple otorhinolaryngological surgeries. This will significantly reduce the burden of adenotonsillar surgical conditions in an economically low income community. Mobile clinics have been effective in performing some surgery in some study similar approach could be used for adenoid and tonsillar surgical procedures to improve accessibility [33].
5. Conclusions
- Findings from this study revealed close to half of the studied patients do not have scheduled adenotonsillectomy done as planned. The barriers for the adenoid and tonsillar surgery were further analyzed and were classified into financial barriers (affordability), cultural barriers (acceptability) and structural or geographical barriers (accessibility) in this study. Possible way out were health education with increase awareness raising campaigns for the patients, subsidizing cost of all aspects of surgical fees, training and distribution of surgical personnel to rural community and introduction of surgical outreach or mobile surgical clinics are advised.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML