-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2017; 7(1): 369-377
doi:10.5923/j.ajmms.20170711.02

The Hidden Truth behind Osteoporosis and Vitamin D Deficiency
Abdullah M. Nasrat1, Rand M. Nasrat2, Mohammad M. Nasrat2
1Department of Surgery, Zytona Therapeutic Center, Medina, KSA
2Department of Internal Medicine, Helwan General Hospital, Helwan, Egypt
Correspondence to: Abdullah M. Nasrat, Department of Surgery, Zytona Therapeutic Center, Medina, KSA.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The study aimed to demonstrate the possibility of an existing hidden underlying reason behind the increased frequency of osteopenia/osteoporosis and vitamin D deficiency during latest decades. Prevalence of osteopenia/osteoporosis and vitamin D deficiency constitutes a world health challenge. The latest decades demonstrated flare up of abnormal-existence/behavior colonic Helicobacter pylori strains and rising figures of disease spread related to these strains. The association of vitamin D deficiency with H. pylori is controversial in literature whereas it has been confirmed that colonic H. pylori strains could lead to abnormal lipid metabolism interfering with absorption of the fat-soluble vitamin D. H. pylori was found significantly associated with osteoporosis; H. pylori can influence osteoporosis directly by increasing the release of toxic inflammatory mediators and through the developed H. pylori related-vitamin D deficiency. Existence of colonic H. pylori strains was investigated among 100 males and females known with osteopenia/osteoporosis due to vitamin D deficiency employing a specific test. Natural measures for eradication of H. pylori with or without vitamin D supplement were employed for 3 groups of patients with osteoporosis/vitamin D deficiency and positive for colonic H. pylori strains in order to assess and compare effect of H. pylori eradication on recovery of vitamin D serum level. Significant recovery of vitamin D serum level was achieved within rather short duration of eradication of the colonic H. pylori strains employing natural measures even without further vitamin D supplement therapy. The striking association of colonic H. pylori strains with osteoporosis/vitamin D deficiency indicates that these strains could have a significant influence on the challenge of osteoporosis and vitamin D deficiency during latest decades. Eradication of colonic H. pylori strains from the colon employing natural measures could be therefore an effective measure to control the challenge of osteoporosis/vitamin D deficiency worldwide.
Keywords: Helicobacter pylori, Osteoporosis, Senna, Vinegar, Vitamin D deficiency
Cite this paper: Abdullah M. Nasrat, Rand M. Nasrat, Mohammad M. Nasrat, The Hidden Truth behind Osteoporosis and Vitamin D Deficiency, American Journal of Medicine and Medical Sciences, Vol. 7 No. 1, 2017, pp. 369-377. doi: 10.5923/j.ajmms.20170711.02.
Article Outline
1. Introduction
- Osteoporosis is an almost increasing public health problem worldwide. Osteoporosis is one of the most prevalent forms of age-related bone diseases, increased bone loss with advancing age has become a grave public health concern. Osteoporosis results from imbalance between bone resorption and bone formation; reduction in the quantity of bone tissue with deterioration of the bone micro-structure leads to general loss in bone strength and greater fracture risk. While it is part of the natural aging process, osteoporosis does not affect everyone to the same degree. [1-3] Genetic factors are considered major contributors to the pathogenesis of osteoporosis while menopause constitutes a major health risk as concerns osteoporosis because it is characterized by decreased bone density and increased fracture risk due to over-activation of osteoclastogenesis. Patients with organ transplantation are at further orthopedic risk as they require life-long immune-suppressive therapy to minimize the risk of immune-mediated graft rejection; complications of the immune-suppressive therapy such as impaired bone strength and increased fracture risk are common among those patients leading to increased morbidity and mortality rates. [1, 4, 5] Osteoporosis is diagnosed primarily by measurement of bone mineral density and several advanced techniques are available while treatment relies upon encouraging osteogenesis or inhibition of osteoclastogenesis. [4, 6, 7] Vitamin D has been appreciated for its role in bone health since its identification in 1921, it is important for non-skeletal health as much as for skeletal health. Vitamin D deficiency is a major association with the phenomena of osteoporosis due to lack of proper function of vitamin D in both calcium and phosphorus homeostasis in the bones. Vitamin D deficiency is recently a common health problem worldwide, it is more common than previously thought; more people have been found severely deficient in vitamin D. Sun exposure is considered the single most important source of vitamin D which is obtained primarily from skin exposure to ultraviolet radiation in sunlight. Hypovitaminosis D resulting from lack of ultraviolet rays exposure is not easily corrected by dietary intake alone in the absence of supplements. [8-12] The association between Helicobacter pylori and serum vitamin D level was found controversial by some investigators. [13] Previous studies have also reported conflicting results on the association between H. pylori and osteoporosis as the development of osteoporosis is complex and multi-factorial but recent reports have emphasized that early eradication could reduce the influence of H. pylori on osteoporosis. [14-16] It was collectively reported that advanced age, low body mass index and H. pylori positivity were the main risk factors for osteoporosis; however, the success of antibiotic H. pylori eradication was not shown to decrease the risk for osteoporosis. [17]
2. Motive of Study
- The marked prevalence of vitamin D deficiency during latest decades as if every living individual should have a degree of vitamin D deficiency and the common medical attitude that lack of sun exposure is the main reason behind this spreading and challenging frequency of vitamin D deficiency to the extent that a national survey in a sunny country like Saudi Arabia including 5000 individuals of all age groups of school students, boys and girls, and their male and female teachers has revealed prevalence of some degree of vitamin D deficiency among most of them which was attributed mainly to lack of sun exposure and next to bad nutritional habits. [18, 19] Exposure to the sun and lack of exposure to the sun should not vary very much during these latest decades from the decades before them and in spite of the fact that lack of sun exposure is the common traditional factor for vitamin D deficiency, it is still insufficient alone to explain the dramatic frequency of vitamin D deficiency during latest decades like a worldwide spreading influenza. These conflicting conceptions have attracted the attention of the research team and constituted part of the motive for this study. Revision of the clinical records of the research team of this study revealed the findings of 5 groups of patients with vitamin D deficiency as 10 patients per each group. These groups resembled civil service workers, traffic police officers, real estate professionals, golf players and owners of private boats for fishing and sailing. All these subjects showed moderate to severe vitamin D deficiency although they are candidates of sufficient sun exposure and the last three groups are supposed to be well to do having good nutrition advantages. In addition, frank colonic upsets were common features in all of them; that was exactly the main and real motive of this study. A general impression has developed that an environmental error could be there most probably in the colon as most population stepping on the earth are suffering colonic troubles. Lack of proper sun exposure is an integral reason for vitamin D deficiency but it seems that it is not the only or at least it is not the main factor responsible for the dramatic challenge of osteopenia/osteoporosis and vitamin D deficiency during latest decades as traditional risk rules such as age and gender are still insufficient alone to explain the flare up of osteoporosis/vitamin D deficiency during these decades. Therefore; efforts had been raised to search for a hidden reason apart of lack of exposure to the sun together with investigation of a colonic pathology that could have an influence on vitamin D uptake by the body, the blame was almost pointing towards existence of colonic H. pylori strains.
3. Aim
- Demonstration of the possibility of an existing hidden underlying environmental error behind the spreading challenge of the increased frequency of osteopenia/osteoporosis and vitamin D deficiency during latest decades.
4. Design & Settings
- A prospective clinical study done in Jeddah/Saudi Arabia between October 2015 and May 2017.
5. Patients & Methods
- The study included four groups of patients with different grades of moderate low bone density (LBD) due to vitamin D deficiency. The first group included 100 patients equally distributed between males and females known with different grades of LBD/vitamin D deficiency and colonic upsets having an age range of 45-59 years, they were randomly included in the study without any selection. The purpose of this group was to investigate the association of LBD/vitamin D deficiency with existence of the colonic Helicobacter pylori strains using a specific test (H. pylori fecal antigen test). [20] The second group consisted of 19 patients (8 males and 11 females) with Osteopenia/osteoporosis due to moderate to severe grades of vitamin D deficiency, their age ranged between 47-56 years. They were referred from a nutritional center for an alternative therapy for their resistant colonic upsets in spite of adequate medications, their response to vitamin D replacement therapy was also not satisfactory but they were not referred for this purpose. H. pylori fecal antigen test was employed for them and the patients who proved to be positive for colonic H. pylori strains followed natural measures for H. pylori eradication from the colon that was consisting of the senna leaves extract purge and vinegar therapy. The senna purge was used for eradication of H. pylori from the colon done once monthly for consequent three months to ensure eradication of the bacterium whereas vinegar therapy consisted of a vinegar-mixed salad with principal meals, once or twice daily/3-5days a week, in order to protect from the recurrence of any abnormal behavior H. pylori strains via food intake. [21] This group has been employed to demonstrate the effect of eradication of H. pylori from the colon via natural measures on the recovery of vitamin D serum level without further vitamin D supplements. As regards the third group, patients were selected from the first group including 20 patients equally distributed between males and females with an age range of 48-57 years, positive for colonic H. pylori strains and having minor or tolerable colonic troubles that were not in need of symptomatic or therapeutic medications, they were having rather a similar grade of vitamin D deficiency as that of the second group and they were receiving standard vitamin D supplement therapy. The purpose of the third group was comparative with patients of the second group as concerns the effect of H. pylori eradication on improvement of vitamin D serum level. A fourth group of patients who were selected also from the first group including 20 patients equally distributed between males and females with an age range of 46-56 years, positive for colonic H. pylori strains and having colonic troubles that were in need of natural therapy (senna leaves purge colon clear and vinegar therapy), patients of this group received standard vitamin D supplements for comparative reasons. All patients were of average body built or well-built. An additional fifth group to illustrate the effect of anti-H. pylori antibiotic therapy on the response of the body to vitamin D supplement therapy was not included for ethical reasons as H. pylori antibiotic eradication therapies demonstrate a lot of controversy. [20] Patients were followed up for 16-18 months.
6. Results
- The vast majority, 96 patients, of the first group (96%) were found positive for colonic H. pylori strains while all patients of the second group were positive for these colonic strains. Serum vitamin D level of the second group patients was ranging between 27-33 nmol/L and the range in the third group was 26-31 nmol/L while in the fourth group it was 29-37 nmol/L. Serum calcium and phosphorus were also compromised in all patients, that was at the lowest range of the normal average (Serum calcium 9.4-9.7 mg/dL and phosphorus 2.7-3.1 mg/dL). Serum vitamin D level of the second group (the group of colon clear/no vitamin D supplement) improved to 78-91 nmol/L after 12-14 weeks of colon clear and eradication of colonic H. pylori strains without any further vitamin D supplement therapy whereas it did not improve among the third group patients (vitamin D supplement/no colon clear) except to a range of 67-72 nmol/L after 16-20 weeks in spite of an adequate vitamin D supplement therapy. Serum vitamin D level of the fourth group (the colon clear/vitamin D supplement group) improved to 89-99 nmol/L after 8-9 weeks of colon clear and supplement therapy. The nutritional center has given a feedback comment that their referred patients (the second group) who followed the colon clear measures without vitamin D supplement therapy have shown relief of their colonic troubles and demonstrated stop in the progress of osteoporosis for 12 months follow up. Recurrence of vitamin D deficiency did not occur in the second group (colon clear/no vitamin D supplement) except in 4 patients due to recurrence of colonic H. pylori strains via query meals which has been corrected in few months after revision of colon clear. Recurrence of vitamin D deficiency occurred in most patients of the third group (vitamin D supplement/ no colon clear), 17 patients (85%), within few months (3-5 months) after discontinuation of the supplement therapy. The fourth group of patients demonstrated good recovery of vitamin D serum level in shorter duration while showing no recurrence of vitamin D deficiency until 12 months follow up.* The table demonstrates the serum vitamin D of the second, third and fourth groups before and after therapy together with calcium and phosphorus levels upon start of the study.
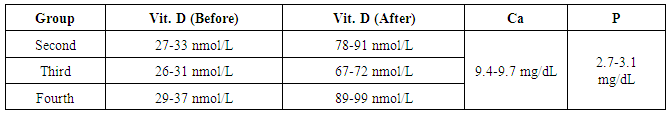 * The table illustrates comparative aspects of the second, third and fourth groups as regards employment of colon clear, intake of vitamin D supplements, rate of recovery of vitamin D serum level and incidence of vitamin D deficiency recurrence.
* The table illustrates comparative aspects of the second, third and fourth groups as regards employment of colon clear, intake of vitamin D supplements, rate of recovery of vitamin D serum level and incidence of vitamin D deficiency recurrence. 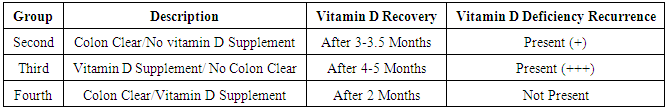
7. Ethical Considerations
- An informed signed consent was taken from all patients, they were made aware about safety of the natural vinegar therapy and senna extract purge, they were free to quit the study whenever they like. The research proposal was approved and the study followed the rules of the Research Ethics Committee.
8. Discussion
- The most important risk factors for developing osteoporosis are advanced age in both men and women, female sex and estrogen deficiency. Osteoporosis can be present without any symptoms for decades because osteoporosis does not cause symptoms until bone breaks. Therefore; patients may not be aware of their osteoporosis until they suffer a painful fracture. [1, 7, 8] The association between H. pylori existence and serum vitamin D deficiency was found controversial in the literature whereas conflicting results were reported on the association between H. pylori and osteoporosis. [13, 14] H. pylori may cause systemic inflammation and increase the production of tumor necrosis factors and interleukins; bone mineral density could be accordingly affected by these cytokines. [15, 16] Further studies investigating the risk factors for osteoporosis and whether the existence or eradication of H. pylori is associated with osteoporosis have reached a conclusion that H. pylori positivity is considered a risk factor for osteoporosis whereas the success of H. pylori eradication was not demonstrated to improve osteoporosis risk. [17]H. pylori existence as determined by serum antibodies and atrophic gastritis diagnosed on the basis of serum pepsinogen was found to significantly increase the risk of low trabecular bone density; accordingly it was emphasized that serological diagnosis of H. pylori existence and atrophic gastritis, which is usually utilized for risk assessment of gastric cancer, could be suggested as useful risk assessment for osteoporosis. [22-24] This matter has been attributed to the fact that H. pylori was linked to extra-digestive conditions and lifestyle-related diseases like osteoporosis as it could elicit a chronic cellular inflammatory response not only in the gastric mucosa but also in the extra-digestive organs particularly when cytotoxin-associated gene A (cagA) positive cytotoxic H. pylori strains are present. [25]The latest reports in the literature demonstrated a definite flare up of many medical challenges in a dramatic way through different reasons. [20] Traditional risk rules do not appear fully sufficient to explain the rising figures of the world’s spread of chronic illness. The latest three decades confirm the prevalence of abnormal-existence/behavior colonic H. pylori strains with flare up of a lot of medical challenges related to these abnormal strains through immune, inflammatory, toxic or different unknown reasons. [20, 21] H. pylori colonized the stomach since an immemorial time as if both the stomach wall and the bacterium used to live together in peace harmless to each other. H. pylori could migrate or get forced to migrate to the colon under the influence of antibiotic violence to become foreign structure to the tissues beyond the stomach as the bacterium is recognized only to the gastric wall tissues. H. pylori outside the stomach is therefore rendered a poison itself by inducing auto-immunity and a source of poison by leading to inflammatory reactions and local tissue pathology. Colonic H. pylori strains will continue producing ammonia for a reason or no reason, un-opposed or buffered by any acidity, leading to accumulation of profuse toxic amounts of ammonia that might cause different adverse toxic sequels inside the body. [20, 21] Different reports in literature have confirmed the association of cagA with colonic H. pylori strains and emphasized that cagA of H. pylori encodes a highly immunogenic and virulence-associated protein; the presence of this virulent gene in the body could affect the clinical outcome in many patients. [26, 27] Although vitamin D deficiency is common and prevalent, measurement of serum vitamin D level is expensive and universal screening is not supported. [8, 10] The association of overweight/obesity and dyslipidemia with existence of the colonic H. pylori strains has been emphasized and confirmed in literature. Obesity is found to be associated with abnormal lipid metabolism and as vitamin D is a fat soluble vitamin, hence obesity could be a risk factor for vitamin D deficiency. [12, 28-33] As long it was emphasized that the risk of developing osteoporosis is increased with the association of extra-gastric cagA positive H. pylori strains; early eradication of H. pylori was suggested in order to reduce the influence of H. pylori on osteoporosis via reducing the incidence of systemic inflammation and lowering cytokines production. [14-16, 22, 23] Accordingly; existence of the colonic H. pylori strains could have double influence in predisposing to osteoporosis; a direct influence through the release of pro-inflammatory mediators and indirect influence via predisposing to vitamin D deficiency due to impairment of lipid metabolism. [12, 28] The principle of employing the senna extract purge in the current study is eradication of the colonic H. pylori strains which are the suggested main pathogenesis leading to osteoporosis and vitamin D deficiency among the patients of this study. The senna leaves extract purge was demonstrated as the typical natural measure for definitive eradication of H. pylori from the colon. Three-times dilution of the standard senna leaves extract was found directly lethal to H. pylori strains on culture media. [33-35] Whereas employment of the vinegar therapy was meant to protect from recurrence of any abnormal-behavior H. pylori strains via buffering any query food intake. The complex nutritional requirements of H. pylori are achieved via its unique energy metabolism as the major routes of generation of energy for H. pylori are via pyruvate while the activity of the pyruvate dehydrogenase complex is controlled by the rules of product inhibition and feedback regulation. [36, 37] As acetate is demonstrated as an end product among the metabolic pathway of H. pylori; [38, 39] therefore, addition of acetic acid to the atmosphere around H. pylori could compromise the energy metabolism of H. pylori or interfere with the organism’s respiratory chain metabolism. So long the matter includes interference with the energy metabolism and respiratory chain metabolism of H. pylori, an immediate dramatic lethal effect on the bacterium could be considered. Twenty times-dilution of dietary white vinegar 6% was found instantly lethal to H. pylori strains on culture media. [34] Most of the miscorrelation as concerns the reported association between H. pylori and osteoporosis/vitamin D deficiency in literature is the result of missing the fact that colonic H. pylori strains could lead to pathologic sequels because of its abnormal existence while gastric H. pylori strains even with abnormal behavior do not induce inflammatory or toxic sequels beyond the stomach, most of the workers were searching only for the gastric but not for the colonic strains. The association of cagA with colonic H. pylori strains is confirmed in literature and it is emphasized that cagA of H. pylori encodes a highly immunogenic and virulence-associated protein. [40, 41] This matter is peculiar to extra-gastric H. pylori strains in general or most commonly to colonic H. pylori strains in particular while gastric H. pylori strains so long confined within the stomach seem to be innocent as concerns inducing immunogenicity as the bacterium is being recognized to the stomach wall tissues. More-over, these gastric strains even including abnormal behavior within the stomach do not lead to accumulation of toxic amounts of ammonia because of the buffering effect of gastric acid and therefore are not supposed to cause systemic inflammatory or toxic sequels beyond the stomach. [20, 21, 42] Most researches working on osteoporosis were looking for H. pylori in the stomach employing serological and urea breath tests or upper endoscopy, [16, 17] while H. pylori serum anti-body test is extremely non-specific, [20, 21] this could be most probably the reason for the resulting miscorrelation as colonic H. pylori strains could be co-existing and could be the reason behind the recorded bad sequels not the gastric strains. The association of H. pylori with osteoporosis is controversial in literature; different reports in literature have given conflicting results about the association between H. pylori and osteoporosis. Few studies have discussed the influence of H. pylori eradication therapy on bone mineral density. Some investigators reported that existence of H. pylori might be associated with an increased risk of developing osteoporosis but they did not demonstrate value of H. pylori eradication on osteoporosis risk. They emphasized that early eradication could reduce the influence of H. pylori on osteoporosis when the follow-up is greater than 5 years; [14] which is rather a long period to confirm exclusion of other related factors or ruling out other variables. The reason for this controversy is most probably because investigators were employing antibiotics for H. pylori eradication forcing more H. pylori strains to migrate to the colon, [20, 21, 34] which is unfortunate for the progress of osteoporosis. Antibiotic eradication therapies seem to have no effect on gastric H. pylori strains except forcing them to migrate from the stomach as evidenced by the observational finding of development of new symptoms and new sequels. [20, 34] This suggestion is supported by the findings that pseudo-membranous toxic colitis and toxic megacolon have developed after eradication of H. pylori by antibiotic therapy, [43, 44] whereas antibiotics are seldom effective against extra-gastric H. pylori strains. [45]Although osteoporosis is expected after the age of 50 years, physicians usually look for it at older age. The prominent observation in the current study is presentation of osteoporosis in rather lower age range without association of frank risk factors for developing osteoporosis in addition of finding osteoporosis among men rather similar as in females, therefore; this study might gain value from paying the attention towards the possibility to find osteoporosis at further lower age groups particularly when it is considered that diagnosis of osteoporosis is seldom included in the admission or discharge reports of patients with fractures of the hip for example. [7] The prevalence of osteopenia/osteoporosis and vitamin D deficiency in rather younger age groups and among males as much as in females could further confirm the concept about the possibility of an existing hidden environmental error which does not exclude an age group or dominates in a particular gender as traditional risk rules usually suggest as regards the challenge of osteoporosis/vitamin D deficiency. This could be furthermore a good answer for a perfect question; has vitamin D deficiency become an epidemic!! or is it real, vitamin D deficiency is pandemic!! [46]As long as some investigators have referred to the correlation between the prevalence of H. pylori and the frequency of osteopenia/osteoporosis and vitamin D deficiency, hence the matter is not altogether hidden; those investigators who missed to indicate this relation were looking for gastric H. pylori strains employing upper endoscopy but missed to fetch for the colonic strains. Therefore; the truth which is hidden in this subject is the responsibility of the colonic H. pylori strains but not the gastric strains on the challenge of osteoporosis/vitamin D deficiency and that the major factor behind the frequency and the dramatic flare up of the phenomena of osteoporosis/vitamin D deficiency during late decades is H. pylori not other traditional factors such as lack of sun exposure for example; the influence or impact of traditional risk factors on vitamin D deficiency should be rather similar during latest decades and previous decades. This suggestion is supported by the observational findings in the 5 groups of vitamin D deficiency in spite of sufficient sun exposure constituting the main motive of this study as 60% at least among them were supposed to have good nutrition advantages in addition. Accordingly, what is hidden in the subject is the combined influence of colonic H. pylori strains on vitamin D absorption and the onset/progress of osteoporosis. In brief, traditional risk rules remain insufficient to explain the flare up of vitamin D deficiency and osteoporosis during these latest decades on the basis of lack of sun exposure alone which could further indicate that all efforts to control the challenge via employing traditional measures alone would never be adequate or successful without elimination of a newly-existing underlying pathological error. What is also hidden is the false impression that H. pylori existence does not constitute a risk factor for osteoporosis depending on the findings that eradication of H. pylori employing antibiotics does not improve the risk of osteoporosis, on the contrary antibiotic eradication might increase it. That is simply because antibiotics are not effective against gastric H. pylori strains except forcing them to migrate to the colon; thus antibiotic eradication would increase the possibility for development and progress of osteoporosis. [20, 34, 43, 44] What is also missed in the subject is the fact that existence of H. pylori strains in the stomach is natural existence and gastric H. pylori strains even including abnormal behavior within the stomach such as its presence inside the gastric lumen during presence of food would not have distant pathologic sequels beyond the stomach. It is the major existence of H. pylori strains in the colon which could influence distant remote adverse effects in the body or it is the co-existence of gastric and colonic strains which is the commonest situation; colonic stains are the pathogens while the gastric are mostly not, investigators are searching for the gastric strains only and get mixed up about the undesirable sequels of H. pylori existence in general. [21, 42] What is also hidden and commonly missed in this subject is a common un-realized therapeutic nutritional mistake in recommending low-fat milk products for the purpose of improving dyslipidemia. [28] It has been demonstrated that the reason behind the conflict of dyslipidemia during late decades is mostly colonic due to major existence of H. pylori strains in the colon but not the traditional dietary reasons of eating full-fat products. It has been further reported and confirmed that food or specifically fat of the food is innocent as concerns the sequels of dyslipidemia namely the increased serum level of cholesterol and triglycerides; the pathogenesis of dyslipidemia is essentially metabolic not dietary due to intake of full-cream food products. [47-50] Milk products include two components which are having biological correlation with each other which are the fat content and lactic acid content. The fat contains the fat-soluble vitamins (A, D, E and K) while lactic acid is a healthy stuff. Lactic acid is digestive and works to behave the abnormal behavior of gastric H. pylori strains as much as the vinegar does; it was found that bio-organic acids such as lactic, formic and acetic inhibit bacterial growth on solid culture media with the lactic acid demonstrating the maximum inhibition. [51] It was also reported that addition of pyruvate inhibits H. pylori growth on culture media and this inhibition was attributed to accumulation of acetate, lactate and formate. [52] The reason for this biological inhibition is the fact that the pyruvate dehdrogenase complex is controlled by the rules of feedback regulation and product inhibition, [36, 37] hence these bio-organic acids could interfere with the energy metabolism of bacteria. As lactate is identified among the main metabolic products of glucose utilization, [53] therefore; inclusion of lactic acid in food would interfere with ability of the human body to gain energy from carbohydrates and the body becomes obliged to gain the energy from lipids. Furthermore, as much as vinegar mixed in salad could be used for slimming purposes through forcing the body for consumption of fat, [28] lactic acid content of milk products forces the body to consume the milk fat content and hence getting benefit of the vitamins dissolved in its fat. Therefore; lowering the fat content of milk products reduces the digestive, biological and vitamin supplement values without much benefit on dyslipidemia while in the meantime adding further insult towards vitamin D deficiency due to the poor vitamin D content of low-fat milk products. The striking association of colonic H. pylori strains with osteoporosis and vitamin D deficiency confirm that the existence of these strains in the colon could have a significant influence on the challenge of osteoporosis/ vitamin D deficiency during latest decades. It has been furthermore previously confirmed that the existence of H. pylori in the colon could compromise the fat-soluble vitamin D absorption via interference with lipid metabolism. [28] Therefore; these findings conform with the results of the current study to support the concept that colonic H. pylori strains could constitute a hidden reason behind the flare up of osteoporosis and vitamin D deficiency during late decades. The dilemma of H. pylori is essentially a sanitary conflict before it is a medical challenge, [20] sanitary problems are treated with sanitary measures and antiseptics but not antibiotics. The antibiotics violence towards H. pylori could lead to major migration of H. pylori to the colon and flare up of abnormal-existence/behavior of H. pylori strains. Existence of H. pylori in the colon is life-long unless eradicated, [20, 54] these abnormal-behavior H. pylori strains could travel from stomach to stomach via meals and even navigate between countries predisposing to spread of many reasons of chronic and major illness; [20, 21, 55] that could exactly constitute a grave environmental healthcare error. Therefore; eradication of H. pylori strains from the colon via natural measures could be an ideal effective and definitive measure to control the challenge of osteoporosis/vitamin D deficiency; improving vitamin D serum level and stopping progress of osteoporosis even without further vitamin D supplement therapy.Could osteoporosis be prevented!! The goal of treatment of osteoporosis is prevention of bone fractures by reducing bone loss or preferably by increasing bone density and strength. Although early detection and timely treatment of osteoporosis can substantially decrease the risk of future fractures, none of the available treatments for osteoporosis are complete cure. In other words, it is difficult to completely rebuild bone that has been weakened by osteoporosis. Therefore; prevention of osteoporosis is rather more important than treatment. [7, 8]Osteoporosis prevention: A dream, difficult to access!! But why not? Adequate screening might reveal that the majority of the increased frequency of osteoporosis developing in recent decades could be related to major existence of colonic H. pylori strains, these strains could be easily screened and eradicated employing natural measures; complications associated with these strains could be therefore avoided.A National Healthcare Program of Screening and Prevention could be suggested; mass screening of colonic H. pylori strains for population at risk of developing osteoporosis is in-expensive and possible or empirical colon clear upon developing frank colonic upsets or H. pylori dyspeptic symptoms is also easy, safe and healthy. Accordingly; existence of colonic H. pylori strains could be therefore raised as a new healthcare predictor for developing osteoporosis among population at risk. Prevention of osteoporosis is a challenge, treatment of osteoporosis is also a challenge and complications of treatments are further challenge; therefore, implementation of the concept of this study could give good promises for many patients at risk of osteoporosis. If further accurate re-determination is required for the wide practical application of the concept of this study, it should be done without much delay as it could save a lot of osteoporosis misery for so many people, impaired quality of life for many patients with fractures and save an adequate healthcare budget.
9. Conclusions
- A hidden truth in the challenge of osteoporosis/vitamin D deficiency could lie in the prevalence and major existence of H. pylori strains in the colon that could lead to a significant double influence on the development of both osteoporosis and vitamin D deficiency accounting for the main world’s burden of this challenge during latest decades not lack of sun exposure. Whereas gastric H. pylori strains even including abnormal behavior within the stomach seem rather innocent as regards the conflict of osteoporosis/vitamin D deficiency. Eradication of H. pylori strains from the colon via natural measures could be therefore an effective and definitive measure for the control of the challenge of osteoporosis and vitamin D deficiency worldwide; improving serum vitamin D level and protecting from an onset of osteopenia or stopping further progress of osteoporosis even without an additional vitamin D supplement therapy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML