-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2017; 7(0): 350-355
doi:10.5923/j.ajmms.20170710.02

Time for Recovery of Symptoms after Septoplasty
Abdullah Alotaibi1, Bassam Ahmed Almutlaq2, Hussain Gadelkarim Ahmed2
1Department of Otolaryngology Head and Neck Surgery, College of Medicine, Hail of University, Saudi Arabia
2College of Medicine, University of Hail, Saudi Arabia
Correspondence to: Hussain Gadelkarim Ahmed, College of Medicine, University of Hail, Saudi Arabia.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Nasal obstruction is one of the mutual clinical presentations that otorhinolaryngologists faces in every day practice. Deviated nasal septum (DNS) is one of the most frequent reason for the nasal obstruction. Therefore, the aim of the present study was assess the suitable timing for recovery of nasal obstruction associated complications after Septoplasty. Methodology: This study included a series of 104 patients presented with nasal obstruction and subsequently undergone septoplasty. Several nasal obstruction clinical complains were evaluated after 3 months and one year of septoplasty. Results: Statistically significant improvement with increase of time has been achieved in nasal blockage, breathing distress, sleeping distress, nasal congestion, exercise, and other complications. Conclusion: A significant improvement of nasal obstruction associated complications start after 3 months of Septoplasty but ultimate benefit may occur after one year.
Keywords: Septoplasty, Nasal blockage, Nasal obstruction, Breathing distress, Nasal congestion, Sleeping distress
Cite this paper: Abdullah Alotaibi, Bassam Ahmed Almutlaq, Hussain Gadelkarim Ahmed, Time for Recovery of Symptoms after Septoplasty, American Journal of Medicine and Medical Sciences, Vol. 7 No. 0, 2017, pp. 350-355. doi: 10.5923/j.ajmms.20170710.02.
1. Introduction
- Obstructed nasal breathing can occur due to deviation of the nasal septum [1]. Nasal obstruction is one of the most common problems in otolaryngology practice. Nasal obstruction can be caused by several factors such as deviation of nasal septum, nasal valve collapse, turbinate hypertrophy and nasal polyposis [2]. Among them, septum deviation is the main etiologic factor and more than half of the population have this problem [3, 4].Septoplasty is one of the most frequently performed otorhinolaryngological procedures which might be very challenging for the surgeon [5]. Successful septoplasty involves accurate assessment of septal pathology and sound technique to avoid persistent symptoms and new complications [6]. An accurate preoperative diagnosis of pathologies of the septum in the context of the nasal cavity is essential for the success of surgery. Intraoperative visualization through microscope or endoscope is very helpful for the surgeon and for the training of the residents. The modern technique of septoplasty with the phases of approach, mobilization, resection/repositioning and reconstruction/fixation is presented. Furthermore, the extracorporeal septoplasty in extreme deviations of the septum and alternative techniques for use in cases with limited pathologies as well as aspects of septoplasty in children are discussed. As particularly pathologies of the caudal septum are responsible for failures of septal surgery, some special problems of this region such as the vertical fracture of the caudal septum, the lack of caudal septum or anterior convexities of the cartilaginous septum are argued [5].Most studies show that objective measures to quantify and determine surgical success in the treatment of nasal obstruction do not correlate with subjective improvement as reported by patients [7]. Since there are many septoplasty procedures, each with its limitations, a variety of postoperative complications, which might be associated with preoperative complaints or associated with the surgical modification can occur. Therefore, the aim of the present study was assess the suitable timing for recovery of nasal obstruction associated complications after Septoplasty.
2. Materials and Methods
- This study included a series of 104 patients presented with nasal obstruction and subsequently undergone septoplasty. Archives related to all patients selected for septoplasty between 2012 and 2017 were retrieved from ear, nose, throat (ENT) department, King Khalid hospital in Hail, Northern Saudi Arabia. Patients’ medical records were investigated, and patients with a history of rhinoplasty, cranial and facial trauma or bone deformity (except DNS), and patients with a mass in the nasal cavity were excluded from the study. Only patients with apparent nasal obstruction related clinical presentation (complains) were considered. Several nasal obstruction clinical presentations were recorded included: nasal congestion, nasal blockage, breathing distress, sleeping distress, and exercise unease. Demographical characteristics including; age, gender and residence were also recorded.The different initial clinical presentations and complications were compared after three one year of septoplasty.Ethical consentOur study protocol was conformed according to the 2013 Declaration of Helsinki and this study was approved by ethics committee of College of Medicine, University of Hail, Saudi Arabia.Statistical analysisStatistical analysis was performed using SPSS software for Windows (version 16.0, SPSS Inc., Chicago, IL, USA). Categorical variables are given as frequencies and percentages, and continuous variables. For all statistical comparisons, a p value below 0.05 was considered statistically significant.
3. Results
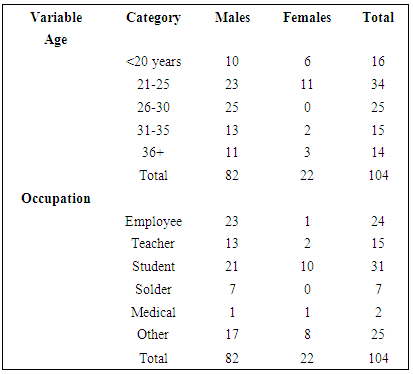
- The present study examined records of 104 patients presented with different clinical complains related to nasal obstruction. Out of the 104 patients, 82/104(78.8%) were males and 22/104(21.2%) were females, giving males' females' ration of 3.73: 1.00. The ages of the patients ranging from 17 to 42 years with a mean age of 27 years old. The majority of the patients were at age group 21-25 years followed by 26-30, and <20 years, representing 34/104(32.7%), 25/104(21.9%) and 16/104(15.4%), respectively. For males most of them were at age range 26-30 years followed by 21-25 and 30-35 years constituting 25/82(30.5%), 23/82(28%) and 13/82(15.9%) correspondingly. For females most of them were at age range 21-25 years followed by <20 and 36+ years constituting 11/22(50%), 6/22(27.3%) and 3/22(13.6%) correspondingly, as indicated in Table 1, Fig 1.
|
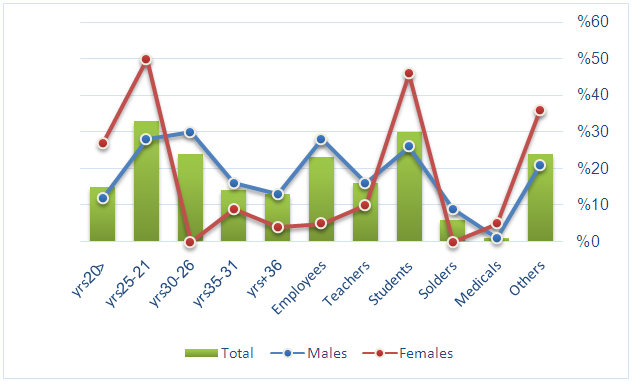 | Figure 1. Description of the study subjects by demographical characteristics |
|
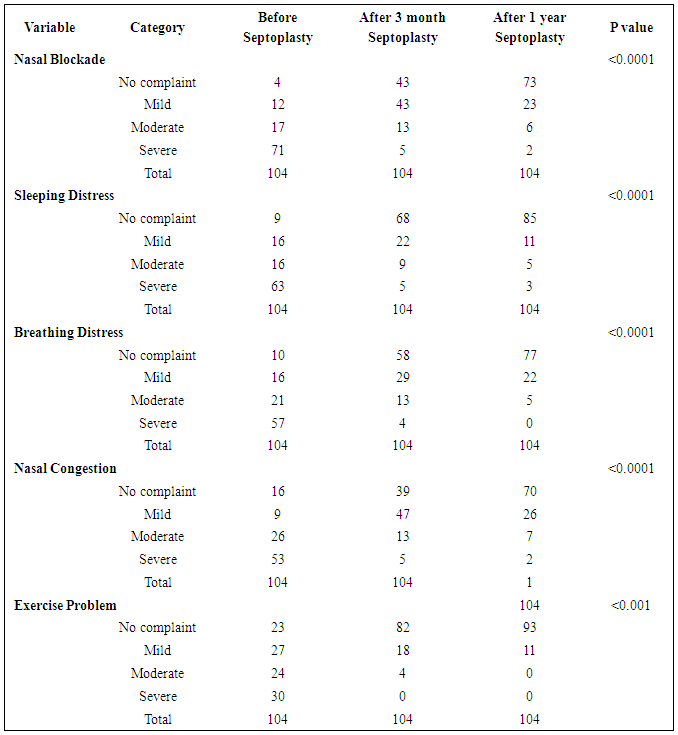
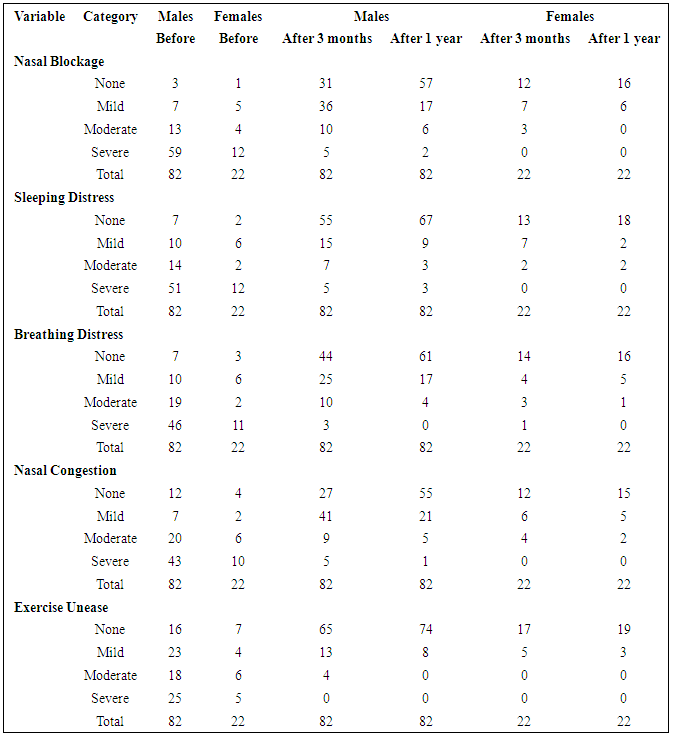
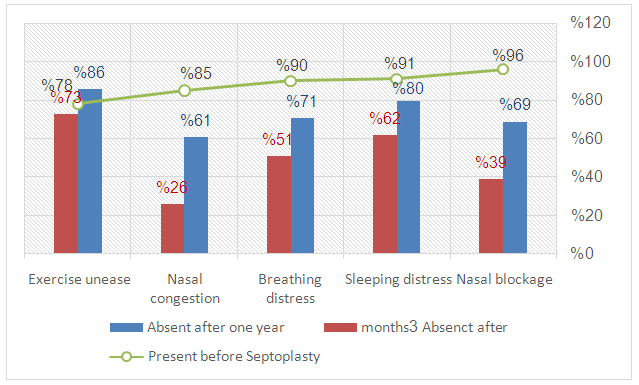 | Figure 2. Description of patients by clinical symptoms at initial presentation, after 3 months and after one year of septoplasty |
|
4. Discussion
- Nasal airway obstruction can be a source of discomfort and can have a significant impact on daily life. Nasal obstruction may lead to difficulty in breathing, eating, speaking, sleeping and overall physical activity of an individual. Septoplasty is a treatment of choice to relief these complains particularly when the obstruction is associated with DNS. In most instances the timing for recovery from these symptoms is chiefly depends on Septoplasty method involved. Outcome analysis is one vital mean for the evaluation of quality of medical carefulness. It assesses to what level the aims of medical care have been succeeded. Miscellaneous approaches are in use to execute this task. In the present study assess the suitable timing for recovery of nasal obstruction associated complications after Septoplasty. Three sets of nasal obstruction related complications associated data were compared to find out the suitable timing to a chief ultimate recovery of initial symptoms after Septoplasty. After three months of septoplasty we found statistically significant improvement of all assessed initial clinical complications (P <0.001). Many factors have been involved in the determination of the outcomes of Septoplasty. Procedures used for the diagnosis and treatment of DNS vary according to indications for the procedure and surgeon option, which in turn determine the fast or delayed recovery of obstruction symptoms [8]. Studies have shown that nasal obstruction clinical presentations start to recover after 15 days of septoplasty [9, 10]. However, great improvements have been achieved after one year of septoplasty in all obstruction related symptoms, but with high number nasal deformities. Some patients suffer from persistent obstruction after their primary septoplasty and may undergo a revision septoplasty to improve their nasal passageway It was found that a significant number of patients who undergo revision septoplasty also have nasal valve collapse. Thus it was recommended that in addition to septal deviation and inferior turbinate hypertrophy, nasal valve function be fully evaluated before performing septoplasty. This will help to ensure a complete understanding of a patient's nasal airway obstruction and, consequently, appropriate and effective surgical intervention [11]. However, the effectiveness of septoplasty for nasal obstruction in adults with a deviated nasal septum remains uncertain [12]. Scientific evidence is scarce and inconclusive, and internationally accepted guidelines are rare. There is a discrepancy between the occasionally heard opinion that septoplasty is an easy operation and its relatively high failure and complication rates [13].This clinical agreement declaration was developed by and for otolaryngologists and is anticipated to inspire evidence-based care for patients undergoing septoplasty with or without inferior turbinate reduction. A complete definition of septoplasty with or without inferior turbinate reduction was first developed, and extra statements were consequently produced and assessed addressing diagnosis, medical managing prior to septoplasty, and surgical considerations, as well as the proper role of perioperative, postoperative, and adjuvant measures, in addition to outcomes. Moreover, a series of clinical statements were developed, such as "Computed tomography scan may not precisely demonstrate the degree of septal deviation," "Septoplasty can assist delivery of intranasal medications to the nasal cavity," "Endoscopy can be applied to enhance visualization of posterior-based septal deviation during septoplasty," and "Quilting sutures can obviate the need for nasal packing after septoplasty." It is expected that the application of these guidelines will result in reduced discrepancies in the care of septoplasty patients and an upsurge in the quality of care [14].Although most of the initial clinical complications were subsided or diminished to mild symptoms, but patients satisfactory represent the major challenge. Although septoplasty offers sufficient correction of septal deviation, patients are not always satisfied with the procedure [15]. The level of satisfaction after Septoplasty may be influenced by individual differences in the perception of one's nasal passage changes and emotional factors. Thus of the limitations in the present study, the studied variables were less measureable.
5. Conclusions
- Maximum recovery of symptoms associated nasal blockage can be achieved after one years of Septoplasty, through significant improvement can be acquired after three months. Individual perceptual variances of air passage modifications and emotional factors do not guess biased symptom enhancement after septoplasty. However, initial clinical presentations were the only prognostic factor for patient contentment after septoplasty.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML