S. O. Tilemisov, F. A. Khadjibaev, M. A. Khashimov, R. O. Tilemisov
Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Treatment and diagnostics analysis of 1552 patients with obstructive jaundice of malignant genesis was carried out. At the first stage of investigation all patients were undergone mini-invasive methods of bile ducts decompression. The level of bile ducts lesion was specified by performing ultrasound diagnostics, magnetic resonance pancreato-cholangiography (MRPCG) before biliary decompression. Biliary decompression by retrograde method was performed at the localization of the process in the terminal part. When the timorous process was located in the proximal parts of the bile ducts we had carried out antegrade cholangiography with cholangiostomy. Complications after retrograde interventions were observed in 19% of patients and in 12.5% cases – after antegrade interventions. Total mortality after mini-invasive roentgen-endobiliary interventions made up 1.4%.
Keywords:
Obstructive jaundice, Tumor of caput pancreatic, Tumor of portal zone, Retrograde cholangio-pancreatography, Percutaneous transhepatic cholangiography, Cholangiostomy
Cite this paper: S. O. Tilemisov, F. A. Khadjibaev, M. A. Khashimov, R. O. Tilemisov, Mini-Invasive Roentgen Endobiliary Interventions at Obstructive Jaundice of Timorous Genesis, American Journal of Medicine and Medical Sciences, Vol. 7 No. 8, 2017, pp. 309-312. doi: 10.5923/j.ajmms.20170708.01.
1. Background
The growth of malignant diseases of hepato-pancreato-duodenal zone (HPDZ) for the recent years leads to a significant increase of patients quantity with obstructive jaundice (OJ) which is developed in 75-95% of cases [1-4]. The most frequent cause of OJ development is pancreas cancer (54-72%). The following causes of OJ development also are: major duodenal papilla cancer (18.3%); tumors of extrahepatic bile ducts (15%); gallbladder carcinoma (up to 13%). At present time the only radical treatment method of HPDZ malignant tumors remains a surgical one. Resectability by various data does not increase 10-17% [1-3]. Operability is mainly determined by the absence of tumor prevalence to the adjacent with main vessels. Therefore, at observation and levels of treatment tactics choice it is important to have an information allowing to see an interrelation of the tumor with adjacent organs and main vessels: aorta, celiac trunk, splenic and superior mesenteric arteries, superior mesenteric and portal veins. Patients with OJ usually admit by ambulance service. The urgent issue is emergency resolution of OJ by performing biliary decompression. The presence of OJ in majority of cases is evidence on the 3rd-4th stage of timorous process and that is why surgical intervention can be performed only in 5-25% of patients [4-5]. Surgical intervention conduction at the peak of OJ is followed by the high postoperative lethality due to hemo- and homeostasis abnormalities. It is necessary to eliminate OJ by mini-invasive and safety method. Preoperational drainage of the bile ducts allows to cut short manifestations of OJ and to perform further planned surgical intervention in more “advantageous” conditions both for a surgeon and for a patient. Such treatment tactics with preliminary mini-invasive reduction of OJ decreases the quantity of postoperative complications and lethal outcomes. In inoperable patients (due to the local prevalence of the tumor or at the presence of disseminated lesion) mini-invasive methods of internal cholepoiesis restoration is either ultimate treatment method undertaken with symptomatic purpose or provide a possibility for conducting special (chemo- radiation) therapy. A sufficient experience on using different endovascular methods in the cure of OJ of malignant genesis has been accumulated by nowadays, but methodical aspects of prevention and treatment issues of complications and side effects at undertaking biliary decompression still remain untaken up [2, 5].
2. Goal
To improve direct treatment results of the patients with HPDZ organs cancer complicated with OJ by the way of working-out the indications for different types of bile ducts drainage and their differentiated use subject to the condition of patients severity, location and stage of the tumor in the conditions of emergency medicine.
3. Material and Methods
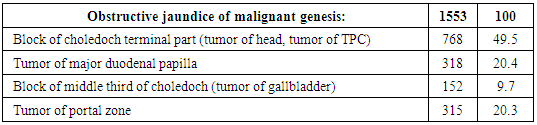
An experience of diagnostics and treatment of 1553 patients by OJ of malignant genesis was performed. Diagnostic and treatment algorithm subject to the cause of OJ has been presented on the base of received data. The most rational sequence of radial and endoscopic methods of diagnostics, the choice of the bile ducts decompression ways as the first treatment stage at the obstructive jaundice (OJ) syndrome were defined. The analysis of history cases of 1553 patients with OJ who were cured at the department of emergency surgery of the Republican Research Centre of Emergency Medicine has been carried out. Men were 908 (58.5%), women - 645 (41.5%). The patients’ age varied from 17 to 89 years, more than 60% were the patients of elderly and old age burdened by concomitant pathology and a high operational risk. 60% of patients had a severe level of jaundice (bilirubin level made up more than 250.0 micromole/l). Table 1. The causes of obstructive jaundice
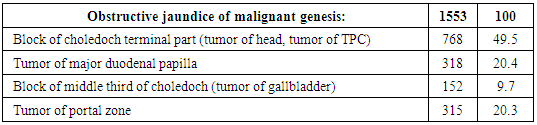 |
| |
|
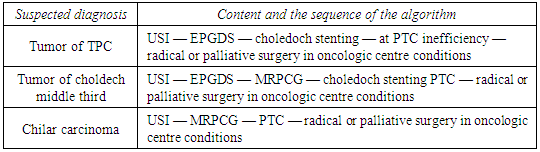
Independently from obstructive jaundice etiology the main patho-physiological links of the syndrome are similar and it allows to be guided by a single treatment-diagnostic tactics. The choice of instrumental method of the diagnostics is determined by estimated cause of OJ obturation, ability of diagnostic investigation continuation to medicinal intervention, technical equipment of the hospital and the availability of the qualified specialists. Patients treatment was carried out with the use of traditional, endo-video-surgical and mini-invasive interventions on the background of the conservative therapy, mainly directed to the prevention of hepatic and renal insufficiency. Being an emergency condition OJ requires a rapid diagnosing and decompression of the bile ducts: all patients performed the whole complex of procedures during the first 24 hours including clinical and biochemical analysis, ultra sound investigation (USI), Esophago-gastro-duodenoscopy (EPGDS) with the observation of MDP zone. At the suspicion on the timorous genesis jaundice (by clinical-anamnestic and USI data) we performed computer tomography (CT) which allowed to confirm a diagnosis of tumor. A capacity of performing magnetic resonance pancreato-cholangiography (MRPCG) has been recently available (fig.1).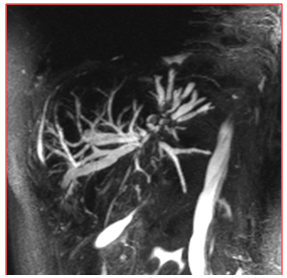 | Figure 1. MRPCG. Dilatation of intrahepatic bile ducts and choledoch |
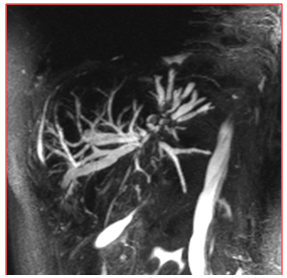
The most informative method of the diagnostics is a direct opacification of the bile ducts. Endoscopic retrograde pancreato-cholangiography (ERPCG) is a method of choice (fig. 2) which allows to get a correct diagnosis in 79-98% of cases [10-12]. | Figure 2. ERPCG. Tumor of choledoch terminal part with choledochectazia |
1298 of ERPCG were totally performed from 2004 to 2016. It was not always practicable due to the presence of the pathology (tumor invasion to the duodenum lumen) or some anatomic features (the presence of paraphateral diverticulum) in TPC and in postbulbar part of duodenum. In 120 (9.2%) patients retrograde intervention was used as diagnostic procedure. In 312(24%) cases we carried out an endoscopic papilla-sphincterotomy (EPST), in 720(55.4%) cases – stenting of choledoch, in 128(9.8%) patients we performed restenting of the choledoch due to recurring admission because of the stent obstruction. Nazobiliary drainage of choledoch was performed in 18(1.4%) cases.
4. Results and Discussions
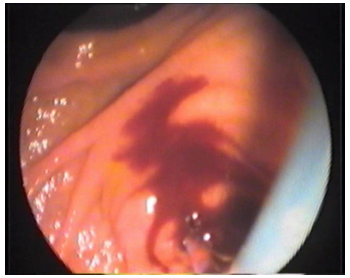
Being the invasive methods ERPCG and EPST sometimes bring on complications. According to our reports ERPCG and EPST were followed by some complications which arose both during the surgery and in the postoperative period. The most frequent complication of ERPCG and EPST was a hemorrhage from papillotomic wound (fig.3.). | Figure 3. Hemorrhage from papillotomic wound |
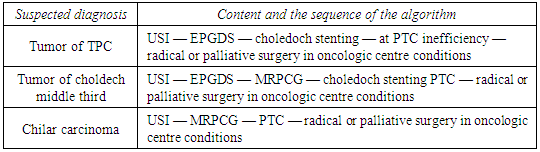
Hemorrhage occurred in 150(11.5%) patients from the cut area at performing EPST. In 136 cases bleeding was insignificant and stopped without any assistance. In 14(1.1%) patients the hemorrhage was massive and in 4 cases it was stopped by the local and general hemostatic manipulations, in 10 cases it required laparotomy to stop bleeding. The prevention of hemorrhage is consisted in patient’s preparation: introduction of hemostatics the day before the surgery, a phased EPST in the complicated cases with the interval of 3-6 days.The second frequent complication after retrograde intervention is acute pancreatitis (AP). It frequency varies from 2 to 10% by different literary data and lethality makes up 0.2-1.5% [13-15]. The light pancreatitis occurred in 60(4.6%) patients. Pancreatonecrosis was developed in 5 (0.3%) cases and it required an operative intervention. We consider that the following measures are effective for prevention AP after ERPCG and EPST: a correct preparation for investigation, an adequate and effective premedication, sparing operation, adequate and rational therapy after the surgeries. The next frequent complication is a cholangitis [16-18]. In our observations a purulent cholangitis occurred in 25(2%) patients after RPCG due to the location of timorous process in portal area and unsuccessful stenting. Those patients were undergone percutaneous transhepatic cholangiography (PTC) for relief of cholangitis. Perforation of duodenum with catheter and with the development of retroperitoneal phlegmon which required operative treatment was registered in 7 (0.5%) cases. At the impossibility of the drainage of the biliary tree by retrograde method or at the presence of the “high block” of OJ (tumor at the portal zone) we carried out antegrade puncture drainage of the bile ducts - percutaneous transhepatic cholangiography (PTC). PTC was performed in 255 patients. This procedure gives a possibility of carrying out a fistulography for correction a diagnosis and also to prepare a patient for radical surgery or to improve life quality in incurable cases. We used the Bismuth-Corlette standard classification for detecting the level of lesion and the tactics of percutaneous drainage. In more than 55% of patients the tumor was located in the portal zone. At the antegrade cholangiography it was detected that the causes of OJ were: tumor of pancreas head and TPC - in 84 patients, choldech tumor by Bismuth-I was registered in 39 cases, chilar carcinoma by Вismuth –II was observed in 36 cases, chilar carcinoma by Вismuth-II – in 54 patients, chilar carcinoma by Вismuth-IV – in 42 patients. Those patients were performed: PTC with external drainage of choledoch was performed in 154(60,4%) cases, external-internal drainage of choledoch - in 81(31.7%) cases, percutaneous transhepatic (PT) endoprosthesis - in 16(6.3%) patients. 4(0.1%) patients were performed PT plugging of puncture channel due to the hemorrhage which was occurred during PTC. Complications after PTC arose in 32(12.5%) patients: hemobilia - 16(6.3%), hemorrhage from the puncture channel - 5(2%) cases, gallbladder perforation – in 1(3.9%) case, drainage dislocation - 3(1.2%), hepatic failure - 7(2.7%) cases. General lethality after ante- and retrograde endobiliary interventions made up 22(1.4%) cases: retroduodenal perforation with retroperitoneal space phlegmon - 7(0.4%), purulent cholangitis with sepsis development - 4(0.2%); hepatic-renal failure - 7(0.4%); cardiac infarction -1(0.06%); hemorrhage from EPST - 1(0.06%); intra-abdominal hemorrhage arose due to portal vein injury during PTC - 1(0.06%); drainage dislocation, biliary peritonitis, sepsis - 1(0.06%). The terms of conducting surgical interventions depend on initial severity of hepatic failure and make up 1-4 weeks. As a rule, one of the basic landmark showing a clear tendency to the resolution of cholestasis and a possibility of performing a surgery is a drop of general bilirubin below 50 Mmole/l. The analysis of our investigations allowed us to determine the most rational sequence of the use of diagnostics and treatment tactics methods at the obstructive jaundice (table 2).Table 2. Diagnostics and treatment tactics algorithm at the obstructive jaundice
 |
| |
|
5. Conclusions
1. Treatment results of OJ can be improved by the use of different mini-invasive methods the main goal of which is not only a diagnostics but also a treatment which is performed simultaneously.2. Temporal decompression of the bile ducts should be performed at the first stage of treatment as a preparation to the basic (second) stage and in some cases – as a complete change of surgical treatment. 3. ERPCG with stenting is a method of choice at the detection of malignant formation in the distal part of choledoch; PTC with external bile excretion – at the detection of proximal blocks. 4. The knowledge of possible complications after mini-invasive interventions, their frequency and development allow to reduce a quantity of postoperative complications and to improve the prognosis of the disease.
Abbreviation
Hepato-pancreato-duodenal zone (HPDZ) Obstructive jaundice (OJ) Terminal part of choledoch (TPC) Major duodenal papilla (MDP) Esophago-gastroduodenoscopy (EPGDS) Magnetic resonance pancreato-cholangiography (MRPCG) Endoscopic retrograde pancreato-cholangiography (ERPCG) Endoscopic papillosphincterotomy (EPST) Percutaneous transhepatic cholangiography (PTC)
References
| [1] | Dolgushin B.I., Patyutko Yu. I, Nechipay A.M. et. Antegrade endobiliary interventions in oncology. M.: Practical medicine, 2005. P.176. |
| [2] | The guide on surgery of liver and bile ducts // Ed. by A. E. Borisov. St-Petersburg., 2003.- V.2.- p.281-348. |
| [3] | The guide on surgery of bile ducts // Ed. by E.I. Galperin, P.S. Vetshev. |
| [4] | Aksel E. M. Morbidity by malignant neoplasms and mortality of CIS countries population in 1998 // М. 2000. - p.270. |
| [5] | Altiev B.K., Atadjanov Sh.K., Khoshimov M.A., Baynazarov I.Kh. Endovisual interventions at cholelithiasis complicated by obstructive jaundice and cholangitis. Materials of the 7th Rep. scientific conference. Tashkent. 2007; p.571. |
| [6] | Aripova N.U., Ismailov U.S., Nazarov E.I. et al. Mini-invasive methods in the urgent surgery of the biliary system. Annals of Surg Hepatol 2003; 2: 259-260. |
| [7] | Khadjibaev A.M., Alidjanov F.B., Aripova N.U et al. Endoscopic interventions in the treatment of residual and recurrent choledocholithiasis. J Surgery 2006, № 12. - p. 27-29. |
| [8] | Karimov Sh.I., Akhmedov R.M. Endobiliary interventions in the diagnostics and treatment of patients with obstructive jaundice. Tashkent. Press named after Abu Ali ibn Sino 1994; 240. |
| [9] | Izrailov R.E., Kuleznyova Yu.V. Antegrade endobiliary interventions in the treatment of patients with obstructive jaundice of timorous genesis // Clinical technologies. 2007. - №1. — p.20. |
| [10] | Patyutko Yu.I, Kotel’nikov A.G. Surgery of biliopancreoduodenal zone organs cancer. M.: «Medicine». - 2007.-p.448. |
| [11] | Yee A.C.N., Ho Ch.S. complication of percutaneous biliary drainage: benign vs. malignant diseases //AGR. -1987; 148: 1207-1209. |
| [12] | Blokhin N.N., Intin A.B., Klimenkov A.A. Pancreas and bile ducts cancer //М.: Medicine. 1982. - p.259. |
| [13] | Davidov M.I., Aksel E.M. Morbidity by malignant neoplasms and mortality of CIS countries population in 2005. ttp://www.ronc.ru/files/3479/. |
| [14] | Khadjibaev F.A., Baymuradov Sh.E., Khashimov M.A., Eshmuradov A.B. //Complications of endoscopic transpapillary interventions at the treatment of obstructive jaundice of timorous genesis // Materials of the plenum of the court of the association of hepatopancreatobiliary surgeons of CIS countries. 2016.-p.112. |
| [15] | Namdar T, Raffel AM, Topp SA. Et al. Complications and treatment of migrated biliary endoprostheses: a review of the literature // World J Gastroenterol. 2007 Oct. - Vol. 28. - P.5397- |
| [16] | Saltz LB, Cox JV, Blanke C, Rosen LS, Fehrenbacher L, Moore MJ, f. |
| [17] | Varker KA, Martin EW, Klemanski D, Repeat Transarterial Chemoembolization (TACE) for Progressive Hepatic Carcinoid Metastases Provides Results Similar to First TACE, J Gastrointest Surg. 2007 Dec; ll(12): 1680-1685. |
| [18] | Brown BD, Geschwind JF, Soulen MC, et al. Society of interventional radiology position statement on chemoembolization of hepatic malignancies. J Vase Interv Radiol 2006; 17: 217-223. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML