-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2017; 7(6): 229-237
doi:10.5923/j.ajmms.20170706.01

The Effect of Tai Chi on Functional Lower Extremity Mobility and Strength, Ankle Proprioception, and Postural Adaptation in Older Adults
Anshul Jain1, Jane Taylor1, Paolo Sanzo1, 2, Carlos Zerpa1
1School of Kinesiology, Lakehead University, Thunder Bay, Canada
2Northern Ontario School of Medicine, Lakehead University, Thunder Bay, Canada
Correspondence to: Paolo Sanzo, School of Kinesiology, Lakehead University, Thunder Bay, Canada.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: The purpose of this study was to examine the effects of a 10-week Tai Chi program on functional lower extremity mobility and strength, ankle proprioception, and postural adaptation in older adults. Subjects: Thirty-two participants ranging in age from 57 to 79 years (M = 66.5, SD = 4.94) were recruited to participate in the study. Methods: Seventeen of these participants were allocated to a Tai Chi group and 17 participants to a control group. Baseline testing for each dependent measure related to functional lower extremity mobility and strength, ankle proprioception, and postural adaptation was completed. Functional lower extremity mobility was assessed by recording the amount of time participants took to complete the Adapted Timed Up and Go Test (ATUGT). Functional lower extremity strength was assessed by recording the number of repetitions of getting up and sitting down repeatedly during the 30-Second Chair Stand Test. Ankle proprioception was examined with the use of a proprietary footplate to measure angular displacement at the ankle joint. Postural adaptation was assessed by examining postural sway on an Advanced Mechanical Technology Incorporated© force platform. After completion of the baseline measures, participants in the Tai Chi group attended a supervised Tai Chi training program led by a trained Tai Chi trainer twice weekly for 60 minutes over a 10-week period. The 17 participants in the control group, however, continued their daily regular activities and were asked not to practice Tai Chi during the study period. Post-treatment assessment was completed after the 10-week program. Participants in the control were offered the opportunity to attend these classes after the post-treatment data collection was completed. Pre- and post-treatment data for each of the dependent variables were analyzed using 2 (groups) X 2 (time) mixed factorials analysis of variance with repeated measures on time. Results: There was a significant interaction effect between group and time in which the Tai Chi group improved for backward angle ankle joint proprioception (F(1, 30)=16.53, p=.001, ƞ2=.36). There was also a significant main effect for functional lower extremity strength (F(1, 30)=12.07, p=.002, ƞ2=.29) with both groups increasing in the number of chair stand repetitions. There was also a significant main effect and reduction for the ATUGT turning time (F(1, 30)=8.98, p=.005, ƞ2=.23) and sitting on a chair and walking 2 meters time (F(1, 30)=15.56, p=.001, ƞ2=.34). Conclusion: Tai Chi can be a viable alternative to traditional exercise programs to improve overall health, mobility, strength, and possibly be an adjunct to aid in falls prevention programs.
Keywords: Tai Chi, Mobility, Strength, Proprioception, Posture
Cite this paper: Anshul Jain, Jane Taylor, Paolo Sanzo, Carlos Zerpa, The Effect of Tai Chi on Functional Lower Extremity Mobility and Strength, Ankle Proprioception, and Postural Adaptation in Older Adults, American Journal of Medicine and Medical Sciences, Vol. 7 No. 6, 2017, pp. 229-237. doi: 10.5923/j.ajmms.20170706.01.
Article Outline
1. Introduction
- Tai Chi is an increasingly popular form of multi-modal mind body exercise developed in ancient China and is characterized by its meditative and relaxing effect induced by slow, gentle, rhythmic, and graceful movements [1]. The movements of the upper and lower extremities are also then coordinated with one’s breathing pattern [2] and incorporate dynamic weight shifting and single limb support with imagery, body awareness; cognitive, social, and meditative components [3].Tai Chi has been reported to be a safe [4] and beneficial exercise improving strength, endurance, flexibility, and balance [2, 5, 7]; it has also been reported to provide moderate aerobic, agility, and mobility training [3]. Fall prevention studies have also proposed the possible efficacy of Tai Chi on older adults in reducing the fall rate, risk of falls, and fear of falling [8, 9]. Recent systematic reviews have also proposed enhanced cognitive functioning [3]. The learning of the choreographed movement patterns and multi-modal stimulation affect visual spatial processing, processing speed, memory, attentional focus, and multi-tasking [3]. Despite all of these documented effects of Tai Chi practice, its clinical implication in fall prevention programs has not been clearly demonstrated. Although some studies have been conducted to determine the effects of various exercises on fall prevention, to date, little has been confirmed about Tai Chi specifically, even though it is commonly used as a recreational activity by older adults. Tai Chi’s slow and relaxing movement patterns may be practiced individually or in a group, which is helpful in promoting social interaction. After learning the basic movements, Tai Chi can be practiced in different locations such as individually at home or community based recreational parks or gyms [5-7]. Tai Chi movements are simple, coordinated, dance like movements and can be easily adopted after a couple of training sessions. The information on the use of Tai Chi for other disorders is contradictory. It has been reported to be helpful with some disorders such as individuals with cardiovascular conditions or risk factors of cardiovascular disease [10], and effective for pain control in patients with knee osteoarthritis but not helpful in improving physical function [11]. Recent systematic reviews have either been inconclusive or stated no benefits of Tai Chi in individuals with osteoporosis [12, 13] and mixed results for Parkinson’s disease patients often limited by the quality and quantity of research available to date. Based on these qualities, Tai Chi has been proposed to enhance mobility, balance, and functional independence in older adults and may be a logical addition to exercise programs to achieve beneficial outcomes potentially reducing health related costs and reducing the fear of falling [14]. Approximately, one third of the population aged 65 years and over experience a minimum of one fall annually [15]. The consequences of these falls may be more severe in the elderly and are one of the most prominent causes of morbidity and mortality. Even a single fall may impair the functional mobility and psychological well-being of the individual resulting in restricted activities and prolonged immobility [16]. The short and long-term impact of elderly falls on the Canadian health care system is also widespread. From 2009 to 2010, over 53,500 Canadians aged 65 years and older were hospitalized due to falls with related injuries and direct health care costs totalling more than $2 billion [17]. It is anticipated that the number of elderly falls will increase as the total population aged 65 years and over continues to increase making up a greater percentage of the overall population [17]. As a result, it is imperative for healthcare providers to attempt to address some of the causes leading to a fall and potentially implement prevention strategies and solutions.Balance has been shown to be a good predictor of falls in the elderly population and is defined as the ability to maintain the body’s position over its base of support [18]. Conversely, the term proprioception is described as the sensory information that contributes to the perception of joint and body movement as well as the position of the body, or body segments, in space [19]. Joint position sense and the sense of limb movement are vital for the execution of smooth and coordinated movements and motor learning [16, 20]. Mion et al. [21] reported that impaired proprioception is one of the major predictors of falls in the elderly. Results of a recent study by Robinovitch et al. [22] suggested that the lack of proprioceptive awareness while taking the initial step was also responsible for the majority of falls observed in a long-term care setting. Balance, also plays a major role in the performance of daily functional tasks [23] and the maintenance of erect postures [24]. Balance is a complex skill that requires constant input from the visual, vestibular, and somatosensory systems in order to affect postural adaptation [25]. Due to age related declines in visual, vestibular, and proprioceptive inputs, it is often difficult for older individuals to maintain balance [26, 27].Multidimensional strategies such as active exercises, dietary supplements, pharmacological agents, orthotics, walking aids, and environmental modifications are widely used in fall prevention and rehabilitation programs for seniors [28, 29]. It has also been reported that active exercise is highly effective in reducing falls and preventing fall related injuries. Iwamoto et al. [30] reported a 17% reduction in falls risk in older adults participating in exercise programs that included balance retraining. Physical activities also emphasizing muscle strength, flexibility, and endurance training have been reported to be effective in preventing elderly falls [31]. In recent years, researchers have been attracted to targeted interventions for identified contributing factors. Most review studies have shown promising results of combined physical activities on elderly fall prevention [32]. Exercise interventions such as calisthenics, balance retraining, strength training, and Tai Chi have also been proposed as effective strategies for consideration [32]. Therefore, the purpose of this study was to determine the benefits of a 10-week Tai Chi training program on lower extremity functional mobility and strength, ankle joint proprioception, and postural adaptation in elderly participants.
2. Methods
- After obtaining ethical approval from the academic institution, 34 participants were recruited from the community via information posters displayed in health and fitness centres, as well as in senior activity centres. All potential participants were invited to attend an orientation session that provided a detailed understanding of the study. Participants were included into the study if he/she was a healthy, senior aged 55 years or older that had sustained at least one fall in the past 12 months. Participants were excluded from the study if he/she had any of the following impairments: dementia or cognitive decline that prevented understanding simple instructions; a progressive neurological disease (e.g., Parkinson’s disease); pre-existing severe lower extremity pathology, neurological disorder, or balance difficulty that prevented standing for the testing procedures with or without the aid of an assistive device (e.g., osteoarthritis, vertigo, dizziness, stroke, or epilepsy); any acute health condition (e.g., heart disease, uncontrolled angina, chronic obstructive pulmonary disease, or osteoporosis) that precluded participation in the Tai Chi program; and if the participant was currently actively engaged in a Tai Chi exercise program.Once the participant was enrolled into the study and provided written consent, a demographic, falls history, and Physical Activity Readiness questionnaire was completed. Afterwards, each participant was administered a baseline battery of tests examining functional mobility and strength, ankle joint proprioception, and postural control and adaptation that will be further described in detail. All tests were completed by a member of the research team that is a registered Physiotherapist.
2.1. Participants
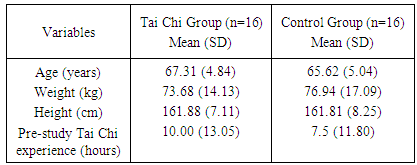
- Thirty-four participants aged 57 to 79 years (M = 66.5, SD = 4.94) began in the study. The participants were conveniently assigned to either a Tai Chi (n=17) or a control group (n=17). The average attendance for the entire Tai Chi training session was 87%. Six of the participants attended all 20 sessions. Two participants left the training midway; one after 8 sessions (for health reasons from the Tai Chi group) and the other after 10 sessions (due to travel commitments from the control group). Demographic information and descriptive characteristics for all participants are highlighted in Table 1.
|
2.2. Functional Lower Extremity Mobility
- Functional lower extremity mobility was examined using the Adapted Timed Get Up and Go Test (ATGUG). This test is similar to the Timed Up and Go Test [33, 34] that is commonly used to examine functional mobility in older adults. The ATGUG uses the overall time taken to complete the task and breaks down the time variable into each of the components of the required task. It has also been adapted for use in different types of populations [35, 36]. To conduct this test, the participant was seated and asked on command to get up from the chair, walk a distance of 3 meters, turn around, and walk back to the chair, and sit down. Each component of the test was timed and measured in seconds using a stopwatch. Time 1 [T1] referred to the rising time; time 2 [T2] referred to the walking time to get to the turn; time 3 [T3] referred to the time to complete the turn; time 4 [T4] referred to the walking time to get back to the chair; and time 5 [T5] referred to the time to return to sitting (see Figure 1).
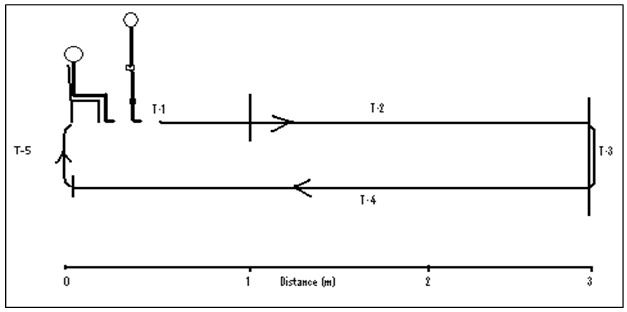 | Figure 1. Adapted Timed Get Up and Go Test |
2.3. Functional Lower Extremity Strength
- The 30-Second Chair Stand Test was used to measure the functional strength of the lower extremities as it is quick and easy to administer and has high test-retest reliability [37]. The participant was asked to sit on a straight backed chair without arm rests. He/she was then instructed to get up and sit down repeatedly for 30 seconds. The total number of repetitions completed was recorded and used to determine lower extremity functional strength.
2.4. Proprioception
- To test proprioception, a proprietary mechanical device with a mobile foot plate as shown in Figure 2 was used. The device was powered by an actuator motor, designed to move in either direction (ankle plantarflexion or dorsiflexion). This device was designed such that the motor was not visible (masked in a box) in order to elicit natural perceptions of movement from the participant. A linear actuator motor was attached to the foot plate resting on an axle. It was also equipped with a potentiometer, connected to a Power Lab unit via an analog to digital converter to measure the angle of the platform. The device was connected to a handheld switch, operated by the participant, to signal the perception of passive motion. The footplate was set at 0° prior to each trial, and the speed was gradually increased from 0° to 0.4° per second to move the platform in the desired direction of plantarflexion or dorsiflexion. Pilot testing of the proprietary mechanical device was completed to examine the reliability and validity of the device.The participant was advised to stand on the foot plate of the device and attempt to detect when the passive movement at the ankle joint occurred. Four practice trials (two forward and two backward) were completed to allow the participant to become familiar with the task. This was then followed by 9 trials that were recorded. After each trial, the participant was asked to step off of the foot plate so that the angle could be reset to 0°. During the test trials, participants were not informed about the direction in which the plate would move as this was under the control of the researcher. To randomize the sequence of direction, participants chose a unique direction order, from a set of cards. As the platform started and speed gradually increased up to the highest limit of 0.4° per second, the participant’s task was to sense the moving platform at the ankle joint and press the handheld switch when this motion was detected. The difference between the start and stop positions of the platform was calculated by measuring the difference between the starting joint angle and the stopping joint angle. During each trial, participants were also blindfolded and provided with headphones to eliminate visual and auditory stimuli that might assist in determining when the movement started and stopped. A random time delay for the motion of 2, 5, 7, and 9 seconds was also used for the 9 trials so that the participant did not know when the motion would begin.
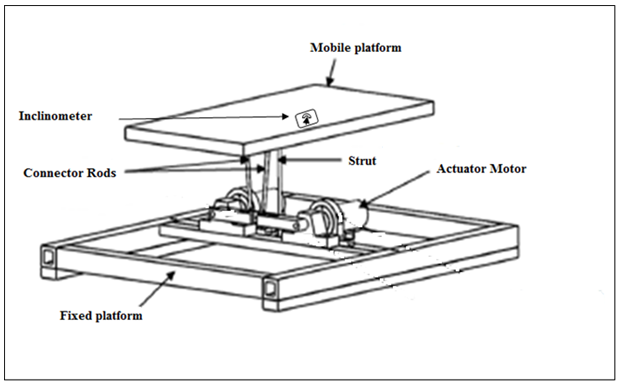 | Figure 2. Proprietary Proprioception Mechanical Device |
2.5. Postural Adaptation
- Postural adaptation was assessed by examining postural sway on an Advanced Mechanical Technology Incorporated© force platform. Postural sway can be defined as the phenomenon of constant horizontal movement and corrective positioning of the centre of gravity within the base of support [38]. During baseline testing, the foot size of each participant was traced on a piece of paper and his/her weight was recorded while standing barefoot on the force platform. Participants were first asked to stand statically. They were then asked to lean in a forward, backward, and right and left position while keeping their trunk straight and without lifting his/her toes or heels for the 20 second duration with the eyes open and the eyes closed. For quiet stance measures, the participant was requested to stand as still as he/she could for the 20 seconds while looking straight ahead at a marker located 10 feet away. This practice was followed by 3 trials completed with his/her eyes open and 3 trials with his/her eyes closed. For the balance space task, each participant was asked to lean forward, backward, right, and left as far as possible while keeping the trunk straight and without lifting his/her toes or heels for a 20 second duration. Three trials of each stance were recorded. The data collected from the AMTI© force plate included 3 forces (Fx, Fy, and Fz) and 3 moments (Mx, My, Mz) and were used to calculate the centre of pressure and postural sway. Centre of pressure and postural sway measures were interfaced with the AMTI BIOSOFT software and used to determine postural control and postural adaptation of the participants. The mean of 3 trials of area of sway, path length, mediolateral sway, and anteroposterior sway measures in each stance (eyes open, eyes closed, and balance space) was analysed. A member of the research team was always present to assist/protect the participants during testing to ensure safety.
2.6. Tai Chi Exercises and Control Group
- After the baseline testing was completed, participants in the Tai Chi group attended a supervised Tai Chi qigong training program led by a trained Tai Chi trainer twice weekly for 60 minutes over a 10-week period. The Tai Chi poses consisted of raise up and press down, open and closed hand, presenting the ball, hands stroke the beard, crane flying in the sky, Qi to dentian poses. The 16 participants in the control group continued their daily regular activities and were asked not to practice Tai Chi during the study period. An activity log was provided to all participants to record his/her physical activity during the study period and collected on a weekly basis for the duration of the study. This was completed to monitor the activity level of both groups. Post-treatment assessment was completed after the 10-week program. All of the participants in the control group were provided with the opportunity to complete the Tai Chi training after the post-treatment measures were completed. After 10-weeks, a post-treatment assessment of functional mobility and strength, ankle proprioception, and postural control and adaptation was completed as previously described and the difference between baseline measures analysed.
2.7. Statistical Analysis
- Data analysis was completed using SPSS software (Version 20). Descriptive statistics were used to compare the mean and standard deviations for individual demographics, functional mobility and strength, ankle proprioception, and postural sway measures. A 2 (Tai Chi training and control group) X 2 (pre- and post-treatment) mixed factorial ANOVAs with repeated measures on time were conducted to examine the interaction effect between time and group for each of the dependent variables. The dependent variables measured in this study were the time taken to complete the ATGUG Test as a measure of functional mobility, number of repetitions completed in the 30-Second Chair Stand Test as a measure of functional lower extremity strength, change in angular displacement as a measure of ankle proprioception, and change in the area of sway, path length, mediolateral and anteroposterior sway (eyes open, eyes closed, and balance space) as a measure of balance and postural control and adaptation. Statistical significance was determined with an alpha level of p<.05. If a statistical significance was found, a Bonferroni post-hoc analysis was performed to determine pairwise comparisons between the variables.
3. Results
3.1. Functional Mobility
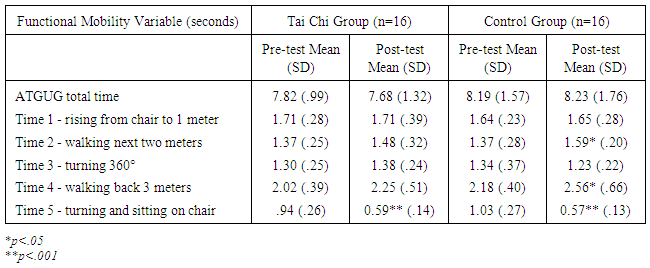
- Functional mobility was evaluated using the ATGUG Test. For all variables, a lower score represented greater mobility. Means and standard deviations for all of the functional mobility measures are presented in Table 2.
|
3.2. Functional Lower Extremity Strength
- The functional strength of the lower extremities was assessed using a 30-Second Chair Stand Test. More repetitions in this test represented better functional strength of the lower extremities. There was no significant interaction effect between time and group in relation to the number of repetitions performed during the 30-Second Chair Stand Test. However, there was a significant main effect for time, with a large effect size in relation to the number of repetitions (F(1, 30)=12.07, p<.002, ƞ2=.29). The mean number of repetitions increased in both the Tai Chi (M =13.06, SD= 2.08) and control (M =12.81, SD = 2.51) groups highlighting an improved functional lower extremity strength performance in both groups. Moreover, analysis of the main effect for group yielded no significant differences.
3.3. Ankle Proprioception
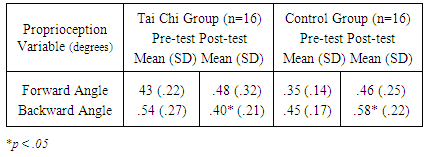
- Ankle proprioception was measured based on the angular displacement above the threshold angle detected during passive motion at the ankle. For all variables, the lower score represented better proprioception. Means and standard deviations for all of the proprioception measures are presented in Table 3.
|
3.4. Postural Control and Postural Adaptation
- In both quiet standing (eyes open and eyes closed) and the balance space tasks, decreased values represented less sway or better postural control for the quiet standing with eyes open and eyes closed conditions; whereas, increased values indicated better postural adaptation in the balance space tasks. Centre of pressure measures in the quiet standing eyes open task. There was no significant interaction effect for time and group for the anteroposterior and mediolateral sway, path length, and area of sway measures. Moreover, analysis of the main effects for each individual factor (i.e., time and group) also yielded no significant differences. This result suggested no change in the postural control mechanism when participants completed the tasks with their eyes open.Centre of pressure measures in the quiet standing eyes closed task. There was no significant interaction effect for time and group for anteroposterior and mediolateral sway, path length, and area of sway. Similarly, analysis of the main effect for each individual factor (i.e., time and group) also yielded no significant differences. This result suggested no change in the postural control mechanism when participants completed the tasks with their eyes closed.Centre of pressure measures on the balance space task. There was no significant interaction effect for time and group for anteroposterior and mediolateral sway, path length, and area of sway. Again, analysis of the main effect for each individual factor (i.e., time and group) also yielded no significant differences. This result suggested no change in the postural adaptation mechanism (i.e., the ability to approach the stability boundaries by leaning).
4. Discussion
- This study evaluated the effect of a 10-week Tai Chi training program on functional mobility and strength, ankle proprioception, and postural control and adaptation of older adults. Results from this study confirmed that a 10-week Tai Chi training program had a significant impact on ankle joint movement sense and proprioception. These findings are similar to the randomized controlled trial conducted by Liu et al. [2] on ankle joint position sense. Irrespective of the different methods used to measure proprioception, both studies highlight an approach to affect proprioception as an avenue for clinicians to monitor rehabilitation protocols and prescribe therapeutic interventions. Although many studies [32, 33, 39] have reported that the adoption of regular physical activity can attenuate the age-related decline in physiological status, few high quality studies have examined the effect of recreational exercises like Tai Chi on the ankle proprioception of older adults. Many forms of Tai Chi are executed in either single-stance weight bearing or double-stance weight bearing positions which further requires pivoting of the whole body or twisting of the trunk [36]. All forms require coordination of the body and the limbs and are highly dependent on synchronized muscle contractions that affect postural adaptation and control in coordination with rhythmic breathing [40]. A declining proprioceptive acuity in older adults due to decreasing levels of hormones such as testosterone, growth hormone, and insulin-like growth factors has been reported along with a reduced number of satellite cells in muscles [27]. Similarly, Ghez, Gordon, and Ghilardi [41] reported delayed movement onset and inaccurate trajectory formation in patients with proprioceptive loss. The findings of the present study on ankle proprioception in the control group mirror this deterioration in proprioception.In the current study, the ATGUG test was used to measure the functional mobility of the participants and lower times represented better functional mobility. A significant decrease in the time taken by the participants was observed in the Tai Chi group for two components of the test, turning and sitting back onto the chair. Jacobson, Ho-Cheng, Cashel, and Guerrero [43] reported that Tai Chi involves pivoting of the whole body and twisting of the trunk. It can be implied from the results of the present study that participants in the Tai Chi group may have improved their skills to make sharp turns and effectively switch between standing to sitting postures due to the twisting described above. However, a significant decrease in the time taken by the participants in the control group in the same task was also observed. It can be argued that the participants in the control group may have completed daily physical activities and functional tasks involving repeated sitting and standing which made them more efficient in this task as well. The 30-Second Chair Stand Test was used to measure the functional strength of the lower extremities. The findings demonstrated that the Tai Chi intervention enhanced the functional strength and endurance of the lower extremity muscles. Tai Chi exercises were performed in standing which may be a possible explanation for this improved strength. Tai Chi training demands controlled knee flexion and extension requiring concentric and eccentric contraction of the muscles around the knee joint. Most of the forms and positions are performed with the knee positioned in slight flexion which enhances eccentric control and strength of the knee extensors [42]. These effects are consistent with the findings reported by Liu et al. [2]; however, we cannot ignore the fact that the control group also improved in functional lower extremity strength with their normal daily functional activities.Increased balance space in quiet upright standing is considered to be an indicator of poor balance [38]. This has been attributed to the secondary effects of aging resulting in declined muscle strength, poor vision, delayed reflexes, and incoordination [44]. The results from this study revealed no change in either group in any of the variables on postural control and adaptation tasks.Postural control and adaptation is highly sensitive to the task specific performance. Any cognitive or physical impairment may have an effect on performance sensitivity. All participants in the current study ranged from 57-79 years, and were physically active. For the postural control and adaptation variables, the inferential statistical analysis revealed no significant differences. The level of change in postural control and adaptation from pre- to post-treatment may also be attributed to the participant’s level of fitness and overall positive health. That is, since the participants were active and generally healthy, their scores with the postural control and postural adaptation tasks may have required longer treatment (increased intensity, duration, and/or type Tai Chi exercises) to achieve significant improvements. It can also be noted that the increased scores in path length and area experienced by the Tai Chi group accompanied by the smaller standard deviations illustrate a positive trend in adaptation which is not shown in the control group. Alternatively, it can be argued that participants executed the assigned tasks within their perceived functional capabilities rather than their actual functional limits affecting the results. Some of the limitations of the current study include possible gender bias. Only one male participant volunteered for the study and this raises the question that males and females may respond differently to Tai Chi retraining. Future research with a larger sample size that was equally distributed for males and females is suggested. Also, combining this protocol with other biomechanical analysis techniques including electromyography, kinematic and kinetic analysis, and video motion capture may provide further insight into the clinical utility of the benefits of Tai Chi as a possible intervention. It is clear, that additional research is needed in order to further examine the effects of Tai Chi in older adults. In the future the development of a randomized control trial study design with different frequencies, intensities, and duration of training that are clearly reported may assist in further exploring the utility of this intervention and increase the external validity of the findings.
5. Conclusions
- The implementation of a 10-week Tai Chi training program resulted in positive effects on functional lower extremity mobility and strength and ankle proprioception but not on postural control and adaption. Although the changes in proprioception were confined to the Tai Chi group, further research is required to explore the clinical utility of this intervention and help to develop the optimal intensity, duration, frequency, and specific movements that would be most beneficial in the older population.
ACKNOWLEDGEMENTS
- The authors wish to extend their sincere appreciation to Dan Vasiliu for his skill and diligence in preparing the tilting platform which was used to measure proprioception.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML