-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2017; 7(5): 216-220
doi:10.5923/j.ajmms.20170705.02

Prognostication of Left Ventricle Deadaptive Remodeling at Myocardial Infarction with ST Segment Elevation
S. R. Kenjaev, A. L. Alyavy, M. L. Kenjaev, R. A. Rakhimova, A. K. Koyirov, U. Sh. Ganiev
Republican Research Center of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Early detection of deadaptive nature of heart remodeling and adequate pharmacological correction can prevent a development of unfavorablelong-term effect of acute myocardial infarctionconditioning survivability of patients. One of the main criteria of postinfarction remodeling is a presence of viable myocardium in the area of ischemic lesion promoting a preservation of left ventricle normal sizes and contractility.302 patients with ST elevation acute myocardial infarction at the age from 21 to 70 years (mean age 56±4,3 years) were included to the research. Patients were performed stress-echocardiography with dobutamine on the 3rd- 6th day after the disease and recurrent echocardiography after 3 months. ROC analysis with estimation of sensitivity and specificity was performed for receiving operational characteristics of predictors of event attachment. In patients with ST segment elevation acute myocardial infarction regardless of myocardium reperfusion type, the development of left ventricle deadaptive remodeling can be prognosed with the use important predictors as initial WMAI >1.57 (with sensitivity 70% and specificity 82%), WMAI at the low dose of dobutamine stress-echocardiography >1,25 (with sensitivity 73% and specificity 82%); ejection fraction of left ventricle at the low doses of dobutamine stress-echocardiography < 42% (with sensitivity 70% and specificity 86%).
Keywords: Acute myocardial infarction, Prognosing of deadaptive remodeling, Stress-echocardiography with low doses of dobutamine
Cite this paper: S. R. Kenjaev, A. L. Alyavy, M. L. Kenjaev, R. A. Rakhimova, A. K. Koyirov, U. Sh. Ganiev, Prognostication of Left Ventricle Deadaptive Remodeling at Myocardial Infarction with ST Segment Elevation, American Journal of Medicine and Medical Sciences, Vol. 7 No. 5, 2017, pp. 216-220. doi: 10.5923/j.ajmms.20170705.02.
Article Outline
1. Background
- One of the main reasons of population’s mortality both in Uzbekistan and all over the world is coronary heart disease (CHD) and its such dangerous form as myocardial infarction. There are effective treatment types of acute myocardial infarction with ST segment elevation in modern medicine: systemic thrombolysis with constantly modified new drugs and interventional treatment methods including coronary angioplasty. In spite of that, in 22% of men and in 46% of women large-focal myocardial infarction is complicated by the development of chronic cardiac failure during the nearest 5 years of observation [13]. That is why measures directed on the fight with processes of the left ventricular postinfarction remodeling are very important [5]. After restoration of blood flow in IRA area, the changes of contractility indices, myocardium geometry and central hemodynamics occur and they determine the further clinical course and treatment tactics. Subject to the development and wide use of modern methods of blood flow restoration at STEMI, a serious attention is paid to the issue of prevention of LV early pathologic remodeling development. It allows to effect on the prognosis of the disease and patients survivability [3, 4]. LV remodeling processes after STEMI evaluate an appearance of recurrent myocardial infarctions, embolic strokes, sudden death. That is why early detection of deadaptive nature of heart remodeling and adequate pharmacological correction can prevent the development of unfavorable long-term outcomes of AMI defining patients survivability [1, 2, 8, 10, 18]. One of the important criteria of postinfarction remodeling is a presence of viable myocardium in the area of ischemic lesion promoting the preservation of LV normal sizes and contractility [1-3, 14-16, 18]. Detection of viable myocardium in patients with AMI allows to predict the development of unfavorable LV remodeling [8, 11, 12, 17, 20]. Hereby, prevention of cardiac rate fatal abnormalities development, sudden death, cardiac failure must be directed on the study of pathogenic mechanisms of deadaptive remodeling (DR) development in patients with AMI of various localization after vascularization by percutaneous coronary interventions (PCI) methods and systemic thrombolysis. All above mentioned procedures allow to work-out measures directed on the fight with LV postinfarction remodeling processes by development of early diagnostics and treatment of myocardial stunning in the conditions of emergency medicine. The evidence of progressing of LV remodeling processes also depends on the presence of viable myocardium which is defined as “myocardial obnubilation” («stunning») which arises at acute coronary occlusion with further reperfusion of myocardium [6, 7, 10, 11, 14]. By L. Bolognese et al. data, after PCI, unfavorable LV remodeling was registered in 30% of patients with ACS with ST elevation [8]. This index approximated to 34% in patients after systemic thrombolysis. Frequency of cardiac remodeling in persons with the presence of viable myocardium in the area of ischemic lesion at anterior and posterior localization of AMI was approximately equal. At the same time, an absence of a viable myocardium defines a part of patients with AMI who are disposed to favorable outcomes of the remodeling: as it has been shown in L. Bolognese and G. Cerisano investigation, there were registered higher volumetrical indices of intracardiac hemodynamics in patients without viable myocardium after 6 months [8]. On the background of intravenous dosing of dobutamine which was used with the aim of indirect detection of viable myocardium, changes of local contractility failure index in infarction area and peak values of CPK were significantly correlated with the rate of EDV index’s decrease: -r=-0.66; Р<0.000001; r=0.51; Р<.00001, respectively.
2. Objective
- To study the condition of myocardial stunning and its value in the process of LV postifarction remodeling, prognosing of deadaptive remodeling of patients at acute myocardial infarction with ST elevation.
3. Material and Methods
- 302 patients with STEMI at the age from 21 to 70 years (mean age 56±4.3 years) having been admitted to the department of cardio-therapeutic ICU of the Republican Research Centre of Emergency Medicine were included to the investigation. STEMI diagnosis was determined on the base of clinical presentation and electrocardiographic criteria. Inclusions criteria: typical clinical presentation of STEMI and one of the criteria stated below: 1) ST elevation more than 2 mm in two adjacent pectoral leads or ST elevation more than 1 mm in the standard leads; 2) acute left bundle branch block (LBBB). Exclusions criteria: patients elder than 70 years; prescription of pain syndrome more than 24 hours; myocardial infarction in anamnesis; severe concomitant somatic diseases (cerebral blood flow acute abnormalities, oncologic, mental and surgical diseases) which influence on informativity of investigation; objective contraindication to the performing of stress-echocardiography; patients with problematic echo-visualization; patient’s refuse from stress-echocardiography. Thrombolytic therapy (TLT) was used as reperfusion therapy, at the presence of contraindications to TLT we had used primary PCI and stenting of coronary artery. Primary PCI was performed in 104 (35%) patients with AMI and STEMI. Saving PCI after unsuccessful thrombolysis during 12 hours was conducted in 13 (4.5%) cases, postponed PCI after thrombolysis during 48-72 hours – in 172 (58%) patients. Peculiarities of clinical presentation, dynamics of electrocardiographic changes, parameters of central hemodynamics were studied in the process of investigation. All patients after stabilization of their condition on the 3rd-6th days of the disease were performed stress-echocardiography with dobutamine. Echocardiography. Echocardiography was conducted by “Clear Vue 650” (Philips) ultrasonograph and “Sonoline Omnia” (Siemens) with the use of 2-4 MHz MF sensor. Investigation was carried out in the patient’s position on the left side with insignificantly raised upper half of the body. Standard projections were used at visualization – parasternally on long and short axes, on the short axis at 3 levels – at the level of mitral valve, at the level of papillary muscles and at the apical level; apically – in the projection of two- and four-chamber image in M and 2D modes. Pulsed-wave, continuous-wave and colored Doppler cardiography were also used. Stress-echocardiography with dobutamine was carried out for detecting reversible dysfunctioning myocardium (stunning myocardium) after condition’s stabilization on the 5th-8th days of the disease. Received data were handled on Pentium-IV PC with the help of Microsoft Office Excel-2012 including the use of built-in functions of statistic handling. Methods of variation parametric and nonparametric statistics with calculation of arithmetical mean index (M), mean quadratic deviation (σ), standard mean error (m), relative number (frequency, %), statistical significance of received measuring at the comparison of mean quantity was detected according to Student’s criterion (t) with calculation of error probability (Р) at the check of distribution of normality (by excess criterion) and equality of general dispersions (F – Fisher’s criterion) were used. For estimation of statistic significance of calculated criteria we used indices and tables of critical values for acceptable levels of significance (P). Four levels of significance were registered as statistically significant changes: high– P<0.001, mean – P<0.010, low (maximum) – P<0.050, insignificant – P>0.050. ROC analysis with definition of sensitivity and specificity was carried out for receiving operational characteristics of event predictors. Working-out of the received data and their graphic presentation were carried out by Pentiun-4 with the use of standard («MS Excel-7», «Statistica 6.0») and special software. Correlated analysis was conducted with the use of Spearman’s (Rs) and Pearson’s (r) analysis.
4. Results
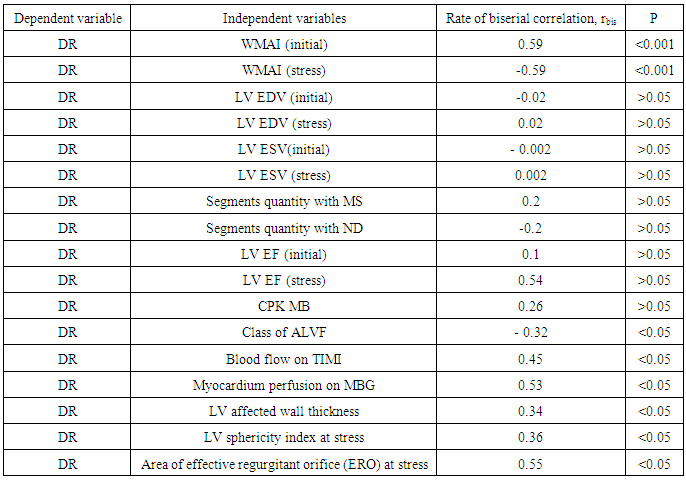
- For preliminary estimation of echocardiography indices on LV deadaptive remodeling development it was carried out the estimation of biserial correlation rates (Table 1).
|
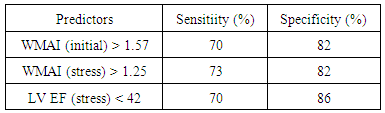
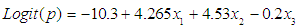 where x1 – WMAI (stress), x2 – WMAI -1, х3 - LV EF (stress).Every index of echocardiography included into equation of logistic regression was an independent criterion of DR development and it allowed to use it as a separate prognostic sign. For estimation of statistic significance of the received regression equation it was used the Hosmer-Lemeshow criteria, the value of which made up Р=0.85 and it testified good indices of the received model. Sensitivity and specificity in the prognosis of unfavorable remodeling development, WMAI (stress) value >1.25 made up 73.1% and 8.8% respectively. (AUC 0.82; Р<0.0001) (Fig. 1).
where x1 – WMAI (stress), x2 – WMAI -1, х3 - LV EF (stress).Every index of echocardiography included into equation of logistic regression was an independent criterion of DR development and it allowed to use it as a separate prognostic sign. For estimation of statistic significance of the received regression equation it was used the Hosmer-Lemeshow criteria, the value of which made up Р=0.85 and it testified good indices of the received model. Sensitivity and specificity in the prognosis of unfavorable remodeling development, WMAI (stress) value >1.25 made up 73.1% and 8.8% respectively. (AUC 0.82; Р<0.0001) (Fig. 1).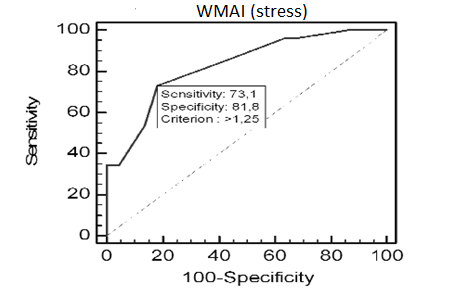 | Figure 1. Sensitivity and specificity of IRA stress-echocardiography with dobutamine low doses in the prognosis of LV deadaptive remodeling in patients with STEMI |
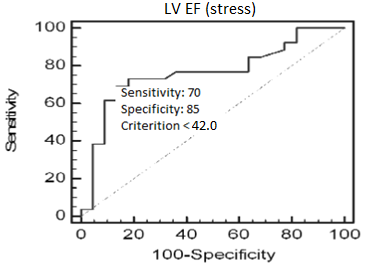 | Figure 2. Sensitivity and specificity of LV EF (stress) in the prognosis of LV deadaptive remodeling development in patients with AMI and STEMI |
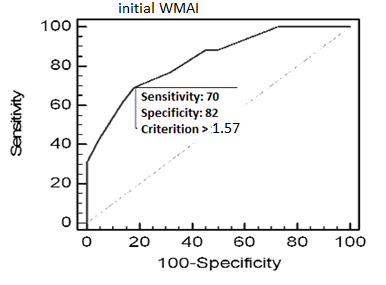 | Figure 3. Sensitivity and specificity of initial WMAI in the prognosis of LV deadaptive remodeling development in patients with AMI and STEMI |
|
5. Discussion
- Prognosing of deadaptive remodeling (DR) is an important task at acute period of transmural myocardial infarction. But there are still no concreat data which indices are exactly important for LV DR after myocardial infarction. Independent predictors of LV dilatation in patients with ACS after reperfusion are: the presence of viable myocardium, the size of local abnormalities of contractility during dobutamine infusion and a quantity of pathologic Q waves. The absence of EDV rising at the presence of viable myocardium in the area of ischemic lesion was kept during 3 months of observation (Р<0.006) [18].Rehabilitation of subepicardial fibers in the parts of transmural lesion promotes the recovery of the function, prevents dilatation and changes of LV forms at later periods. Improvement of contractile function is registered at the absence of systolic thickening of myocardium via subepicardial fibers movement inside [1]. Apparently, perefusion at early period of AMI limits the necrosis area promoting the preservation of myocardial fibers in border-line and subepicardial areas. Due to ROC analysis, WMAI (stress) received in the result of stress-echocardiography with dobutamine low doses on the 5th-8th days of disease at elimination threshold of 1.25 with 73% sensitivity and 82% specifictity in our investigation allows to prognose LV deadaptive remodeling after 3 months of observation (Р<0.001). Initial WMAI > 1.57 testifies a high risk of LV DR development (70% sensitivity and 82% specificity) (P<0.0001). One of the important predictors of deadaptive remodeling after myocardial infarction is LV EF. LV EF value less than 42% with 70% sensitivity and 86% specifictity allows to prosnose the development of LV deadaptive remodeling after 3 months of observation (Р<0.001).
6. Conclusions
- Thereby, it is possible to prognose LV deadaptive remodeling in patients with STEMI independently from myocardium reperfusion type (PCI or thrombolysis) with the use of important predictors such as initial WMAI >1.57 (70% sensitivity and 82% specificity), WMAI at low doses dobutamine stress-echocardiography >1.25 (with 73% sensitivity and 82% specificity) and LV EF < 42% at low dose dobutamine stress-echocardiography with 70% sensitivity and 86% specificity).
ABBREVIATIONS
- CHD - coronary heart diseaseAMI - (acute myocardial infarction) and STEMI – ST elevation MI LV - left ventricle IRA - infarct-related artery DR - deadaptive remodeling PCI - percutaneous coronary interventions CPK - creatine phosphokinaseMI - myocardial infarctionEDV - end diastolic volumeERO - effective regurgitant orifice ALVF - acute left ventricular failure ACS - acute coronary syndrome TLT - thrombolytic therapy LVEF - left ventricle ejection fraction WMAI (initial) - initial wall motion abnormality index in rest WMAI (stress) - wall motion abnormality index at low doses of dobutamine LVEDVI - left ventricular end diastolic volume index LVESVI - left ventricular end systolic volume index МS - myocardial stunning ND - nonreversible dysfunction TIMI - Thrombolysis in myocardial infarction MBG - Myocardial Blush Grade
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML