-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2017; 7(4): 186-188
doi:10.5923/j.ajmms.20170704.05

A 36-year-old Woman with Spastic Quadriparesis: A Case Report and Review of Literature
Mehdi Moghaddasi1, Mona Nabovvati2, Saeed Razmeh2
1Assistant Professor of Neurology, Neurology department, Rasoul Akram Hospital, Iran University of Medical Science, Iran
2Neurology Assistant, Neurology Department, Rasoul Akram Hospital, Iran University of Medical Sciences, Iran
Correspondence to: Saeed Razmeh, Neurology Assistant, Neurology Department, Rasoul Akram Hospital, Iran University of Medical Sciences, Iran.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Neuromyelitis Optica (NMO) is a necrotizing autoimmune disease that affects the spinal cord and optic nerve. It can be associated with systemic autoimmune disorders such as systemic lupus erythematosus (SLE), thyroid diseases, myasthenia gravis and Sjögren’s syndrome. The incidence NMO is very rare in lupus and only have been reported as a case report. In this paper, we present a case of SLE who developed NMO in the course of the disease and we discuss that it is essential in any SLE patient with myelitis, Devic syndrome should be considered.
Keywords: Neuromyelitis Optica, Systemic lupus erythematous, Myelitis
Cite this paper: Mehdi Moghaddasi, Mona Nabovvati, Saeed Razmeh, A 36-year-old Woman with Spastic Quadriparesis: A Case Report and Review of Literature, American Journal of Medicine and Medical Sciences, Vol. 7 No. 4, 2017, pp. 186-188. doi: 10.5923/j.ajmms.20170704.05.
1. Introduction
- Systemic lupus erythematous (SLE) is a chronic autoimmune disease that can affect any organ [1]. Its clinical manifestations and course are highly variable. Central nervous system (CNS) complications of SLE is different including seizures, cerebrovascular disease, myelopathy, mood disorders, cognitive impairment and aseptic meningitis [2]. Neuromyelitis Optica (NMO) is a necrotizing autoimmune disease that affects the spinal cord and optic nerve. The disease can be idiopathic or associated with other inflammatory autoimmune diseases [3]. Myelitis is a rare complication of lupus that involves 2% of patients. It can occur as the first manifestation or in the course of a disease [4]. Spinal cord involvement is characteristic in NMO. Its lesion is necrotizing and longitudinal extending over three or more vertebral segments [5]. For this reason, the incidence of this myelitis and devic is very rare in lupus and only have been reported as a case report. We report a case of SLE that developed NMO in the course of the disease.
2. Case Report
- We report a case of a 36-year-old woman with a history of SLE. The patient’s lupus was diagnosed 8 years ago when she presented with morning Stiffness and pain in joints of hands and since then, her disease was in remission with prednisone doses ranging from 5 mg to 20 mg once a day and hydroxychloroquine 200 mg daily. The patient presented to our hospital with 2 weeks history of lower limbs weakness and gait disturbance that progress to upper limbs during 1 day. She also reported paresthesia of the lower extremity over 1 month. Her family history, social history, and review of systems were negative. On examination, she was conscious and had stable vital signs, there was no peripheral lymphadenopathy palpable. He had normal rate and regular rhythm, no murmur. The abdomen was flat, soft and non-tender with normal liver and spleen. Muscle strength in proximal and distal upper limbs were 4/5 and in lower limbs were 3/5. Sensory examination shows sensory level in T5 with abnormal position and vibratory in lower limbs. Deep tendon reflexes were 3+ in upper limbs and 4+ in Achilles and knee and the plantar response was bilateral extensor. Brain MRI showed no abnormality. MRI of spine showed longitudinal hypersignality lesion in whole cervical and upper thoracic. Cerebrospinal fluid (CSF) was normal for cell count, protein and glucose. Oligoclonal bands (OCB) was negative. NMO Ab was positive. Plasma exchange was started with total dose 250 cc/kg that marked improvement observed in the period of hospitalization and 1 month later in follow-up visit.
3. Discussion
- NMO, also known as Devic’s disease, is a rare autoimmune disorder characterized by involvement of optic nerve and spinal cord. The pathogenesis of NMO is different from MS [6]. in this disease the humeral immune system has important role, NMO-IgG (anti-AQP4) plays a direct role in the pathogenesis of NMO.it is against of Aquaporin-4 (AQP4), a water channel protein that is highly concentrated in brain and spinal cord, in addition, NMO mainly causes necrosis of white matter and gray matter of the brain and the spinal cord and usually with absence of OCB in cerebrospinal fluid (CSF) [7, 8]. It can be associated with systemic autoimmune disorders such as systemic lupus erythematosus, thyroid diseases, myasthenia gravis and Sjögren’s syndrome [9]. SLE has variable effects on the central nervous system (CNS).Neuropsychiatric complications of SLE is different including stroke and transient ischemic attacks, seizures, aseptic meningitis, myelopathy, polyneuropathy, organic psychosis, mood disorders, cognitive impairment and movement disorder such as chorea [10]. The Manifestations of myelitis or optic neuritis in SLE are very unusual that only 1−2% of patients with SLE exhibit myelitis or optic neuritis and only half of the patients affected by myelitis have criteria for the NMO spectrum of disorders [11]. Deodhar et al. reported the first case of SLE with longitudinal myelitis in 1999. He described a 21-year-old woman with SLE that developed extensive involvement of the spinal cord with good response to cyclophosphamide and high dose corticosteroids [12]. The optic neuritis in SLE is usually bilateral with poor prognosis compared to multiple sclerosis [13]. Treatment in this disease consisted of plasma exchange and IV methylprednisolone for acute attacks and azathioprine, rituximab, mycophenolate mofetil, methotrexate, or mitoxantrone for maintenance therapy [14]. In a study Mok CC and colleague showed use of cyclophosphamide was successful in halting relapses in a patient with systemic lupus erythematosus-associated NMO who was unresponsive to high-dose oral and intravenous corticosteroids, intravenous immunoglobulin, mycophenolate mofetil, tacrolimus, low-dose daily oral cyclophosphamide and rituximab [15]. In conclusion it is necessary, in any patient with SLE that present with myelitis, Devic syndrome should be considered because prompt diagnosis and treatment prevents disability and mortality.
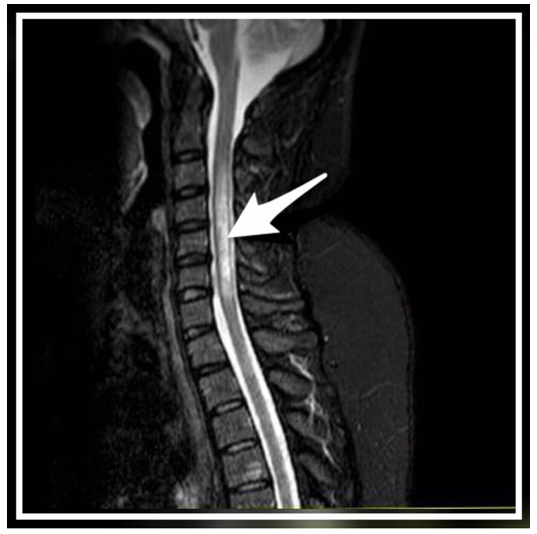 | Figure 1. Sagittal STIR MRI reveals the large longitudinal lesion in cervical and upper thoracic spinal cord |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML