-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2017; 7(4): 174-178
doi:10.5923/j.ajmms.20170704.03

The Issues of Acute Respiratory Distress Syndrome at Combined Skeletal Injury Complicated by Fat Embolism
F. Kh. Mirdjalilov, A. I. Ikramov, M. M. Nizamova, R. N. Khakimov
Republican Research Centre of Emergency Medicine, Tashkent Institute of Post-Education Doctors, Tashkent, Uzbekistan
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

15-20% of all victims with combined injury die from severe complications of a traumatic disease. One of these complications is fat embolism syndrome. One of the basic mechanisms of fat embolism development is a systemic disorder of fat metabolism which leads to the filling of the organs and tissues microcirculation by the neutral fat drops. Microcirculation disorders and cell membranes injury at the fat embolism lead to a massive brain edema, to the development of respiratory distress syndrome of adults, to heart and renal failures, to a toxic disintegration of erythrocytes and hypoplastic anemia. The authors carried out a retrospective analysis of extended clinical, computer-tomography and X-ray investigations of 21 patients with combined skeletal injury admitted to the department of traumatology of the Republican Research Centre of Emergency Medicine in 2016 and revealed X-ray, computer-tomography signs of the acute respiratory distress syndrome caused by post-truamatic fat embolism.
Keywords: Fat embolism syndrome, X-ray semiotics, Acute respiratory distress syndrome
Cite this paper: F. Kh. Mirdjalilov, A. I. Ikramov, M. M. Nizamova, R. N. Khakimov, The Issues of Acute Respiratory Distress Syndrome at Combined Skeletal Injury Complicated by Fat Embolism, American Journal of Medicine and Medical Sciences, Vol. 7 No. 4, 2017, pp. 174-178. doi: 10.5923/j.ajmms.20170704.03.
Article Outline
1. Introduction
- Combined injury remains an object of intent attention for a wide circle of the researchers and practitioners. Combined injury is a simultaneous injury of two or more anatomic areas conditioned by the impact of one traumatic agent. Technological progress, development of industry, construction and transport stipulated a stable tendency of traumatism’s growth. Injury as a death cause is a leading one in the age group from 20 to 60 years increasing a mortality due to cardio-vascular and oncologic diseases in two times [1, 9]. According to some prognosis, injury can take the first place in morbidity and lethality of the population [5, 9]. Victims with multiple and combined injuries make up 17.5-28% of the all traumatologic inpatients and orthopedic traumas make up 49.8-83.5%. In the structure of locomotorium combined injuries extremities traumas predominate (52.5-86.6%) and the most typical ones among them are the fractures of long cortical bones. 15-20% of all victims with combined injuries die from severe complications of the traumatic disease [5, 9]. Fat embolism syndrome (FES) is one of such complications. The severe mechanic injuries of the locomotorium with long cortical bones fractures often lead to the development of FES [3, 9]. But, the fat embolism (FE) occurs more often than it is diagnosed and not only at severe skeletal injury, but also at anaphylactic and cardiogenic shock, pancreatitis, apparent death with successful resuscitation – at any critical condition. It is important to distinguish a phenomenon of fat embolism, which is a morphologic finding (a detection of fat drops 6 micrometer by size in biologic fluids) from fat embolism syndrome with clinical manifestations [2, 3]. There is a significant prevalence of FE morphologic findings over clinical manifestations The frequency of FE development varies, by different authors data, from 0.5 to 30% at injuries with multiples fractures of long cortical bones and pelvic bones fractures. According to ICD 10 FE is classified as T79. 1: fat embolism (traumatic) [10-12]. The resent researches give the data about 3–13% of the lethal outcomes at FES. The lethality reached 47–67% in the past [5, 8]. A big difference in the data can be explained both by the enhancement of prevention methods, intensive therapy and more frequent detection of the light and obliterated forms of FES. The modern views on the biochemical changes suppose that free fatty acids are hydrolyzed from the neutral fats. They provoke endothelium injuries and are directly toxic for pneumocytes. The sources of free fatty acids are: lysed triglycerides from fracture’s place and a deposited fat undergone to the lipolysis under catecholamines. A disturbance of vessels integrity, haemorrhages, adhesion of platelets and thrombus formation are regarded as the main factors of tissues injury and organ dysfunction [7, 8]. One of the leading mechanisms of fat embolism development is a sharp systemic disorder of lipid exchange, which then leads to filling of microcirculation channel of tissue and organs with drops of neutral fat 6-8 micrometer in size with the following micro-thrombus formation up to disseminated intravascular coagulation (DIC), endotoxication by ferments and lipid metabolism’s products (endoperoxides, ketones, leukotrienes, prostaglandin, thromboxane), by the cell membranes systemic injuries in the microcirculation channel (a systemic capillaropathy), first of all at the lungs which block up to 80% of fat drops [3, 4, 12-14]. Microcirculation disorders and cell membranes injury at fat embolism lead to a massive brain edema, to the development of respiratory distress syndrome of adults (RDSA), to heart and renal failures, to a toxic disintegration of erythrocytes and hypoplastic anemia. [4, 5, 12, 15, 16]. Thereby, a complexity and relevance of fat embolism issue is evident and a lethality rate of this complication remains high. The concordance of opinions on the pathogenesis, prevention and treatment of FE is still absent. A special complexity is in the early diagnostics of FE subject to the absence of clear clinical presentation and pathognomic symptoms, laboratoty diagnostics is little specific [10].
2. Object
- To reveal X-ray and computer-tomography (CT) signs of the acute respiratory distress syndrome caused by a post-truamatic fat embolism.
3. Materials and Methods
- A retrospective analysis of extended clinical, computer-tomography and X-ray investigations of 21 patients with combined skeletal injury admitted to the department of traumatology of the Republican Research Centre of Emergency Medicine (RRCEM). There were 14 men and 7 women, mean age made up 47,3±18,4 years.All patients were admitted to the department of combined injury with multiple fractures of cortical bones of upper and lower extremities, it led to the development of pulmonary fat embolism. Radiography of chest organs was carried out by the Polymobil Plus analogous portable X-ray machine with the following digitization of image on CR 30-X 2nd. MSCT was done by Somatom Perspective - 64 (Siemens), at 130kV of the tube voltage, current of 80mAs, 2.0 mm of Slice collimation, 0.6 sec of Rotation Time, Pitch 0.95, 0.5mm of Increment Reconstruction, B80S of Kernel and about 300 mm of FOV. Radiologic investigations were compared with clinical presentation at different periods of disease.
4. Results
- All patients admitted with a combined injury, with predominant damage of the long cortical bones complicated by pulmonary fat embolism. At the admission general condition of 20 patients was severe, respiration was superficial up to 60 per minute, oxygen saturation in blood reached up to 52%. Diminished breath sounds were at auscultation with the presence of singular small bubbling rales, mainly in the inferior lobe. All patients were taken to the surgical ICU where they were performed anti-shock therapy: intubation of ALV, infusive therapy, narcotic pain relief, antibacterial therapy, prevention of DIC-syndrome, pulmonary and fat embolisms. Parallel to the development of clinical presentation, all patients were undergone X-ray investigation and computer tomography. In 80% of patients during the first day from the injury time there were defined symmetric polymorphous nidal shadow along all areas and zones, more in middle-lateral ones (fig. 1a). In the rest of patients (20%) radiologic presentation at admission was negative. In the dynamics on the 2nd -3rd days there were detected free fatty globules in all patients’ analysis of urine and blood, and typical petechial skin rash on the cheek, neck, chest, axillary area and on the conjunctiva. At the X-ray investigation in 78% of patients there was detected a positive X-ray dynamics, an improvement of pulmonary tissue pneumatization from the both sides (fig.1b). At the same time during computer tomography we detected diffuse induration of pulmonary tissue by a “mat glass” type, mainly in the dependent zones and increase of radiologic density of pulmonary parenchyma from the right up to 590±35HU, from the left up to 650±25HU. “Mat glass” is a term used for feature of the processes conducting by reduction of pulmonary tissue density (a sign of interstitial type of infiltration). “Mat glass” is an area of moderately reduced aerial pulmonary tissue, the key-sign of which is a visibility of pulmonary vessels and bronchus walls. The cause of “mat glass” phenomenon appearance is a thickening of alveolar septum and partial filling of alveolus with secretion [2]. On the background of the “mat glass” there were defined irregular areas of consolidation, mainly in dependent, posterior segments of the lungs; radiologic density of the pulmonary tissue there reached up to 125±35HU (fig. 1c).
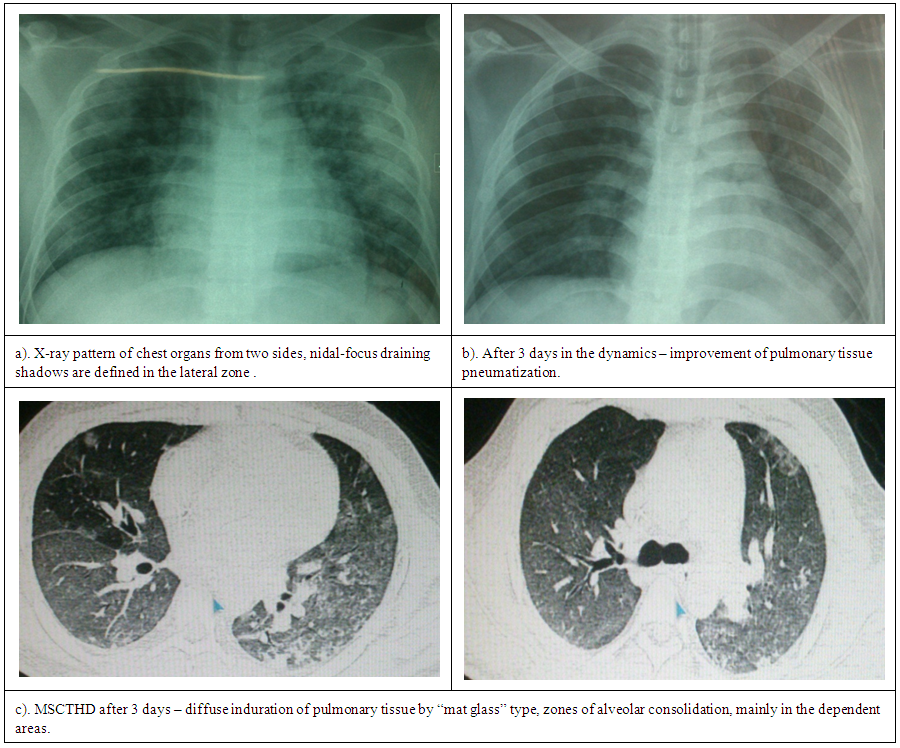 | Figure 1. X-ray pattern and MSCT of chest organs in patients with combined injury, complicated by fat embolism |
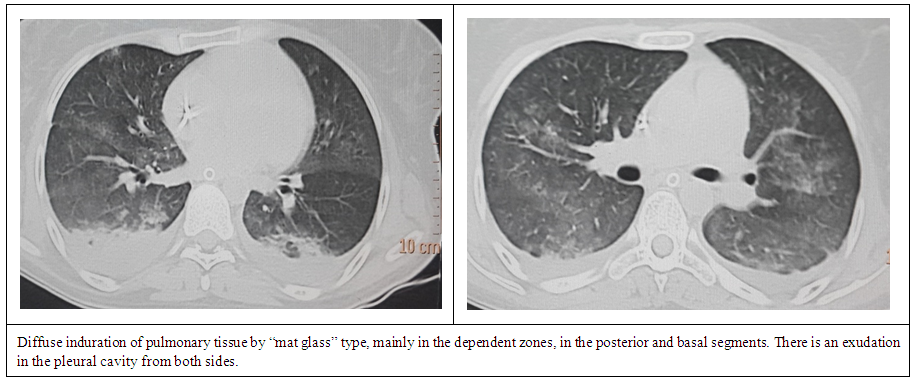 | Figure 2. MSCTHD of chest organs in patient with combined injury complicated by fat embolism, the 4th day |
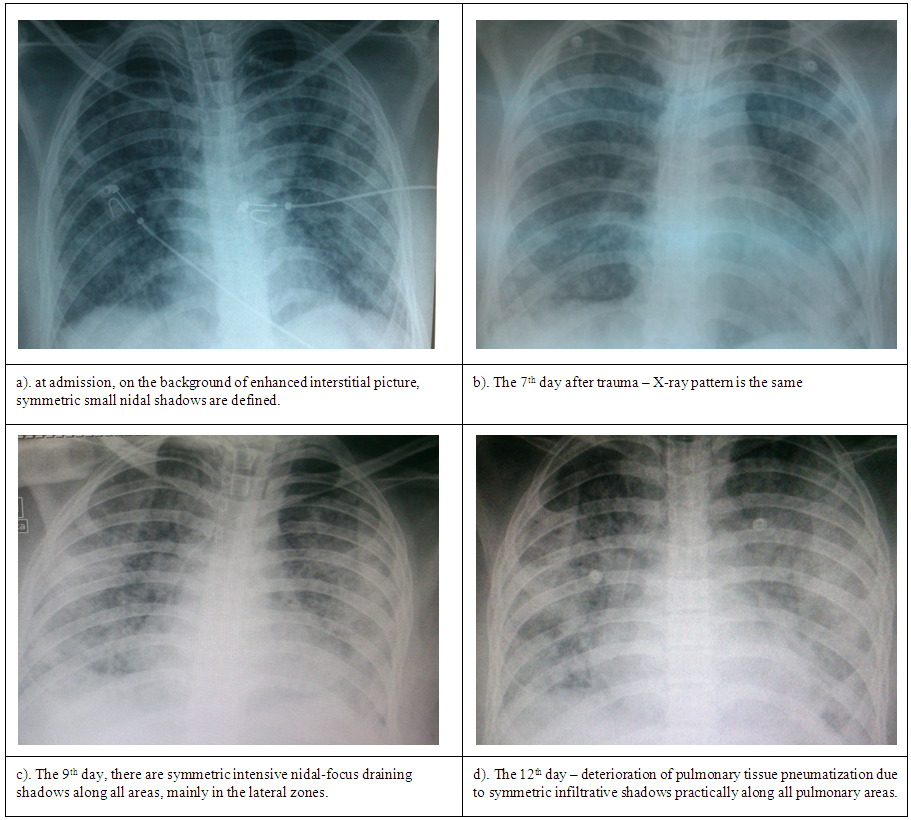 | Figure 3. X-ray pattern of the patient with combined injury complicated with a mixed form of fat embolism and severe rate of traumatic shock |
5. Discussions
- The issue of fat embolism syndrome remains actual. Concurrence in the views on pathogenesis, diagnostics, treatment and prevention of fat embolism is absent till now. The early diagnostics of fat embolism has a special difficulty subject to the absence of clear clinical presentation and pathognomonic symptoms, laboratory diagnostics is little specific. In our investigation in all patients with post-traumatic respiratory distress-syndrome we revealed two phases of pulmonary edema – interstitial and alveolar. In other words, early diagnostics is based on the detection of interstitial edema in patients, but it is complicated at performing X-ray investigation. MSCT allows to objectively estimate structural changes of pulmonary parenchyma – it is very important for early diagnostics and for the choice of treatment tactics.
6. Conclusions
- 1. Correlation of received X-ray and CT data with clinical presentation dynamics which was depended on the disease severity and development rate of fat embolism syndrome in the organism has been detected.2. X-ray pattern in 90% patients with a combined skeletal injury was characterized by the fleetingness of the process: on the 1st day after trauma X-ray pattern of chest organs in 95% of patients defined nidal draining shadows, mainly in the lateral zones and it corresponded to the phase of alveolar pulmonary edema. The reverse X-ray dynamics of the process was the same: on the 3rd day after injury there was an improvement of the pulmonary tissue pneumatization, the enchancement of the lung pattern by the interstitial type. In patient with a severe rate of the traumatic shock (rate III) X-ray pattern was characterized by longer and evident phase of alveolar edema on the peak of which she died. 3. MSCTHD allowed to estimate a condition of the lung parenchyma and other chest organs more objectively. At performing computer tomography, the CT pattern in 95% of patients on the 3rd -6th days of the process, in spite of a positive X-ray pattern, in all patients we registered induration of pulmonary tissue by the “mat glass” type with the presence of consolidation areas; there was an exudation to the pleural cavity in 30% of patients with a density up to +23HU, heart borders were not changed, ejection fraction was normal. Also, with the use of CT data, an anteroposterior gradient was revealed (more dense pulmonary tissue was in the dependent zones – in the posterior and basal segments of the lungs).
Abbreviations
- ARDS – acute respiratory distress syndromeMSCTHD – multi-spiral computer tomography of high definition FE – fat embolism FES – fat embolism syndrome РаО2 – oxygen tension in the arterial blood SO2 – oxygen saturation of blood PPEE – positive pressure at the end of expiration DIC – disseminated intravascular clotting TA – traffic accidentALV – artificial lung ventilation
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML