-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2017; 7(3): 97-102
doi:10.5923/j.ajmms.20170703.02

Tactics of Surgial Treatment of Patients with Multifocal Atherosclerosis
Sh. I. Karimov, A. A. Irnazarov, U. A. Asrarov, H. K. Alidzhanov, J. P. Matmuradov
Department of Faculty and Hospital Surgery, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Sh. I. Karimov, Department of Faculty and Hospital Surgery, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: improve the results of treatment of patients with chronic lower limb ischemia in multifocal atherosclerosis by selecting the appropriate surgical approach with using both open and interventional therapies. Material and Methods: The study is based on the results of surgical treatment of 115 patients with atherosclerosis several arterial pools who have received treatment in the Vascular Surgery Department of the Second Clinic of Tashkent Medical Academy for the period from 2014 to 2016. The age of patients was 48 to 82 years (63,3 ± 5,2). The criterion for selection of patients was the presence of lesions of the terminal aorta and lower limb arteries in conjunction with hemodynamically significant lesions of other arterial pools, i.e. chronic ischemia of the lower limbs in advanced atherosclerosis. Results: 38 patients with chronic lower limb ischemia II B degree in combination with hemodynamically significant carotid stenosis for primary prevention of ischemic stroke was carried out and the subsequent stage of the 22 (57.8%) patients were produced revascularization of lower limb arteries. In 19 (24%) patients with carotid stenosis with critical lower limb ischemia was achieved regression of clinical manifestations of lower limb ischemia using drug therapy, 12 (63.1%) patients carried out the installation of the catheter for prolonged intra-arterial catheter therapy, and then the carotid endarterectomy. In 19 (16.5%) patients with lesions of the carotid arteries and critical lower limb ischemia in the first stage performed endovascular interventions for critical limb ischemia. In 6 (5.2%) patients with lesions of the coronary arteries and the arteries of the lower extremities in the first stage performed stenting of the coronary arteries, in the second stage - the reconstruction of the lower extremity arteries. In 2 (1.7%) patients underwent open surgery on the arteries of the lower extremities due to hemodynamically insignificant lesions of the coronary arteries in coronary angiography. In 3 (2.6%) patients carried out palliative intervention (thoracoscopic sympathectomy) after coronary artery stenting. Only in one patient developed acute myocardial infarction.
Keywords: Multifocal Atherosclerosis, Chronic Lower Limb Ischemia, Critic Lower Limb Ischemia, Stenosis of Carotid, Treatment, Hybrid Unterventions
Cite this paper: Sh. I. Karimov, A. A. Irnazarov, U. A. Asrarov, H. K. Alidzhanov, J. P. Matmuradov, Tactics of Surgial Treatment of Patients with Multifocal Atherosclerosis, American Journal of Medicine and Medical Sciences, Vol. 7 No. 3, 2017, pp. 97-102. doi: 10.5923/j.ajmms.20170703.02.
Article Outline
1. Introduction
- The prevalence of multifocal atherosclerosis is up to 95%, and selective lesion of one vascular pool is the exception rather than the rule. [1] In this case, a combination of atherosclerotic lesions of brachiocephalic arteries, the terminal aorta and lower limb arteries accounts for about 60% of all multifocal vascular lesions [2-4]. Patients with occlusive lesions of the terminal part of aorta and the arteries of the lower limb ischemic heart disease occurs from 10.4 to 90%. Approximately one third of patients with two-pool lesions clinically detectable change in one or another third vascular pool [5-7].Defeats of arterial pools leads to dire consequences. Thus, from 40 to 60% of patients, only 10% are disabled, persistent residual changes observed in 30% of patients, and working capacity is restored after an ischemic stroke patients [8-10]. Complications of coronary heart disease are the basis of 50-70% of deaths after the reconstruction of aortic arch arteries, exceeding the number of strokes 3-5 times. It is known that the defeat of the terminal aorta in 30-52% of patients leads to the develop of gangrene followed by amputation of her [11-13].It should be noted that multiple surgical aggression increases when combined lesions. The reconstruction of a vascular pools can lead to serious complications of other vascular ones. Rothwell P.M. et al. notes the development of complications of the heart up to 22% of cases during reconstructive operations on extracranial arteries in patients with coronary heart disease, and in patients with asymptomatic ischemic heart disease - in 6% of cases. In the same study emphasizes the role of latent coronary insufficiency in the development of coronary complications after surgery on extracranial arteries [13].According to the International Register REACH (2006), approximately 50% of patients with coronary heart disease, cerebral ischemia and atherosclerotic lesions of lower limb arteries have symptoms of atherothrombosis in more than one vascular pool, and approximately 4% of the patients revealed symptoms in all 3 pools. And if you take into account the asymptomatic lesions that can be detected only by means of additional methods of research, the proportion of multifocal lesions reach high numbers [4, 7, 14].Therefore, detection of atherosclerotic lesions of a vascular regions is an indication to the need for a thorough examination of other basins [1, 6, 15].Thus, the urgency of the problem is predetermined by a high frequency of various combinations of lesions, unsatisfactory in vivo diagnosis, different, sometimes diametrically opposite tactics. Also today, scarce information, defining the role of non-invasive research methods combined with interventional treatment of patients with lesions of two, three or more arterial beds, which will surely represent the great interest, both from a scientific and practical point of view.Therefore, detection of atherosclerotic lesions of a vascular regions is an indication to the need for a thorough examination of other pools [1, 6, 15].Thus, the urgency of the problem is predetermined by a high frequency of various combinations of lesions, unsatisfactory in vivo diagnosis, different, sometimes diametrically opposite tactics. Also today, scarce information, defining the role of non-invasive research methods combined with interventional treatment of patients with lesions of two, three or more arterial pools, which will surely represent the great interest, both from a scientific and practical point of view.
2. Objective
- To improve the results of treatment of patients with chronic lower limb ischemia in multifocal atherosclerosis by selecting the appropriate surgical approach with using both open and interventional therapies.
3. Material and Methods
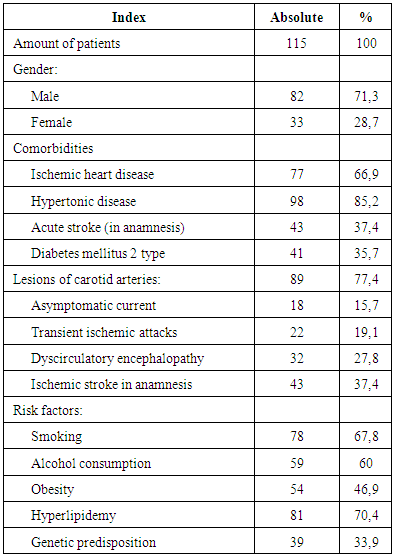
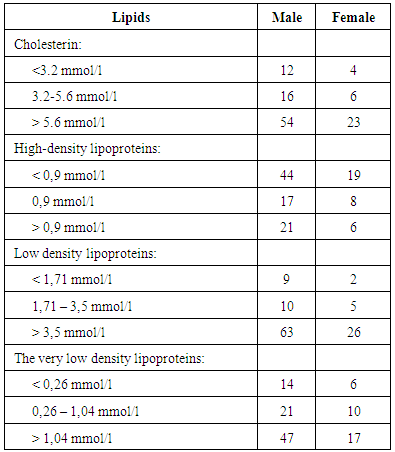
- The study is based on the results of surgical treatment of 115 patients with atherosclerosis several arterial pools who have received the treatment in the Vascular Surgery Department of Second Clinic of Tashkent Medical Academy for the period from 2014 to 2016. The age of patients was from 48 to 82 years (63,3 ± 5,2).The criterion for selection of patients was the presence of lesions of the terminal aorta and lower limb arteries in conjunction with hemodynamically significant lesions of other arterial pools, i.e. chronic ischemia of the lower limbs in advanced atherosclerosis (tab.1).
|
|
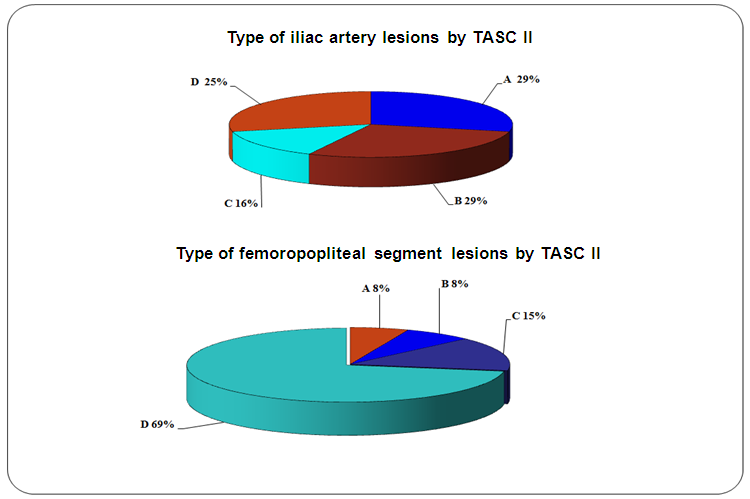 | Figure 1. Distribution of patients by TASC II classification |
4. Results
- 38 patients with chronic lower limb ischemia II B degree in combination with hemodynamically significant carotid stenosis primary prevention of ischemic stroke has been performed, and the subsequent stage of the 22 (57.8%) patients revascularization of lower limb arteries was performed.In 19 (24%) patients with carotid stenosis with critical lower limb ischemia was achieved regression of clinical manifestations of lower limb ischemia using drug therapy, 12 (63.1%) patients carried out the installation of the catheter for prolonged intra-arterial catheter therapy, and then the carotid endarterectomy. Of these, 14 (48.2%) patients on 7-th day performed reconstructive surgery on the arteries of the lower extremities. 5 (17.2%) patients after carotid endarterectomy performed endovascular interventions on the lower limb arteries. 1 (1.2%) patient made high amputation of limbs due to the progression of ischemia. In 1 (1.2%) patient developed acute myocardial infarction with lethal outcome.Selecting the one-stage tactic was based on the impossibility of relief critical ischemia of the lower limbs and of interventional procedures or their ineffectiveness. Simultaneous operations are made in 5 (4.3%) patients with carotid stenosis with critical lower limb ischemia. No complications were observed.In 19 (16.5%) patients with lesions of the carotid arteries and critical lower limb ischemia in the first stage performed endovascular interventions for critical lower limb ischemia, and to 5 (4.3%) of them produced hybrid intervention. 1 (0.86%) patient underwent high amputation with fatal outcome and still 1 (0.86%), - amputation by Sharp.Open interventions in the lower limb arteries with concomitant carotid lesions and critical lower limb ischemia was performed in cases where an alternative intervention was high amputation of the limb. An important condition for the implementation of such interventions were high tolerance of brain to cerebral ischemia, asymptomatic type of chronic cerebrovascular insufficiency, uncomplicated carotid plaque and the absence of hemodynamically significant stenosis of the carotid artery on one side. Open interventions at a critical ischemia of the lower limbs in the first stage performed in 11 (9.5%) patients. All operations on the lower limbs were performed under spinal anesthesia and below of poupart ligament. In 1 (0.86%) of these patients due to ischemia progresses achieved high amputation of the limb.For patients with coronary heart disease important criteria, which influencing to the choice of treatment strategy is coronar reserve, which expressed in decreasing of stroke volume less than 50 ml per minute, left ventricular ejection fraction less than 45%, increase of end-diastolic volume of the left ventricle, the presence of segmental disorders that testified about violation pumping function of the myocardium, threatening cardiac complications in the intra- and postoperative according to echocardiography. Given this, to the patients was indicated coronary angiography for diagnostic purposes. In 6 (5.2%) patients with lesions of the coronary arteries and the arteries of the lower extremities in the first stage performed stenting of the coronary arteries, in the second stage - the reconstruction of the lower extremity arteries. In 2 (1.7%) patients underwent open surgery on the arteries of the lower extremities due to hemodynamically insignificant lesions of the coronary arteries in coronary angiography. In 3 (2.6%) cases performed palliative intervention (thoracoscopic sympathectomy) after coronary artery stenting.The effectiveness of interventions determined on the basis of the absence of acute or new focal neurological changes, changes of myocardium and improves blood flow in the lower extremities. Among the patients we observed only one developed acute myocardial infarction. In assessing of regress of lower limb ischemia we accounted the ankle-brachial index: initially the rate was 0,28 ± 0,04, for 3-4 days after surgery on the arteries of the lower extremities increased to 0,53 ± 0,3 (p <0, 05).
5. Discussion
- Diagnosis and treatment of patients with multivessel lesion disease in atherosclerosis, especially when in the process involved carotid, coronary arteries and the arteries of the lower extremities, is quite a challenge for cardiovascular surgery [5, 14]. In the literature of recent years prevails critical approach to simultaneous interventions in atherosclerosis [2, 6, 7, 11]. The mortality rate, even in hospitals with extensive experience, ranging from 3% [7] to 12% [4, 5, 14].In the course of the work we have formed the following tactics of phasing the operative interventions at multivessel atherosclerosis:• If you have a hemodynamically significant carotid stenosis and chronic ischemia of the lower limbs:1st stage - reconstruction of the carotid arteries2-stage - reconstruction of the lower limb arteries• If you have a hemodynamically significant carotid stenosis and critical limb ischemia:1 stage - relief of critical limb ischemia (pharmacological and interventional)2-stage - reconstruction of the carotid arteries3-stage - reconstruction of the lower limb arteries• If it is impossible to stop the critical ischemia of the lower limbs:1st stage - reconstruction of the lower limb arteries below of poupart ligament under spinal anesthesia (endovascular or combined)2-stage - reconstruction of the carotid arteries• If it is impossible to stop the critical ischemia of the lower limbs:1st stage - reconstruction of the carotid arteries under regional anesthesia2-stage - the reconstruction of the terminal aorta and lower limb arteries (open)• When combined lesions of the coronary arteries and chronic ischemia of the lower limbs:1st stage - coronary revascularization2-stage - reconstruction of the lower limb arteries• When combined lesions of the coronary arteries and the critical lower limb ischemia:1 stage - relief of critical limb ischemia (pharmacological and interventional)2-stage - coronary revascularization3-stage - reconstruction of the lower limb arteries• If it is impossible to stop the critical ischemia of the lower limbs:1st stage - reconstruction of the lower limb arteries occlusive disease following spinal anesthesia (endovascular or combined)2-stage - coronary revascularizationAs we know, the conservative treatment of critical limb ischemia is ineffective even when using modern genetic engineering drugs. According to our research, only 27.5% of patients with marked regression of limb ischemia.Thus, in patients with chronic lower limb ischemia with concomitant lesions of the carotid and coronary arteries it is advisable to conduct prevention of acute focal cerebral infarction and disorders. To obtain satisfactory results, it is necessary to apply a differentiated surgical approach, the choice of which is determined only after careful study of local hemodynamics and evaluation of compensatory possibilities of the affected remote arterial pools. It should try to either medication or minimally invasive methods to stop the chronic ischemia of the lower limbs for the purpose of primary prevention of ischemic cerebral infarction and infarction.This tactic allowed to receive early postoperative good result in 95.5% of cases and the unsatisfactory result of 3.5% of patients. Keeping of the limb in the late postoperative period with a follow-up of 12 months was noted in 94%, and the survival rate of patients with combined lesions of several arterial beds was observed in 88% (Fig. 2, 3).Statistical analysis was performed with using SPSS version 19. The effectiveness of the treatment was assessed on the 6th month after surgery (r≤0.05).
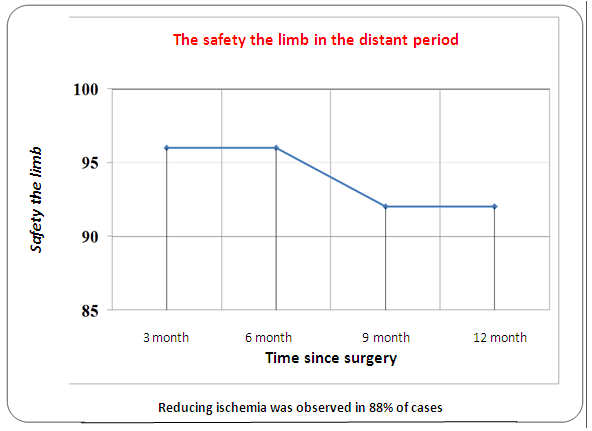 | Figure 2 |
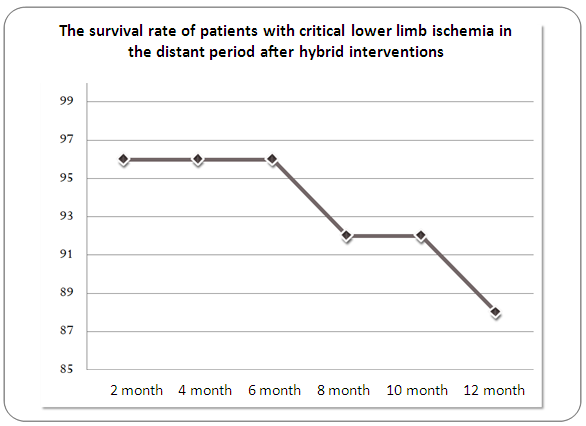 | Figure 3 |
6. Conclusions
- Number of patients with multifocal atherosclerosis who need the surgical treatment is much more than is revealed that dictates an individual approach in the diagnosis and treatment strategies to this category of patients. At the same time, priority should be given to less traumatic interventions1) In the next preference should be given to interventions with the least surgical aggression, including hybrid operations that allow you to perform an optimal correction of two blocks of lesions in patients with critical lower limb ischemia with multifocal atherosclerosis.2) Using of the proposed diagnostic algorithm and stages of surgical intervention significantly improves the detection of multifocal lesions and allows to expand the indications for surgical treatment with the use of combined interventions for the primary prevention of ischemic stroke and acute myocardial infarction.3) Using of interventional procedures in patients with multifocal atherosclerosis for relief of critical lower limb ischemia, correction renovascular hypertension and myocardial ischemia, reduces the risk of focal ischemic complications of vital organs.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML