-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2017; 7(2): 55-60
doi:10.5923/j.ajmms.20170702.03

Serum Calcium Level in Neonates under Phototherapy with and without Head Covering
Abd-Elmagid M. Bayomy1, Ahmed Mahmoud Solaiman2
1Pediatric Department, Al-Azhar University, Assiut, Egypt
2Clinical Pathology Department, Al-Azhar University, Assiut, Egypt
Correspondence to: Abd-Elmagid M. Bayomy, Pediatric Department, Al-Azhar University, Assiut, Egypt.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

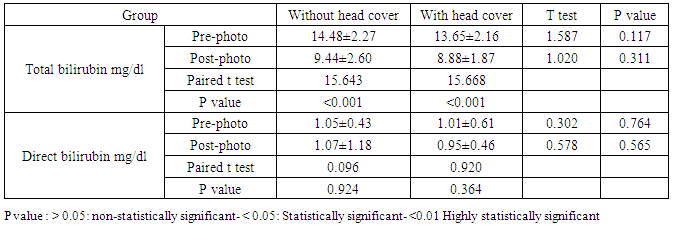
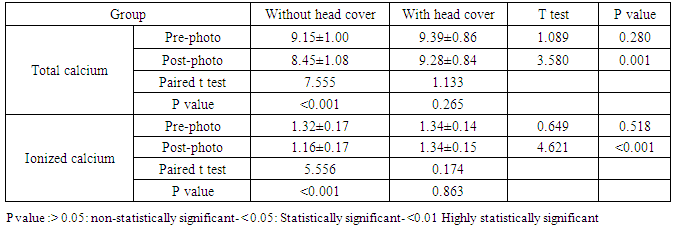
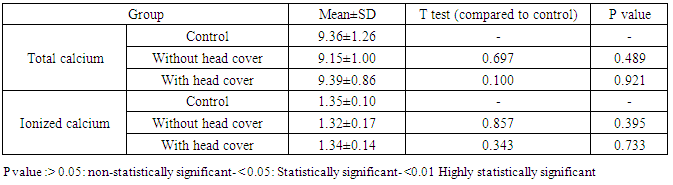
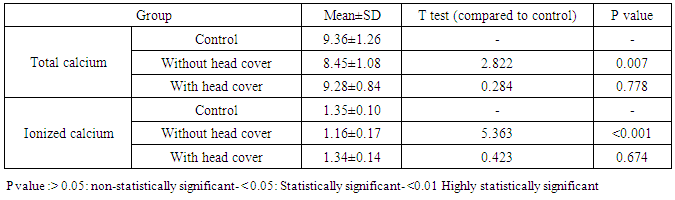
Background: Neonatal jaundice is one of the most common conditions confronting neonatologists daily. About 60% of term and 80% of preterm infants develop jaundice in the first week of life. A lesser known side effect, but potential complication of phototherapy is hypocalcemia. Melatonin stimulates secretion of corticosterone, which decreases calcium absorption by bones. Phototherapy leads to inhibition of pineal gland via transcranial illumination, resulting in a decline in melatonin level and, as a result, hypocalcemia develops. The aim of the study was to determine the effect of head covering of infants under phototherapy on phototherapy-induced hypocalcemia in jaundiced newborns. Patients and methods: we conducted a prospective randomized controlled study at the neonatal intensive care unit (NICU) at Al azhar university hospital Assiut and Sohag Teaching Hospital, during the period from June 2015 till December 2015. The study included 70 icteric neonates under ptototherapy. Total and ionized serum calcium levels were measured pre and 48 hours post exposure to phototherapy. Neonates were randomized and divided into two groups Group I: under phototherapy without head covering. Group II: under phototherapy with head covering. Comparison between these groups was done to detect the effect of hat in phototherapy induced hypocalcemia. A control group of 20 healthy neonates was added to the study to compare total and ionized serum calcium levels in the controls and in the icteric groups under phototherapy. Results: We detected hypocalcemia detected by ionized serum calcium <1.2 mg/dL after 48 hours of phototherapy in 24 cases of our icteric neonates (34.3%). Hypocalcemia was in 17 neonates (48.6%) in group without hats, and in 7 neonates (20%) in group with hats. The difference between groups was statistically significant (P value=0.012). Also, we detected hypocalcaemia with total serum calcium after phototherapy (<8mg/dl) in 18 cases of our icteric neonates (25.7%). Hypocalcemia was detected in 12 neonate (34.3%) in group without hats and in 6 neonates (17.1%) in group with hats. The difference between groups was statistically significant (p=0.035). Comparison between total and ionized calcium levels in the control group and the two icteric groups was done. Pre-phototherapy, there was no statistically significant differences between three groups. While post phototherapy, there was statistically significant differences between total (p=0.007) and ionized (p<0.001) calcium in the control group and group I without head cover. There was no statistically significant differences between total (p=0.778) and ionized (p= 0.674) calcium in the control group and group II with head cover. Our study showed that head covering during phototherapy is an effective, safe, non-invasive and cheap method for preventing phototherapy-induced hypocalcaemia in icterus newborns. Conclusions: we conclude that hypocalcemia is a significant problem in neonates subjected to phototherapy. Total and ionized serum calcium levels should be assessed in newborns treated with phototherapy for 48 hrs or more and managed accordingly.
Keywords: Calcium, Phototherapy, Head covering
Cite this paper: Abd-Elmagid M. Bayomy, Ahmed Mahmoud Solaiman, Serum Calcium Level in Neonates under Phototherapy with and without Head Covering, American Journal of Medicine and Medical Sciences, Vol. 7 No. 2, 2017, pp. 55-60. doi: 10.5923/j.ajmms.20170702.03.
1. Introduction
- Neonatal jaundice is one of the commonest issues affecting newborns. It is observed in up to 60% of term infants and 80% of preterm infants. Clinically, jaundice appears as yellowness of skin due to elevated serum bilirubin (a breakdown product of hemoglobin) levels above 85-120 umol/L, or 5-6 mg/dL. Most jaundice is "physiologic" and self-limited. Physiologic jaundice normally occurs postpartum day 2-3, peaking by the fourth day, and resolving by 7 days. Premature infants have longer duration [1]. In most infants with physiologic jaundice, bilirubin concentrations do not rise to a point that requires treatment. However, in some infants with exaggerated physiological jaundice, and in many infants with pathological jaundice, bilirubin in the blood reaches very high concentrations that put the infant at risk for acute and chronic bilirubin encephalopathy (kernicterus). In these cases, treatment aimed at decreasing bilirubin concentration which is required in order to avoid kernicterus [2]. Phototherapy plays a significant role in the treatment and prevention of hyperbilirubinemia in neonates. This relatively common therapy lowers the serum bilirubin level by transforming bilirubin into water-soluble isomers that can be eliminated without conjugation in the liver [3]. Phototherapy may lead to complications including skin rash, diarrhea, hyperthermia, chills, dehydration, DNA damage to lymphocytes, retinal degeneration, bronze baby syndrome especially in cholestatic jaundice and PDA opening in LBWs and hypocalcemia [4]. There are several theories to explain the effect of phototherapy on calcium metabolism. Phototherapy decreases melatonin level and corticosterone secretion. Melatonin stimulates secretion of corticosterone, which decreases calcium absorption by bones. Phototherapy leads to inhibition of pineal gland via transcranial illumination, resulting in a decline in melatonin level and, as a result, hypocalcemia develops [5]. As hypocalcemia is accompanied by a decrease in serum melatonin concentration, this effect can be prevented by shielding the occiput [6].
2. Subjects and Methods
- This study was conducted at the neonatal intensive care unit (NICU) at Al azhar university hospital Assiut and at Sohag Teaching Hospital, during the period from JUNE 2015 till December 2015. The study included 70 icteric neonates under ptototherapy and included 20 healthy neonates. Inclusion criteria:- Any case with neonatal jaundice under phototherapy including full-term and nearterm infants. Control group included healthy neonates with no apparent disease. Exclusion criteria:-Neonatal sepsis, perinatal asphyxia, Infant of diabetic mother (IDM), neonates in NICU for causes other than neonatal jaundice and those need exchange transfusion. The studied neonates were classified into three groups: Group I (35 icteric neonate): under phototherapy without head covering. Group II (35 icteric neonate): under phototherapy with head covering by a stockinet cap. Control Group (20 healthy neonates): with no exposure to phototherapy. The phototherapy used contains four blue light fluorescent lamps with 20 watts and wavelengths of 410–470 nm. The icteric neonates was placed at a distance of 40–45 cm from phototherapy. All neonates were subjected to the following: 1-History taking with stress on. Prenatal history: maternal diseases as diabetes mellitus, maternal drugs as sulfa orasprin. Natal history: mode of delivery, premature rupture of membrane (PROM), birthtrauma, Asphyxia. Post natal history: history of neonatal convulsions or hypocalcaemia. Family history: Previous sibling with Jaundice or hypocalcaemia. 2-Gestational age: was assessed by New Ballard score. 3-Complete physical examination General examination: general condition, activity, pulse, respiratory rate, temperature and colour (observation of jaundice in cephalocaudal direction). Neurological: examination: anterior fontanelle, muscle tone & reflexes, grasp reflex, Moro reflex and suckling reflex. Anthropometric measures:-weight: using an electronic scale with subject wearing light clothes. - Head circumference: measured with a measuring tape. Signs of hypocalcemia: Jitterness, twitches, apnea, seizures. 4-Investigations: For all icteric patients, the following investigations were done: •Total and direct serum bilirubin level pre and 48hours post exposure to phototherapy. •Total and ionized serum calcium level pre and 48hours post exposure to phototherapy. For control group, total and ionized serum calcium levels were assessed. Sample collection: 2 ml venous blood samples from a periphral vein were drawn from icteric groups under aseptic conditions to determine total, direct bilirubin & total and ionized calcium pre exposure to phtotherapy. Another sample were drawn for the same investigations 48 hours after exposure to phototherapy. For control group sampling was once for assessment of total and ionized calcium levels. Total calcium: Principle: Calcium ions form a highly colored complex with Arsenazo3 at neutral ph. The color which has formed will correspond to the amount of calcium present in the sample. Calcium +2 Arsenazo3àCa-Arsenazo Complex. Reagents: Kit3 ×20ml code A-R0000000007-Reagent: no.3vials×1905ml-Kit6×50ml code A-R0100000301. Reagent: no.6 vials×48.5ml. Precautions: In addition to the eventual risk indications regarding the active components, the reagent my contain inactive components such as preservatives and detergents. The total concentreation of these components is lower than the limits reported by the 67/548/EEC and 1999 /45/EC directives and following modifications and amendments. However it is recommended to handle reagents carefully and avoid contact with eyes, skin and mucous membranes. Sample collection: type of sample storage: Heparinized plasma or serum samples should be used. Do not use anticoagulants containing citrates, oxalates or EDTA as these tend to remove the calcium through formation of complexes. The samples can be stored for 7 days at 20-25°C, 3 weeks at 4-8°C, 8 months at -20°C. Procedudure: Quality control: Human control serum with known levels of Calcium is commercially available for quality control purposes. Data sheets are included, listing the values and the confidence limits. Normal and abnormal control sera are available from I.S.E. S.r.I "normal control serum "code R0400000006 and "pathological control serum" code R0400000106. Obtained values must be within the range of acceptability. If erratic results occur, the following pointd should be checked: *cleanliness of glassware *wavelength setting. *Expiration date of reagents. Automation: This kit, through developed and manufactured to be used as manual assay and with I.S.E. S.r.I analyser, can be used also with other analyzer able to meet the specifications indicated in section "reaction conditions- Test procedure" Applicatoin sheets are available for automatic instruments. All applications not explicity approved by I.S.E. S.r.I. cannot be guaranteed in terms of performance, and must therefore be established by the operator. Calibration stability: For the instruments series Miura, the calibration is recommended to be done every 10 days. Calibration: For calibration use the "Multicalibrator" I.S.E S.r.I code R0300000006. Traceability: The calcium value is reported in the package insert supplied with the "multicalibrator". Ionized calcium: AFT500 Electrolytes Analyzer: Analyzer for any combination of k+, Na+, Cl-, Li+ - Sample type: plasma, serum, whole blood, urine. Bilirubin (total and direct): Intended Use: Spectrum diagnostics bilirubin reagent is intented for in-vitro quantitative, diagnostic determination of bilirubin in human serum on both automated and manual systems. Method: Colorimetric Diazo method. Assay principle: The total bilirubin concentration is determined in prescence of caffeine by the reaction with diazotized sulphanic acid to prdduce an intensely colored diazo dye (560-600nm). The intensity of color of this dye formed is proportional to the concentration of total bilirubin. Direct bilirubin is determined in absence of caffeine by the direct reaction with diazotized sulphanilic acid to form red-colored azobilirubin, the color intensity of which measured at 546nm is proportional to the concentration of the direct bilirubin in the sample. Statistical Methods: Statistical package for social sciences (IBM-SPSS), version 22 IBM- Chicago, USA was used for statistical data analysis. Data expressed as mean, standard deviation (SD), number and percentage. Mean and standard deviation were used as descriptive value for quantitative data. Pearson Chi square test was used to compare percentages of qualitative data. Student t test was used to compare the means between two groups, and one-way analysis of variance (ANOVA) test was used to compare means of more than two groups. Pearson correlation test was used to compare two quantitative variables. The value of (r) is explained in the following figures: r 0-0.4
 weak correlation - r 0.4-0.7
weak correlation - r 0.4-0.7  moderate correlation - r 0.7-1
moderate correlation - r 0.7-1  strong correlation-r positive
strong correlation-r positive  positive correlation - r negative
positive correlation - r negative  negative correlation. For all these tests, the level of significance (P-value) can be explained as: No significance P > 0.05 - Significance P < 0.05 - High significance P < 0.001.3.
negative correlation. For all these tests, the level of significance (P-value) can be explained as: No significance P > 0.05 - Significance P < 0.05 - High significance P < 0.001.3. 3. Results
|
|
|
|
|
|
4. Discussion
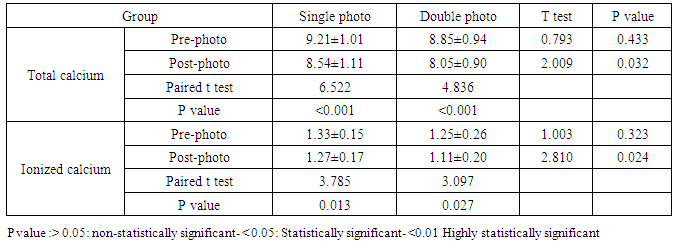
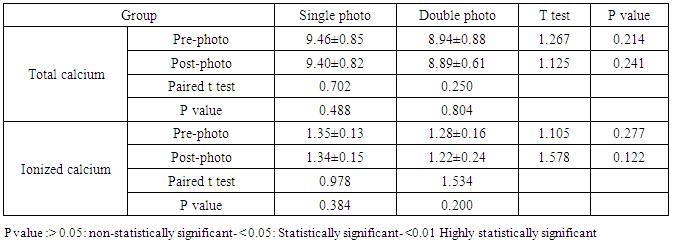
- We conducted a randomized controlled study included 70 full-term neonates with hyperbilirubinemia treated with phototherapy and 20 full-term healthy neonates. In our study, the mean body weight was 2.84 kg±0.58, mean gestational age was 38 wk ±1.41, mean head circumference was 33.9 cm±1.18, mean age was 6 days ±5.41 and mean total bilirubin in icteric neonates on admission was14 mg/dl ±2.24. Icteric Neonates were randomized and divided into two groups. Group I: under phototherapy without head covering. Group II: under phototherapy with head covering. Comparison between total and ionized calcium levels before and after 48 hours phototherapy in each group was done to detect the change in serum calcium level induced by phototherapy and the effect of head covering on phototherapy-induced hypocalcemia in jaundiced newborns. Comparison between total and ionized calcium levels in the control group and the two icteric groups was done. Pre-phototherapy, there were no statistically significant differences between three groups. While post phototherapy, there was statistically significant differences between total (p=0.007) and ionized (p<0.001) calcium in the control group and group I without head cover. There was no statistically significant differences between total (p=0.0.778) and ionized (p= 0.674) calcium in the control group and group II with head cover. As regard ionized calcium, we detected hypocalcemia with ionized calcium (<1.2 mg/dL) in 24 cases of our icteric neonates (34.3%). Hypocalcemia was in 17 neonates (48.6%) in group without hats, and in 7 neonates (20%) in group with hats. The difference between groups was statistically high significant. (P value= 0.012). In group I, the difference between ionized calcium level before and after 48 hours phototherapy (1.32±0.17 and 1.16±0.17) was statistically significant (p value<0.001). In group II, the difference between ionized calcium level before and after 48 hours phototherapy (1.34±0.14 and 1.34±0.15) was statistically insignificant (p value=0.863). Our results are in agreement with the following studies: Nishant Prabhakar et al, (2016) [7], In their study they observed ionic calcium level instead of total serum calcium level which is more reliable marker of hypocalcaemia. They observed a significant decrease in serum ionic calcium level in study group with phototherapy while in control group without phototherapy there was no significant difference observed after 48 hours of phototherapy. Between 24 cases 66.67% developed hypocalcaemia while among control group only one newborn had hypocalcaemia and there was a significant difference observed between cases and controls (P=0.00016). Rajesh Kumar et al, (2011) [8] observeda significant fall in ionized calcium level in 66.6% of term & 80% of preterm neonates after 48 hours of exposure to phototherapy in the study group. There was higher prevalence of hypocalcaemia than our study in Sethi et al, (1993) [9] who studied the effects of phototherapy in 20 term & 20 preterm hyperblirubinemic neonates. They observed that 75% of term & 90% of preterm neonates developed hypocalcaemia after phototherapy. There was a highly significant fall in the total as well as ionized calcium levels in the study group in contrast to the control group. We detected hypocalcaemia with total serum calcium after phototherapy (<8mg/dl) in 18 cases of our icteric neonates (25.7%). Hypocalcemia was in12 neonate (34.3%) in group without hats and in 6 neonates (17.1%) in group with hats. The difference between groups was statistically significant (p=0.035). In group I without hats, the difference between total calcium level before and after 48 hours phototherapy (9.15±1.00 and 8.45±1.08) was statistically significant (p value<0.001). In group II with hats, the difference between total calcium level before and after 48 hours phototherapy (9.39±0.86 and 9.28±0.84) was statistically insignificant (p value = 0.265). Hat blocked the effect of phototherapy by preventing passage of light to head of infant. Our results in hypocalcaemia detected by total calcium are in consistent with the following studies: Mohammed Hamed Bahbah, et al, (2015) [10] found that neonates with hypocalcemia represented 13 cases (26%) out of 50 neonates. Arora S et al, (2014) [11] concluded thatout of 56 term neonates, 30 (56%) at the end of 48 hrs developed hypocalcaemia in term babies. Eghbalian and Monsef, (2002), [12] showed that the difference between pre- and post-phototherapy plasma calcium levels were found to be statistically significant (p<0.05). The decline in plasma calcium level at times reached hypocalcaemia threshold. Mean±SD serum calcium level decreased significantly (p<0.001) from a baseline value of 9.85±1.23 mg/dl (before phototherapy) to 9.09±0.93 mg/dl, after phototherapy. Our results in hypocalcemia prevalence are higher than the prevalence of hypocalcemia in Ehsanipoor's, (2008), [6], where (15%) neonates developed hypocalcemia after starting phototherapy. Our results in hypocalcemia prevalence are also higher than the study done by Abdolmajid Nazemiet al, (2015), [13], where among the 100 newborns studied, 54% had decreased calcium levels after phototherapy. The prevalence of hypocalcemia was 9% only. Similarly, in Karamifar's, [5], study (8.7%) of term neonates developed hypocalcaemia 48hrs after phototherapy [5]. Also, In Paymaneh et al, (2013), [14], study, 83 (56%) newborns had decline in serum calcium level, and only 7% had hypocalcaemia. There was a significant difference between serum calcium level before and after phototherapy (P=0.03). In Fatemeh Haji, [15], results: Fifteen neonates (7.5%) developed hypocalcaemia. After 48 hours of phototherapy, there were significant differences between serum calcium levels from baseline values of 9.46±0.8 mg/dL to 9.12±0.83 mg/dL and they mentioned in conclusion: although phototherapy induces hypocalcaemia in term infants, but the incidence of phototherapy-associated hypocalcaemia is not too much [15]. As regard our results in head covering effective protection are in consistent with the following studies: In a randomized controlled study for effect of head covering on phototherapy- induced hypocalcaemia in Icterus Newborns 72 full-term icterus newborns 14 (38.8%) newborns in the control group without head cover and 5 (13.8%) in the case group with head cover hadhypocalcemia after phototherapy. A significant difference was found between the incidence of hypocalcemia in these two groups (P=0.03) [16]. In Ezzeldin Z. et al, (2015), [17], study, there was no difference in the mean Ca levels in the two groups on admission. However, after 48 hours of phototherapy, there was a trend toward an increased Ca level in the group with the hat; 8.74±0.95 mg/dLvs 8.51±0.24 mg/dL in the control group without hat. Moreover, there was a statistically significant decrease in the incidence of neonates with hypocalcemia in Group B (with hat) in only six cases (9.7%), compared to 15 cases (24.2%) in Group A (without hat; P = 0.031). There was a statistically significant difference between the prevalence of hypocalcemia in group A without hat (77.77%) and group B using hats (22.22%) (p<0.001) [6]. This proves protective role of head covering in prevention of phototherapy-induced hypocalcaemia in agreement with our study. Zangoei , et al., (2016), [18]: Results of their study showed that the average of calcium level was significantly higher in the infants of test group with hat 48 hours after starting phototherapy compared to the control group without hat [P<0.001]. In other words, the incidence of hypocalcemia in infants with phototherapy with hat was significantly lower than infants with routine phototherapy. Hypocalcemia accounted for 11% and 24.4% in term neonates with covered heads and uncovered heads, respectively with significant difference (p0.02) in Maha A. Nouh, et al, (2013) [19]. Our results are not in agreement with Afshin, et al., (2016), [20], where in 80 newborn cases under phototherapy, the mean serum Ca levels before and after phototherapy were 9.37 ± 0.86 and 9.25 ± 0.61 mg/dL, respectively (P = 0.171, paired t-test). They found no significant difference between se- rum Ca levels before and after phototherapy. Therefore, they do not suggest Ca prophylaxis before and during phototherapy. In the present study, there is more decrease in total (p=0.023) and ionized serum calcium (p=0.014) level post photo therapy in cases treated with double phototherapy than with single phototherapy. In group I without hats, there was more decrease in the total (p= 0.032) and ionized serum calcium level (p= 0.024) post photo therapy in cases treated with double phototherapy than those treate with single phototherapy. In group II with hats, there was no significant difference in the reduction of the total (p= 0.241) and ionized (p= 0.122) serum calcium level post photo therapy in cases treated with double phototherapy than those treated with single phototherapy. Our results are in consistent with Arora S et al, (2014) [11] in which 14 (42%) term babies developed hypocalcemia under SSPT while under DSPT, 16 (76%) term babies developed hypocalcaemia. At 48 hrs, hypocalcemia occurred more commonly under double stranded phototherapy (DSPT) than single stranded phototherapy (SSPT). Fall in serum calcium level is statistically significant since t value is more than table value of t at 95% confidence level (t. 0.05 = 2.084). No side effects were detected from using hat during this study. Hat is the safest method in prevention of phototherapy-induced hypocalcemia as it is non-invasive method and keeps the normal and physiological pattern of melatonin secretion. Using prophylactic calcium supplementation can cause some side effects including gas, bloating, constipation, or a combination of these symptoms. Calcium carbonate appears to cause more of these side effects than calcium citrate. Also, intravenous calcium therapy may lead to bradycardia, cardiac arrest, and necrosis. On the other hand, monitoring intravenous infusions of calcium is difficult because of the shortage of trained staff [6]. We recommend using this hat in preterm neonates as well, as the incidence of phototherapy-induced hypocalcemia is higher in the latter than in full-term neonates. This may be due to the higher penetration of light in premature infants [5]. Future studies including preterm and full-term neonates, comparing the results between treatment, covering the heads and prophylactic calcium supplementation will strength our results.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML