-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2017; 7(1): 7-10
doi:10.5923/j.ajmms.20170701.02

Comparative Efficiency of Surgical and Intra-Coronary Revascularization in Patients with Instable Angina against the Background of Diabetes Mellitus
B. F. Mukhamedova, D. A. Alimov, Kh. M. Tursunov, M. A. Obeid, A. A. Abdurakhmonov
Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
Correspondence to: B. F. Mukhamedova, Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

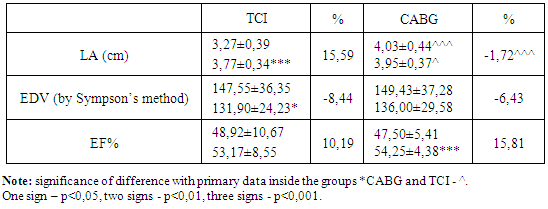
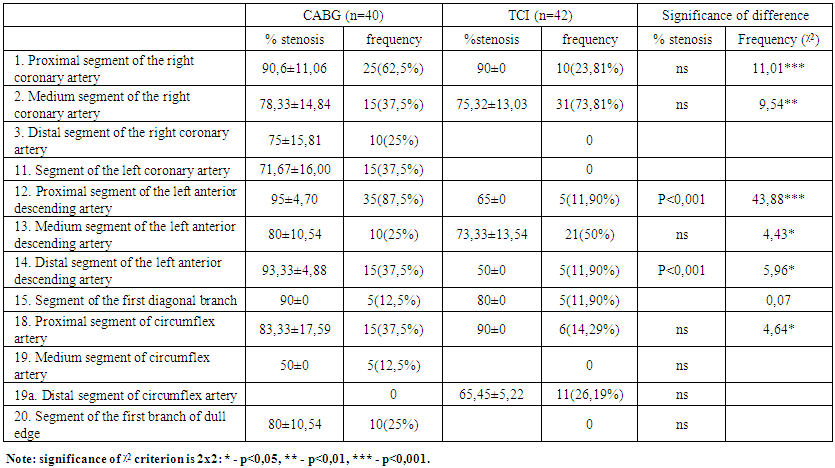
Goal of investigation: to define long-term angiographic and hemodynamic efficiency of different methods of revascularization in patients with instable angina against the background of diabetes mellitus (DM). Material and methods: 82 diabetic patients with instable angina were included to investigation. 40 of them (group of coronary artery bypass grafting (CABG)) were undergone surgical revascularization (during 1 month after CHD destabilization episode), the rest of 42 patients (group of transcutaneous coronary intervention (TCI)) – were performed stenting of coronary arteries (immediately after angiography). Initially and 12 months after revascularization all patients were performed echocardiographic investigation (EchoCG) and control coronaroangiography. Conclusion: Investigation has proved that surgical revascularization of the patients with DM provides fuller coronary perfusion by the 12th month of observation in compare with TCI. It promotes the reduction of left atrium (LA) size which is one of the indices of LA full pumping function. In the TCI group LA size has been decreased. It testifies the keeping and progressing of myocardial failure. At the same time both methods of revascularization have promoted comparable improvements of the left ventricle (LV) end diastolic volume (EDV) and ejection fraction of LV (EF LV) indices.
Keywords: Unstable angina, Diabetes mellitus, Coronary artery by-pass grafting, Coronary arteries stenting
Cite this paper: B. F. Mukhamedova, D. A. Alimov, Kh. M. Tursunov, M. A. Obeid, A. A. Abdurakhmonov, Comparative Efficiency of Surgical and Intra-Coronary Revascularization in Patients with Instable Angina against the Background of Diabetes Mellitus, American Journal of Medicine and Medical Sciences, Vol. 7 No. 1, 2017, pp. 7-10. doi: 10.5923/j.ajmms.20170701.02.
- Current level of medicine provides revascularization as treatment standard of coronary heart disease (CHD). In the case of instable angina (IA) in consideration of atherosclerotic plaque instability which is the base of pathogenesis, revascularization is a key point of the therapy. There are continuous debates in the literature about which revascularization method is more preferable at IA, especially at the presence of background disease such as diabetes mellitus (DM) which activates pro-inflammatory reactions. As some investigations showed, the frequency of end points in patients with DM were significantly higher than in patients without metabolic disorders even after revascularization [1]. At the same time, in patients with DM surgical revascularization had more positive effect on 10-year survival rate in compare with coronary angioplasty. Patients with monovascular lesion (identical results independently from revascularization method) or patients with a high operation risk (significantly better results after angioplasty) made up an exception [2].Object of the research is to define long-term angiographic and hemodynamic efficiency of different revascularization methods in patients with instable angina against the background of diabetes mellitus (DM).
1. Material and Methods
- 82 patients with instable angina which has been developed against the background of DM were included to the investigation. Only those patients who were undergone diagnostic coronaroangiography and who had indications for revascularization were included to investigation. 40 of them (CABG group) were performed surgical revascularization (during one month after CHD destabilization episode) and the rest of 42 patients (group of transcutaneous coronary intervention (TCI)) – were performed stenting of coronary arteries (immediately after angiography). The mean age of patients made up 58,84±3,28 years. All patients were performed echoargiographic investigation (EchoCG) and control coronaroangiography primary and 12 months after revascularization. EchoCG determined the sizes of heart left cavity, an indexed mass of left ventricle myocardium to the area of body surface, parameters of left ventricle myocardium global systolic function (ejection fraction - LV EF). TIMI coronary blood flow scheme has been used for the estimation of angiography results (figure 1).
 | Figure 1. Scheme of TIMI coronary blood flow |
2. Results and Discussion
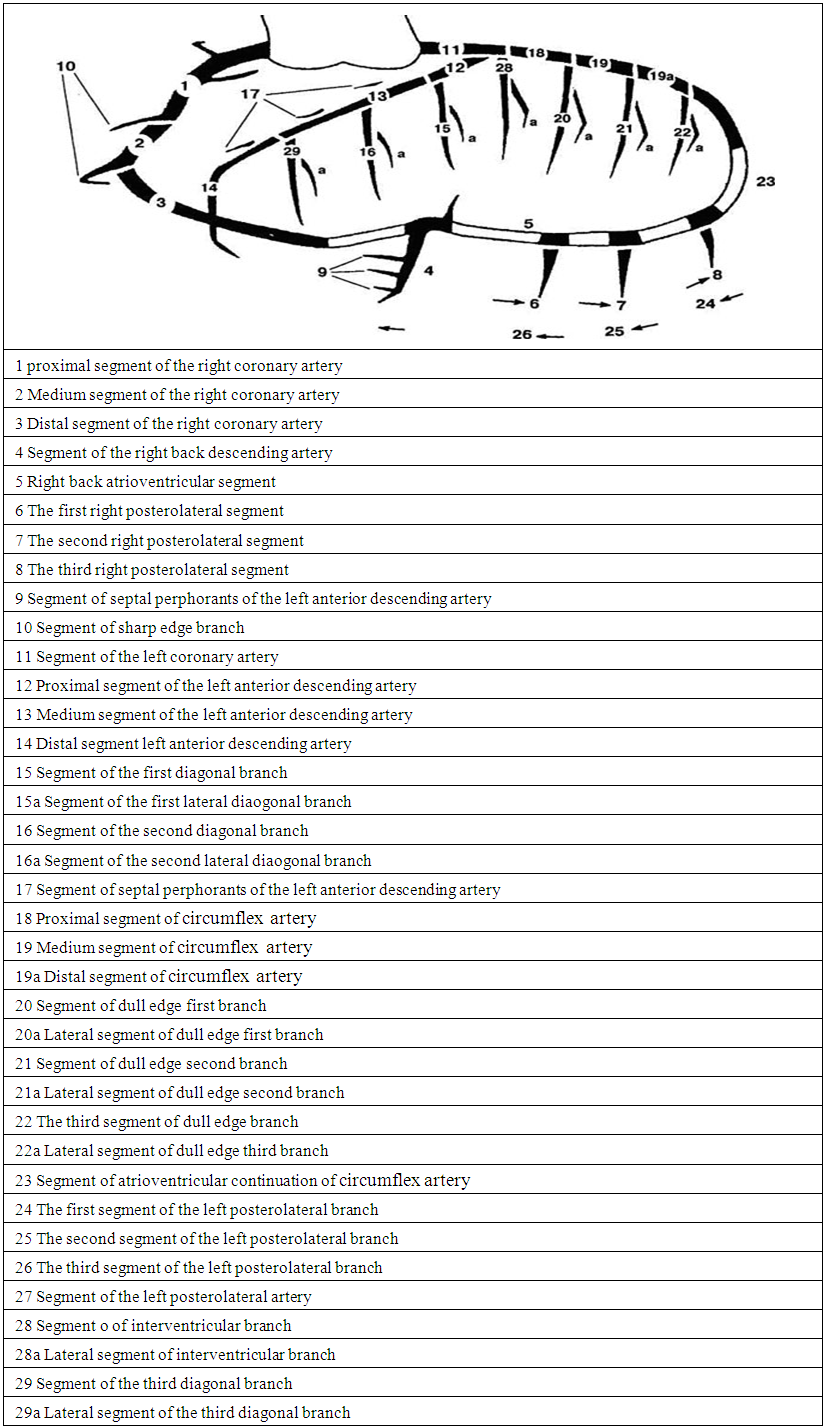
- Primary performed diagnostic coronaroangiography revealed more hemodynamically significant stenosis in patients who required surgical revascularization in compare with those ones who were undergone coronary arteries stenting (4,00±1,31 vs 2,24±1,19 stenosis, p<0,001). The following differences by anatomic character of coronary by-pass lesion were registered (as it is presented in table 1): patients with left coronary artery trunk involvement were not included to TCI group (37,5% of such patients were in CABG group), the lesions of right coronary artery distal segment were not also registered in that group (25% in CABG group), involvement of circumflex artery medium segment (there were 12,5% cases in CABG group) and dull edge first branch segment (25% cases of CABG group), and there was not an involvement of circumflex artery distal segment in CABG group (26,19% patients of TCI group). Stenting was more frequently performed on the right coronary artery medium segment (73,81% vs 37,5%, p<0,01) and on the medium segment of anterior interventricular artery (50% vs 25%, p<0,05).
 | Table 1. Localization of coronary artery stenosis in patients with CHD against the background of DM subject to the requirement in revascularization |
|
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML