-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2016; 6(6): 182-185
doi:10.5923/j.ajmms.20160606.04

Minimally Invasive Surgery in Restoring Reproductive Function of Female Infertility Caused by Benign Ovarian Structural Changes
Shukurov Farkhad Ishkulovich
Associate Professor, Department of Obstetrics and Gynecology, Tashkent Medical Academy, Uzbekistan
Correspondence to: Shukurov Farkhad Ishkulovich, Associate Professor, Department of Obstetrics and Gynecology, Tashkent Medical Academy, Uzbekistan.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the study: to assess the effectiveness of advanced minimally invasive laparoscopic surgical interventions in the treatment of women with infertility due to a benign structural changes of the ovaries. Material and methods: A survey of 270 patients with infertility who underwent in operation in gynecology department of obstetric complex № 9 in Tashkent in 2014-2016. The average age of patients was 25.8±098 years. Primary infertility suffered 160 (59.2%), the secondary - 110 (40.7%) patients. The duration of infertility was from 2 to 9 years. To clarify the causes of infertility all patients were conducted a comprehensive survey that included clinical, laboratory, hormonal, bimanual, microbiological examination, transvaginal ultrasound scan, hysterosalpingography, laparoscopy and hysteroscopy. Endosurgical treatment of patients with infertility was carried out by two methods: laparoscopic and hysteroscopic. Results: As a result of investigation of 120 women (44.4%) identified infertility due to follicular ovarian cysts and 120 (44.4%) of infertility associated with impaired ovulation - polycystic ovary syndrome (PCOS). It should be noted that 80 infertile women (30.0%) mentioned a combination of 2 to 3 factors that violate the reproductive function. During laparoscopy the patients with infertility due to a benign structural changes of the ovaries, revealed various pathological changes in the fallopian tubes: 24 (10%) had adhesions in the fimbria tract, 6 (2.5%) was determined by the obstruction of the fallopian tube in the proximal. 3 patients (1.25%) had determined adhesion process 2 - 3 degrees of severity. When hysteroscopic study, 30 women with benign structural changes of the ovaries 26 (10.8%) of women detected intrauterine pathology: chronic endometritis - 11 (4.6%), synechia in the uterus - 5 (2.1%), endometrial hyperplasia - in 4 (1.6%), foreign bodies of the uterus in the form of silk sutures after cesarean section 6 (2.5%). Conclusions: The effectiveness of resection of the ovaries in PCOS is increased 1.5 times compared to electrocauterisation. The restoration of women fertility in with benign structural changes of the ovaries amounted to 87.5%, undergoing endosurgical operation in PCOS and cystectomy. A differentiated approach to the choice of method of surgical intervention depending on the kind of benign structural changes of the ovaries. Combined laparoscopy hysteroscopic study allows to identify and eliminate the causes of uterine infertility.
Keywords: Benign structural changes of the ovaries, Laparoscopy, Hysteroscopy, Reproductive function
Cite this paper: Shukurov Farkhad Ishkulovich, Minimally Invasive Surgery in Restoring Reproductive Function of Female Infertility Caused by Benign Ovarian Structural Changes, American Journal of Medicine and Medical Sciences, Vol. 6 No. 6, 2016, pp. 182-185. doi: 10.5923/j.ajmms.20160606.04.
Article Outline
- The development of effective methods of overcoming infertility is now the most important public health and social problem. This is due to a high rate of infertility, its adverse impact on the demographic situation in the country, the psychological climate in the family and social adaptation couple [1, 2]. One of the infertility treatment is the use of endosurgical technology, the pregnancy rate after that ranges from 21% to 30% [3, 4]. Diagnostic value of endoscopic methods in identifying the causes of women is fertility problems is extremely high, reached 97.6%. The effectiveness of surgical treatment of women reproductive age with various gynecological diseases increased significantly after the introduction into clinical practice of new technologies with the use of endoscopic techniques [5, 6]. However, the controversial issues remain of the use of certain technical methods of surgery, different surgical accesses, a new technical means [7, 8]. In connection with the current debate about the treatment of female infertility due to benign structural changes in the ovaries, it is highly relevant to specify the role and place of endoscopic surgical treatment of patients with infertility in the modern world.
1. The Aim of the Study
- The aim of the study was the evaluation of the effectiveness of modern minimally invasive endosurgical surgical interventions in the treatment of female infertility caused by benign ovarian structural changes.
2. Materials and Methods
- A survey of 270 patients with infertility who underwent in operation in gynecology department of obstetric complex № 9 in Tashkent in 2014-2016. The average age of patients was 25.8±098 years. Primary infertility suffered 160 (59.2%), the secondary - 110 (40,7%) patients. The duration of infertility was from 2 to 9 years. To clarify the causes of infertility all patients were conducted a comprehensive survey that included clinical, laboratory, hormonal, bimanual, microbiological examination, transvaginal ultrasound scan, hysterosalpingography, laparoscopy and hysteroscopy. Endosurgical treatment of patients with infertility was carried out by two methods: laparoscopic and hysteroscopic. Laparoscopic surgery was performed by standard methods using equipment of "Karl Storz". Hysteroscopic surgery was performed using an apparatus «Karl Storz» in liquid simultaneously with or separately laparoscopy. Depending on the used operative method, the patients were divided into 2 groups: all 240 patients had the operation on the ovaries by laparoscopy; other 30 patients had by hysteroscopy. In order to assess the effectiveness of various techniques in reproductive surgery there were used the following indicators according to the survey: frequency of recovery of menstrual function and frequency of uterine pregnancy. The obtained facts were processed with the help of statistical software package "Statistic 6.0".
3. Results and Discussion
- As a result of investigation of 120 women (44.4%) identified infertility due to follicular ovarian cysts and 120 (44.4%) of infertility associated with impaired ovulation - polycystic ovary syndrome (PCOS). It should be noted that 80 infertile women (30.0%) mentioned a combination of 2 to 3 factors that violate the reproductive function. During a laparoscopy was discovered characterized by the following signs PCOS: ovaries of a pearl-gray color, smooth, shiny, taut surface with a characteristic vascular pattern or looped vessels, the presence of undercapsular translucent cysts with a diameter of from 0.3 to 1sm, dense or uniformly thickened shell. Resection of the ovaries with toothed forceps, found small cysts with a diameter of 0.3 - 2 sm with clear or yellowish contents (number of cysts in each ovary was usually equal to from 10 to 15). During a laparoscopy, follicular ovarian cysts, the tumor was smooth - and thin-walled unilocular formation of rounded, containing transparent light yellow liquid, with a diameter of from 50 to 80 mm, located mostly on the side or posterior from the uterus. When follicular cysts were produced in the husking of the capsule of the cyst - cystectomy, but with PCOS commonly employed by 2 options laparoscopic surgery: electrocauterisare (30 patients) and partial resection of the ovaries (90 patients). The laparoscopic electrocauterisation of polycystic ovaries has been performed with using a monopolar needle electrode. Ovarian electrocautery conducted, as for as possible, all the fine-cystic inclusions. Partial resection of the ovaries was performed in the following nay: the ovary for free captured pole toothed forceps, and depending on the size of the incision was made around the tongs - the holders of the distance necessary to remove the desired amount of tissue. Excision of tissue is about 0.5 to 1 sm ovarian tissue. During laparoscopy the patients with infertility due to a benign structural changes of the ovaries, revealed various pathological changes in the fallopian tubes: 24 (10%) had adhesions in the fimbria tract, 6 (2.5%) was determined by the obstruction of the fallopian tube in the proximal. 3 patients (1.25%) had determined adhesion process 2 - 3 degrees of severity. (Fig 1)
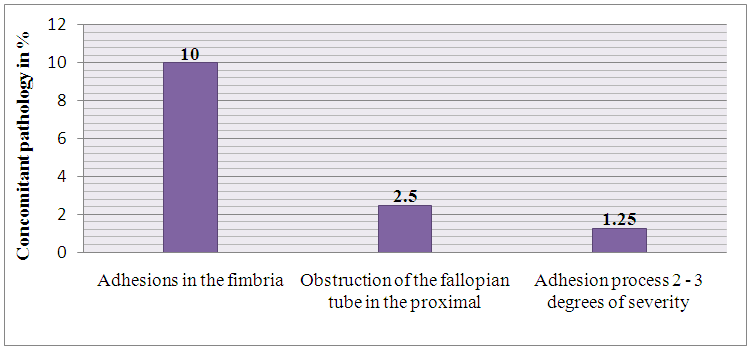 | Figure 1. Concomitant pathology identified during laparoscopy of patients with benign structural changes of the ovaries |
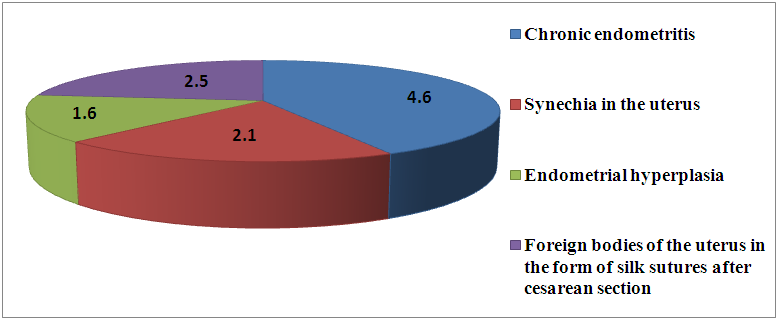 | Figure 2. The patients with benign structural changes of the ovaries were identified types of pathology during hysteroscopy |
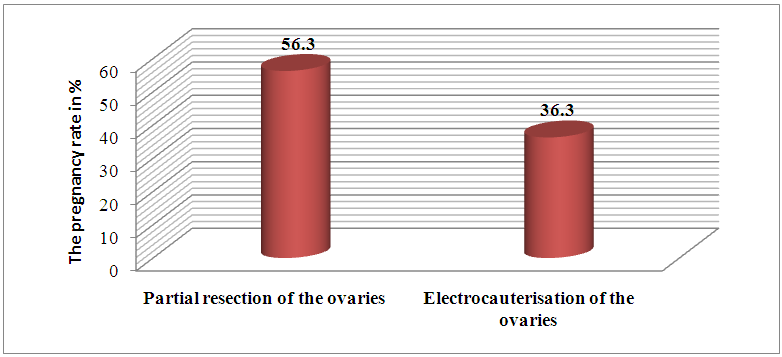 | Figure 3. The pregnancy rate in patients with PCOS, depending on the type of surgery on the ovaries |
4. Conclusions
- 1. To increase the effectiveness of treatment of patients with infertility due to a benign structural changes of the ovaries, early detection of diseases and the use of minimally invasive surgical procedures in the early stages of the disease.2. The effectiveness of resection of the ovaries in PCOS is increased 1.5 times compared to electrocauterisation. The restoration of women fertility in with benign structural changes of the ovaries amounted to 87.5%, undergoing endosurgical operation in PCOS and cystectomy. 3. A differentiated approach to the choice of method of surgical intervention depending on the kind of benign structural changes of the ovaries. Combined laparoscopy hysteroscopic study allows to identify and eliminate the causes of uterine infertility. 4. Hysteroscopy is a highly effective method for diagnosing intrauterine womens pathology of reproductive age and can be used as a screening method of examination in women with infertility caused by structural changes of the ovaries, in some cases, as surgery without additional traumatization of the cervical canal and cervix.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML