-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2016; 6(6): 176-181
doi:10.5923/j.ajmms.20160606.03

Ophthalmological Complications from Diabetes Mellitus: The Organization of Medical Care and Peculiarities of Disability Formation in Tashkent
S. A. Djamalova1, S. T. Iskandarova1, A. S. Babadjanov2
1Department of Public Health Organizations and Health Management, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
2Department of General Practice Therapy, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Correspondence to: S. A. Djamalova, Department of Public Health Organizations and Health Management, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The state of organization of medical aid for patients suffering from diabetes mellitus at the first, ambulatory-policlinic stage has been studied with the aim of preventing its ophthalmological complications. An opinion poll held among general practice doctors, endocrinologists and ophthalmologists, as well as among patients, showed that level of the work of family polyclinic doctors for prophylaxis and early treatment of ophthalmological complications from diabetes mellitus is not quite satisfactory. There are also presented ten-year data on the disability caused by ophthalmodiabetes, peculiarities of its formation depending on a disability group, disabled person’s age, the type of diabetes mellitus as well as a frequency of its detection by year. It is shown that the level of disability from ophthalmological complications of diabetes mellitus is relatively low, however, active working age people with a severe degree of disability, i.e. total loss of sight, prevail among the disabled people. In such cases, as a rule, not only the sick person himself drops out of labor activity, but some of their family members has to nurse him that causes significant economic loss.
Keywords: Sight-disability, Ophthalmological complications from diabetes mellitus
Cite this paper: S. A. Djamalova, S. T. Iskandarova, A. S. Babadjanov, Ophthalmological Complications from Diabetes Mellitus: The Organization of Medical Care and Peculiarities of Disability Formation in Tashkent, American Journal of Medicine and Medical Sciences, Vol. 6 No. 6, 2016, pp. 176-181. doi: 10.5923/j.ajmms.20160606.03.
Article Outline
1. Introduction
- At the present time diabetes mellitus (DM) ranks among the paramount medical and social problems all over the world. According to the International Diabetes Federation, currently there are more than 300 million people with diabetes worldwide and, as predicted, by 2030 this number will additionally increase by 67% [2, 3].One of the most frequent and severe DM complications is diabetic ophthalmopathy. Among the DM patients, a risk of blindness increases 25-fold as compared to the population. Most dangerous of them is believed to be diabetic retinopathy (DR) which is one of key causes of total loss of sight among the people of active working age between 20 and 65 in the economically developed countries [1, 2, 4].A similar situation can be observed in Uzbekistan. According to experts of the CIS Executive Committee, over the last 10 years, in our country the number of DM patients annually increases by 8%. So, according to the data of the Republican Center of Endocrinology under the Ministry of Health of the RUz, in the Republic the number of DM patients amounts to about 130 000, however, taking into account that not less than 2% of the Central Asian population suffer from DM while the population of Uzbekistan amounts to about 30 million people, the actual number of people sick with DM is, at least, six time larger and, as estimated by the WHO experts, it amounts to, at least, 800 000. It is expected that by 2030 this number will exceed 1.5 million [5-7].The reformation of the public health-care being implemented in Uzbekistan from 1998, has radically transformed the system of health care delivery to the republic population. According to a new model of health-care organization, it is just at the primary stage of ambulatory-policlinic treatment that the main bulk of medical services are provided including the preventive therapy of ophthalmological complications from DM. At the present time, it has become necessary to assess efficiency and rationality of organization of medical aid to the patients with diabetic ophthalmopathies in our country. Along with this, the problem of incapacitation caused by ophthalmological complications from DM, peculiarities of its formation and structure in Uzbekistan.
2. The Research Objective
- In order to determine guidelines for reduction of disability caused by ophthalmological complications from DM, it is envisaged to study and assess the quality of medical aid (preventive therapy) for ophthalmological complications from DM provided at the ambulatory-policlinic stage and also study the factors influencing the primary and recurrent disability caused by this pathology in Tashkent over 2003-2012.
3. Materials and Methods
- In order to study and assess the primary health care of patients with DR a questionnaire survey was held among 711 doctors of Tashkent city family polyclinics. The group of respondents consisted of general practice doctors (82.8%), endocrinologists (9.6%) and ophthalmologists (7.6%). Their employment experience in the same occupation ranged from 7 months to 42 years. We have also conducted an opinion poll among 154 DM patients who were undergoing medical examination or treatment in the city clinics and had DR in their anamneses. Among the respondents there were 12.6% of patients with type 1 DM and 87.4% patients suffered from type 2 of the disease; 89 patients were residents of Tashkent and the rest (65 people) – of the Tashkent region and other regions of the Republic.We have analyzed the data of 348 acts of examination of patients, whose disability resulted from ophthalmological complications from DM, by specialized ophthalmological medical-labor expert commissions (MLEC) of Tashkent over 10 years. The study was complete, except children under 16 years of age (since capacity for work was under study) and patients suffering from malignant noncompensated hypertension which can also cause retinal angiopathy. The average age of the patients was 55; their sex structure was as follows: men - 59% (205), women – 41% (143). A proportion between the disabled people with types 1 and 2 of DM was 13% and 87% respectively. In the paper are provided the data on the calculated specific weight of disability, registered as a result of both primary and repeated expert examination in their dynamics, as well as disability frequency with the confidence coefficient t determined (at t≥2, the error probability p<0,05) [16].Herewith, the average annual population in Tashkent was: in 2003 – 2137.3 thous; in 2007– 2168.6 thous; in 2012 – 2325.9 thous. Thus, the average annual population over the period under study amounted to 2269.5 thousand people.
4. Results and Discussion
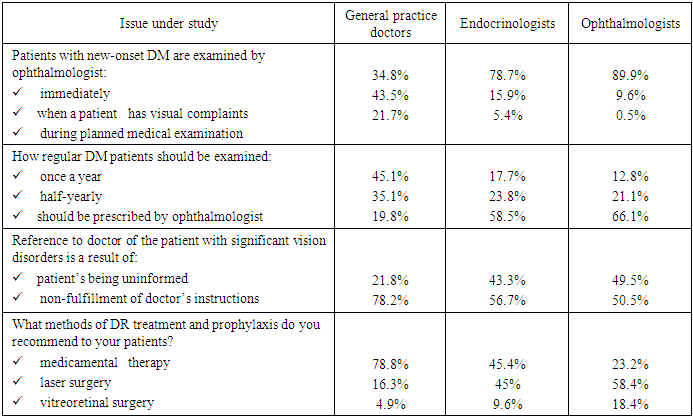
- As results of the questionnaire survey show, almost half of general practice doctors (43.5%) send the patients with new-onset diabetes to ophthalmological examination only if they have visual complaints. While endocrinologists as well as ophthalmologists (78.7% and 89.9% respectively) recommend that ophthalmological examination should be conducted immediately.Similar is the situation with setting the regularity of patients’ examination. In the opinion of the majority of general practice doctors, it is sufficient for a DR patient to undergo examination once a year (45.1%) or half-yearly (35.1%) though its regularity should be determined directly by the ophthalmologist (66.1%) and endocrinologists (58.5%), agree with this.At that, if ophthalmological complications develop in the patient, in the therapists’ opinion, patients themselves are responsible for it (78.2%), since they have not follow doctors’ directions. Yet, endocrinologists and ophthalmologists, who in their majority examine DR patients in proper time, have another view of this problem and think that one of the reasons for DR patients late reference to doctor (almost in half of cases – 49.5%) is unsatisfactory work of primary health care doctors (See Table 1).
|
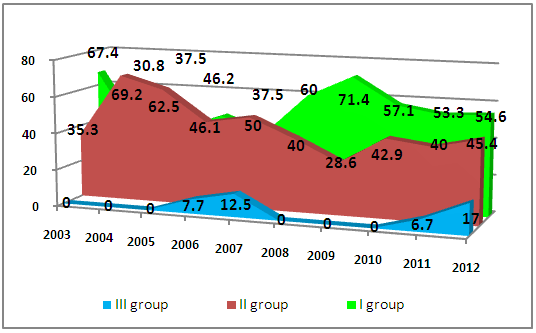 | Figure 1. Distribution of visually impaired persons as a consequence of DM by disability groups among the PRD in Tashkent in 2003-2012 (per 100 thousand people) |
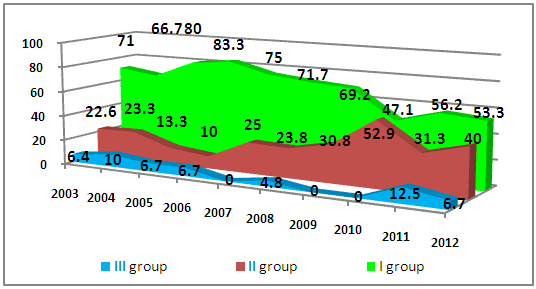 | Figure 2. Distribution of visually impaired persons as a consequence of DM by disability groups among the RRD in Tashkent in 2003-2012 (per 100 thousand people) |
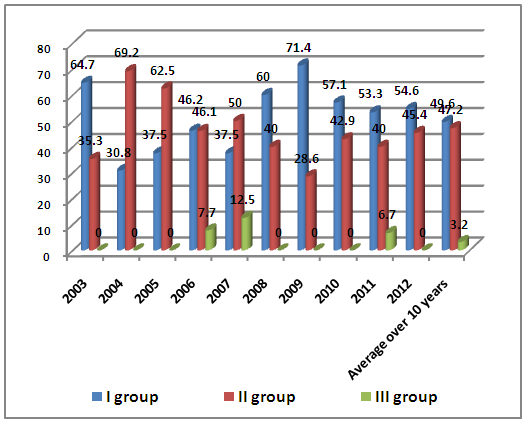 | Figure 3. The structure (specific weight in %) of primary disability caused by ophthalmological complications from DM by disability groups in Tashkent over the 10-year period |
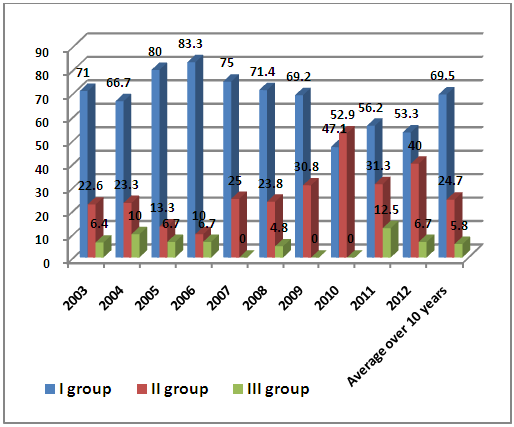 | Figure 4. The structure (specific weight in %) of recurrent disability caused by ophthalmological complications from DM by disability groups in Tashkent over the 10-year period |
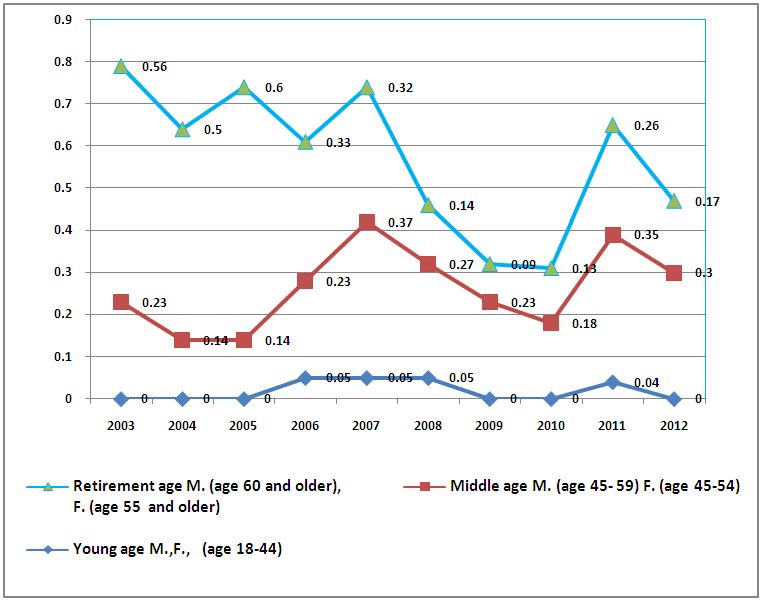 | Figure 5. The level of primary disability caused by ophthalmological complications from DM by age groups in Tashkent within 2003-2012 (per 100 thousand people) |
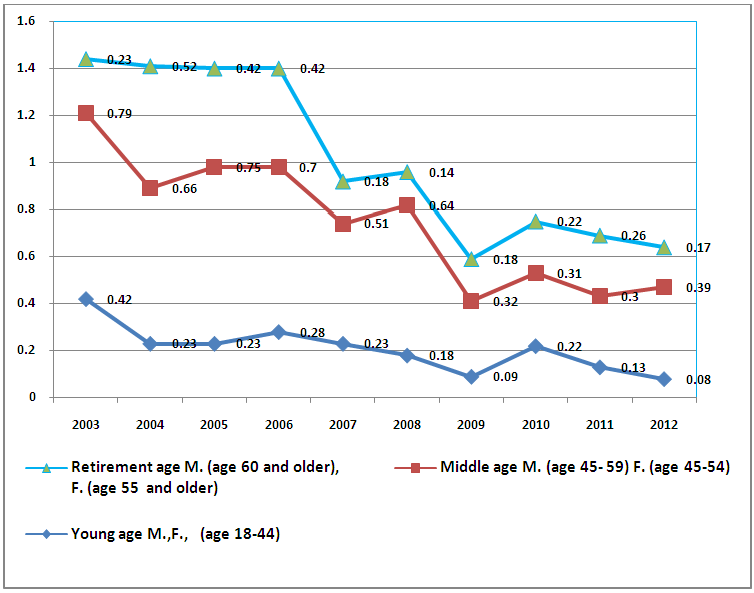 | Figure 6. The level of recurrent disability caused by ophthalmological complications from DM by age groups in Tashkent within 2003-2012 (per 100 thousand people) |
5. Conclusions
- Summarizing the questionnaire survey results as a reserve for further reduction of ophthalmological complications from DM causing disability, the following principal areas should be emphasized:– early referral of all newly diagnosed DM patients for advice of ophthalmologist;– activate explanatory work on the importance of early and regular examination by an ophthalmologist among the DM patients;– focus attention of general practice doctors and narrowly focused specialists on importance of forehanded diagnostics and treatment of this group of sick people.The following peculiarities of primary and recurrent disability caused by ophthalmological complications from DM in Tashkent:– number of RRD is higher than number of PRD;– disabled persons of group II prevail among the patients suffering from type 1 DM; among the patients suffering from type 2 DM, distribution between disabled persons of groups I and II is nearly the same. It is explained by the fact that type 1 DM is diagnosed at an early age when children are under more tight medical supervision which help to prevent the development of complications and also by the fact that at a young age measures of secondary prophylaxis turn out to be more efficient.– on a whole, the level of disability caused by ophthalmological complications from DM is not high, however, disabled persons of groups I and II prevail among the patients with this diagnose who need greater social support;– persons of middle age, i.e. working-age population, prevail among the disabled that also causes economic damage;– it is necessary to have revised the criteria for identification of disability of patients with ophthalmological complications from DM at the stage when it is still possible to adjust a disabling factor and restore working ability.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML