-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2016; 6(6): 171-175
doi:10.5923/j.ajmms.20160606.02

Minimally Invasive Interventions in Surgery of Perforated Duodenal Ulcers
Sh. I. Karimov, M. Sh. Khakimov, Sh. E. Ashurov
Department of Faculty and Hospital Surgery, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Sh. I. Karimov, Department of Faculty and Hospital Surgery, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: To improve the results of surgical treatment of patients with perforated duodenal ulcers by a substantiation of indications for laparoscopic and traditional surgical intervention. Material and Methods: The analysis of results of treatment of 212 patients with perforated duodenal ulcer, complicated by diffuse peritonitis, who were hospitalized in the emergency surgery department of 2 - clinic of the Tashkent Medical Academy for the past 8 years. All patients were divided into three clinical groups. Results: 120 patients of first group with perforated ulcer suturing performed by laparotomy access; second A group - 55 patients operation carried out through a mini-access under video-control; second B group - 37 patients underwent laparoscopic suturing of perforated ulcer. Patients who were executed on the testimony of draining the stomach surgery and vagotomy with antrumectomy gastrectomy, in this study are not included. Complications in all groups were largely associated with traumatic laparotomy access: in the first group in 18 (16.1%) patients, of whom 11 (9.2%) were observed wound complications; and in the second A group in 2 (3.6%) patients in the second B group 1 (2.7%) patients had complications such as surgical wound seroma, early adhesive intestinal obstruction and intestinal paresis. Conclusion: Today, in the presence of the indications for suturing perforated ulcers and ulcer healing predicted the substrate, the optimal methods are minimally invasive surgery with the conduct of a comprehensive anti-ulcer therapy in the postoperative period.
Keywords: Peptic ulcer, Perforation, Laparoscopic suturing
Cite this paper: Sh. I. Karimov, M. Sh. Khakimov, Sh. E. Ashurov, Minimally Invasive Interventions in Surgery of Perforated Duodenal Ulcers, American Journal of Medicine and Medical Sciences, Vol. 6 No. 6, 2016, pp. 171-175. doi: 10.5923/j.ajmms.20160606.02.
1. Introduction
- One of the serious complications of duodenal ulcer (DU) is a perforation, which occupies the first place among the causes of deaths of this disease. According to the Institute of Health and Medical Statistics of the Ministry of Health of the Republic of Uzbekistan and the overall performance of the primary ulcer incidence it declined significantly in recent years. However, currently, the downward trend is not observed frequency of complications. For example, if there is bleeding ulcer in 24.5% cases, the perforation occur in approximately 10% of cases. In 2013, Uzbekistan produced nearly 2,000 emergency operations in patients with perforated gastroduodenal ulcers. This figure in 2014 at above 900 operations than in 2013 [1, 2].However, it has many complications such as suppuration of postoperative wounds, adhesive disease of the abdominal cavity, the formation of ventral hernias, ligature fistulas, etc. The downside suturing perforated ulcer is the high recurrence rate of peptic ulcer disease, reaching up to 50% [5, 6, 12-15]. Therefore, this surgery as a palliative operation has no effect on ulcer etiopathogenesis, indicated for diffuse peritonitis in patients with elderly with serious underlying medical conditions.Currently, due to the emergence of a new generation of drugs with proven ability to significantly accelerate the healing process of gastric ulcer and duodenal defect and to prevent its recurrence, opened up prospects for improving long-term results of treatment of pyloroduodenal perforated ulcer after suturing in young patients [3, 4, 12, 14, 15]. The rapid development of minimally invasive surgery, such as laparoscopic surgery, significantly reduced surgical aggression, mortality and postoperative complications, thereby improving the quality of life of patients in the postoperative period. In this context, it is of particular interest to study the long-term outcomes after laparoscopic duodenal ulcer perforation in the comparative aspect with the traditional method.Objective: to improve the results of surgical treatment of patients with perforated duodenal ulcers by a substantiation of indications for laparoscopic and traditional surgical intervention.
2. Material and Methods
- We conducted an analysis of the results of treatment 212 patients with perforated duodenal ulcer, complicated by diffuse peritonitis, who were hospitalized in the emergency surgery department of 2 - clinic of the Tashkent Medical Academy for the past 8 years. The men were 158 (74.5%), women - 54 (25.5%). The age of patients ranged from 17 to 86 years, with an average of 36,7 ± 8,4 years. Most (84.9%) were persons young and middle age. In the first 12 hours after perforation received 134 (63.2%) patients, from 12 to 24 hours - 57 (26.8%) and days later - 21 (9.9%) patient.The diagnosis of perforated gastroduodenal ulcer established on the basis of a common integrated diagnostic program. From special methods of investigation, besides abdominal radiography, in 41 (19.3%) cases used EGDFS, and in difficult diagnostic situations - laparoscopy (in second groups).In 105 (49.5%) patients ulcer history was absent, in 55 (25.9%) - no more than five years. In 137 (64.6%) cases the ulcer was located on the front wall of the duodenal bulb, 50 (23.5%) - on the front-top and in 25 (11.8%) - on the upper wall. All patients were operated on during the first hour after admission to the hospital.All patients were divided into three clinical groups: first group - 120 patients (laparotomy access (Figure 1) performed suturing perforated ulcer); second A group - 55 patients (operation performed by mini-access under videoassisting control (Figure 2).); second B group - 37 patients (laparoscopic suturing of perforated ulcer (Figure 3).). Patients who were executed on the testimony of draining the stomach surgery and vagotomy with antrumectomy gastrectomy, in this study are not included.
 | Figure 1. Diagnostic error. The scar after appendectomy and midline laparotomy with perforated ulcer duodenum. Perforation was revealed during an appendectomy |
 | Figure 2. Access after video-assisted suturing perforated ulcer |
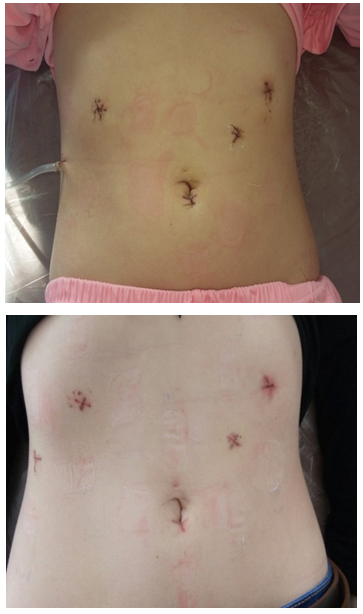 | Figure 3. Area of punctures on the anterior abdominal wall during laparoscopic suturing perforated ulcer (2 and 10 days after surgery) |
3. Results
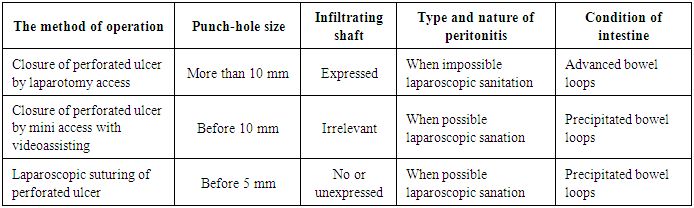
- In most cases, the clinical diagnosis of perforated gastroduodenal ulcer not represent special difficulties. The most authentic and typical signs of the onset of perforation were: sudden onset of acute "dagger" pain in the stomach, followed by the rapid spread of the entire stomach (84.9%), strongest muscle tension of anterior abdominal wall (79.7%), general condition of the patient due to heavy pain shock and intoxication (9.4%).Errors in diagnosis occurred more often in the pre-hospital as a result of an atypical clinical course of perforation (19 cases). In 7 patients were initially diagnosed acute appendicitis, in 10 - acute pancreatitis, in 2 - an exacerbation of peptic ulcer disease. In hospital under dynamic observation perforated ulcer diagnosis was established in 10 of 19 patients using preoperative endoscopy. In 7 patients the true pathology found only during surgery for acute appendicitis. The remaining 2 patients admitted repeatedly from therapeutic department with symptoms of peritonitis. In our opinion, the holding of an emergency EGDFS indicated in all patients with a suspected perforated duodenal and gastric ulcers.In the first group for all patients operations were performed laparotomy access. In the second groups surgery began with a diagnostic laparoscopy and evaluated the ability to perform minimally invasive surgery method. Patients who have shown suturing perforated ulcer laparotomy access is not included in the analyzed material. During diagnostic laparoscopy determined the size of the perforated holes, evaluated the severity of infiltrative shaft, the state of the intestine, the type and nature of peritonitis. Depending on the nature of the pathological process in the abdominal cavity was chosen method of surgical treatment of perforated duodenal ulcer (Table 1).
|
4. Conclusions
- 1. Laparoscopic suturing advisable to perform at the perforation of duodenal ulcers with perforated hole till 5 mm and unexpressed infiltrative shaft. Contraindications to laparoscopic suturing is repeated punching, combination of perforated ulcer bleeding, scar-ulcerative stenosis, size perforated holes larger than 10 mm, the presence of indications for all-out intubation of the small intestine, the impossibility of rehabilitation abdominal laparoscopic way.2. Closure of perforated ulcer through the mini-access using videoassisting should be performed at the perforated hole 10 mm with a pronounced perifocal infiltrate.3. Closure of perforated ulcers is a palliative method of operation, but in the presence of the indications for suturing perforated ulcers and ulcer healing predicted the substrate, the optimal methods are minimally invasive surgery with the conduct of a comprehensive anti-ulcer therapy in the postoperative period.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML