-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2016; 6(4): 129-133
doi:10.5923/j.ajmms.20160604.02

Breast Filariasis on Digital Mammography: Experience from an Endemic Region
Aduayi Olufunso S.1, Akanbi Ganiyu O.1, Aduayi Victor A.2
1Department of Radiology, College of Medicine, Ekiti State University, Ado-Ekiti, Nigeria
2Department of Epidemiology and Community Health, College of Medicine, Ekiti State University, Ado-Ekiti, Nigeria
Correspondence to: Aduayi Olufunso S., Department of Radiology, College of Medicine, Ekiti State University, Ado-Ekiti, Nigeria.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: calcifications of parasitic aetiology are uncommon benign findings on mammograms. Such calcifications are often due to lymphatic filariasis which is endemic in sub-Saharan Africa. This study describes the characteristic features of parasitic calcifications seen on digital mammograms at a tertiary health facility in south-western Nigeria.Materials and Methods: a 2 year prospective cross sectional descriptive study was carried out at the Radiology department of the hospital. Mammographic images were obtained on standard Mediolateral oblique (MLO) and Craniocaudal (CC) views with additional views when indicated. Images were reviewed by two Radiologists and those with parasitic calcifications were further evaluated for appearance, number, distribution and associated findings. A final Breast Imaging Reporting and Data System (BI-RADS) category was assigned according to overall findings. Results: a total of 331 mammograms were done between January 2014 and December 2015, out of which 33 had parasitic calcifications. The age range of the patients with parasitic calcifications was 37-79 years with a mean age of 55±10 years. Breast lumps (n=15, 45.5%) accounted for the highest number of clinical indications for mammography. The parasitic calcifications were coiled and serpiginous in appearance, majorly located within the breast parenchyma and found more in the left breast (n=14, 42.4%). Majority of the mammograms had solitary parasitic calcifications (n=17, 51.6%). Conclusions: breast filariasis may be a source of diagnostic pitfall; hence Radiologists need to be conversant with such mammographic rarities in an endemic region.
Keywords: Mammography, Parasitic calcifications, Breast, Lymphatic filariasis
Cite this paper: Aduayi Olufunso S., Akanbi Ganiyu O., Aduayi Victor A., Breast Filariasis on Digital Mammography: Experience from an Endemic Region, American Journal of Medicine and Medical Sciences, Vol. 6 No. 4, 2016, pp. 129-133. doi: 10.5923/j.ajmms.20160604.02.
1. Introduction
- Parasitic diseases are among the important causes of morbidity and mortality worldwide. In sub-Saharan Africa, a poor socioeconomic status, ignorance, cultural practices and beliefs, poor sanitary conditions together with the climate, provide a conducive environment for parasitic diseases to thrive. Parasitic calcifications are benign and uncommon findings on mammograms and lymphatic filariasis is often the cause. Lymphatic filariasis is a major public health problem affecting an estimated 120 million people worldwide [1]. In Africa, 34 countries are endemic, and Nigeria is believed to bear the highest burden of lymphatic filariasis, with an estimated 80 to 120 million people at risk. [2, 3] The causative organisms are roundworms of the Filarioidea type spread by blood-feeding black flies and mosquitoes. Wuchereria bancrofti accounts for more than 90% of the cases in the world and is transmitted throughout the tropics in Africa, Asia, the Pacific and the Americas while Brugia malayi and Brugia timori are found in east and south Asia [2, 4]. These worms occupy the lymphatic system, including the lymph nodes. Subcutaneous filariasis is caused by Loa loa (the eye worm), Mansonella streptocerca, and Onchocerca volvulus. These worms occupy the subcutaneous layer of the skin. Loa loa filariasis is also known as Calabar Swelling [5, 6] (named after a city of high endemicity in Southern Nigeria). Lymphatic filariasis has a predilection for lower limbs, retroperitoneal tissues, spermatic cord, and epididymis and presents as lymphedema, elephantiasis, and hydrocele. Involvement of the breast is uncommon [7, 8] Mammographic calcifications of parasitic origin may constitute a diagnostic pitfall and result in unwarranted invasive breast procedures in some instances. This study reports on 33 digital mammograms with calcifications of parasitic origin encountered within a 2 year period at a tertiary health facility situated in a country endemic for lymphatic filariasis.
2. Materials and Methods
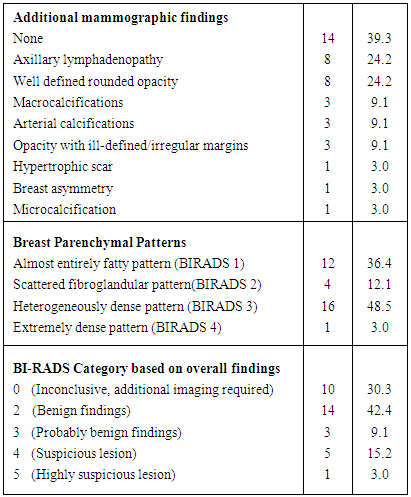
- A prospective cross sectional descriptive study was conducted at Ekiti State University Teaching Hospital in Ado-Ekiti, South-western Nigeria between January 2014 and December 2015. The study population consisted of consecutive patients who presented for mammography at the radiology department during the study period. The basic information on the mammography request cards filled by the referring doctor included the patient’s age, last menstrual period and clinical indication for the study. The clinical indication was either screening mammography for patients without presenting complaints or diagnostic mammography for patients with various breast-related complaints. Approval was granted by the institution’s Ethical clearance Committee. A digital mammogram machine (GE Medical Systems Societe Digital Mammogram machine Model 5145113; France) was utilized. The mammographic images were obtained on standard Mediolateral oblique (MLO) and Craniocaudal (CC) views as well as additional views when indicated. The mammograms were reviewed by two Radiologists for comprehensive evaluation of imaging findings. Mammograms that showed parasitic calcifications had the location, appearance, number and distribution of the calcifications. Other mammographic findings seen on the images apart from parasitic calcifications were taken into consideration before assigning a final BIRADS Category for each mammogram report.Mammographic breast parenchymal density pattern were classified using the BIRADS categories for breast parenchymal density. The breast density classifications are as follows: BIRADS 1: Almost entirely fatty pattern; BIRADS 2: Scattered fibroglandular pattern;BIRADS 3: Heterogeneous dense pattern; BIRADS 4: Extremely dense pattern. The overall mammographic findings were categorized using the American College of Radiology (ACR) guidelines. The assessment categories of mammographic findings are as follows: BIRADS 0: Inconclusive study (additional imaging required); BIRADS 1: Normal study; BIRADS 2: Benign findings; BIRADS 3: Probably benign findings; BIRADS 4: Suspicious lesion; BIRADS 5: Highly suspicious lesion; BIRADS 6: Biopsy proven malignancy.Patients that required additional imaging had breast ultrasonography done. The data was entered into a spread sheet and analysed using Statistical Package for Social Sciences (SPSS) version 20, Chicago USA Inc.
3. Results
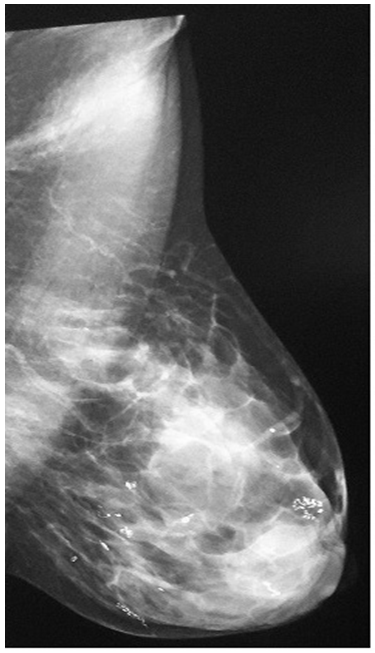
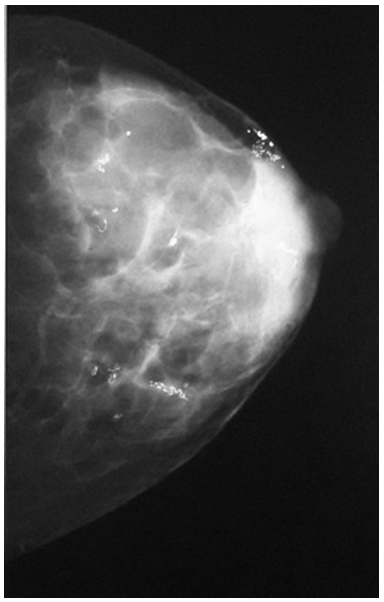
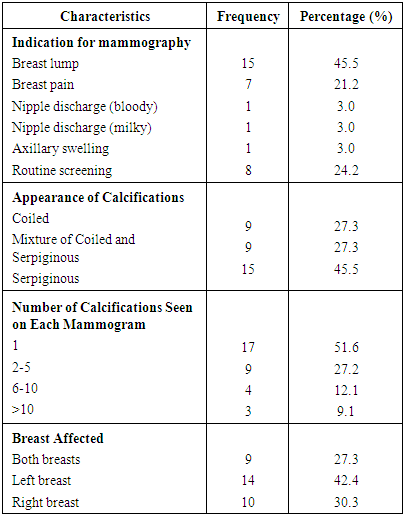
- Out of the 331 mammograms done between January 2014 and December 2015, 33 had parasitic calcifications. The age range of the patients was 37-79 years with a mean age of 55±10 years. One out of the 33 patients was a male (3%) while the remaining 32 (97%) were females. All the females were from Yoruba ethnic group in south western Nigeria while the male was from the Ibo ethnic group of south eastern Nigeria. All the subjects were domiciled in Ekiti state. The clinical indications for mammography showed that 8(24.2%) presented for routine mammographic screening for breast cancer while the remaining 25(75.8%) presented for diagnostic mammographic evaluation based on various breast complaints, the most common of which was breast lump. The most commonly affected breast was the left breast (n=14, 42.4%). Majority of the mammograms had solitary parasitic calcifications (n=17, 51.6%) (Table 1). In terms of location, within the breast tissues, right lower quadrant parasitic calcifications were the most common (Figure 1). The parasites appeared as coiled and serpiginous microcalcifications majorly located within the breast parenchyma (Figure 2 and 3).
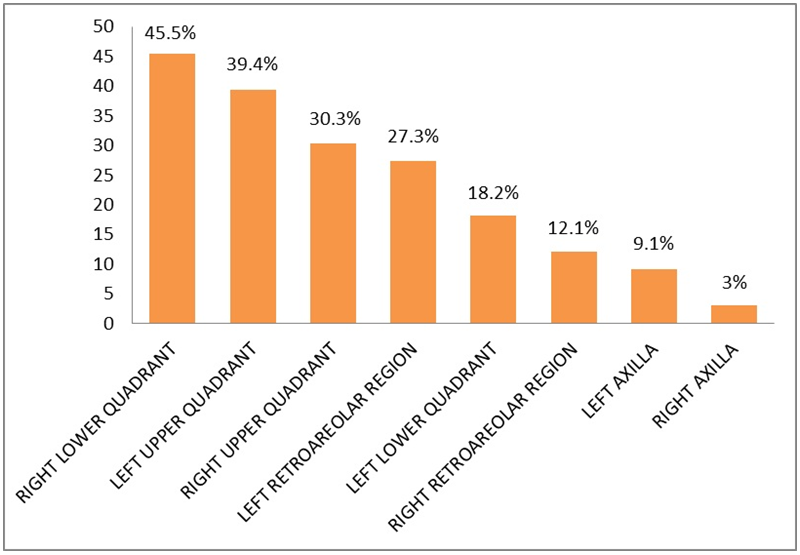 | Figure 1. Location of mammographic parasitic calcifications |
|
|
4. Discussion and Conclusions
- Filariasis is an endemic disease in sub-Saharan Africa which uncommonly manifests in the breast tissues. In this study 33 (10%) patients out of 331 who presented for mammography within a 2 year period had parasitic calcifications. In a study conducted by Adeniji –Sofoluwe et al [9] in Ibadan, south western Nigeria 39(7.4%) patients out of 527 who had mammography done within a period of 6years had parasitic calcifications. Hence the proportion of reported cases of mammographic parasitic calcifications is higher in Ado-Ekiti. A greater proportion of the patients with parasitic calcifications in our study presented for diagnostic mammography (75.8%) with the most common complaints of breast lump while majority of patients in the Ibadan study presented for screening mammography (79.5%). Mammography for screening and diagnostic breast imaging is utilized more by the female gender hence it is expected that cases of mammographic parasitic calcifications will be predominantly reported among women. The only male involved in this study had to undergo diagnostic mammography on account of suspected breast cancer. A suspicious breast mass was seen while the parasitic calcification was an additional finding in his left axilla.This study revealed that a greater proportion of mammographic parasitic calcifications were discovered in the left breast. Also, filarial calcifications can be found anywhere in the breast including the nipple and retroareolar region [9, 10].For breast filariasis to occur, the larvae of the filarial worms enter the lymphatic vessels of the mammary gland, causing lymphangitis, fibrosis, and disruption of lymphatic drainage. [11] Some patients infected with these parasites may present with a unilateral painless solitary lump. The upper outer quadrant of the breast is the most common site of involvement. [12, 13] Acutely, filarial infection of the breast can present with an erythematous painful lump, there may be associated axillary lymphadenopathy with induration and hyperpigmentation of overlying skin all these features are a cause for concern as it may raise a clinical suspicion of a mitotic breast lesion. [8] Suspicious skin and axillary changes are known features of breast cancer and could lead to misdiagnosis in our environment where mammographic breast imaging is in its infancy. [9] More so in a developing country that lacks full complement of further comprehensive breast work up with Magnetic Resonance Imaging (MRI), stereotactic biopsy and needle localization. [9]Digital mammography offers better imaging resolution and diagnostic accuracy [14] compared to analogue (film screen mammography) which is more readily available in resource poor settings. With digital mammography, the radiologists can adjust the image contrast, brightness and magnification for optimized image viewing and reporting directly from the monitor. This was to an advantage in this study. In late inactive phases, calcified filarial worms characteristically appear as serpiginous, tubular calcifications without signs of irregularity or pleiomorphism on mammographic images [10, 15]. The adult form of W. bancrofti resides in the lymphatics, death of the worm with accompanied regional inflammation and necrosis results in filarial calcifications taking the form of the worm. This study shows that in some instances, foci of calcification of worms may be seen, appearing as short coiled calcifications suggestive of smaller fragments of the worm while calcifications of whole worms appear longer and serpiginous. In the heavily infested breast tissues, a combination of both coiled and serpiginous calcifications may be seen (figure 2 and 3). These calcifications are typically present and mammographically stable for many years. If seen on a baseline mammogram, the characteristic morphology and appropriate clinical history are the most helpful factors in diagnosing filarial calcifications. [15] The filarial infection, caused by W bancrofti, has mammographic features different from the nematodal infections caused by Onchocerca volvulus (onchocerciasis), Loa loa (loiasis), and Trichinella spiralis (trichinosis) [16] and can be differentiated based on location and appearance. The O volvulus organisms are often found in spaces just beneath the skin epithelium and, occasionally, in lymphatic vessels and lymph nodes. They are often distinguishable because their calcifications form intricate tangles [10]. The calcifications of loiasis can be distinguished from those of W bancrofti on the basis of their appearance as either short or long continuous or beaded fine calcifications when the worm is extended. Loiasis may also appear as hair like whorls of calcifications. Trichinosis calcifications are located only in the pectoral muscles [17, 18], whereas those of filariasis are located primarily in the breast parenchyma. Trichinosis calcifications are much smaller, more numerous, and not serpiginous when compared with those of filariasis. [10, 18] On real time ultrasound movement of adult filarial worms in a characteristic wriggly manner can be observed and this is described as “filarial dance”. [13, 19] However among the subjects that had additional sonographic evaluation in this study, the filarial dance was not classically demonstrated on real time ultrasonography, further indicating that the parasites were already in the inactive calcified states. Differential diagnosis of calcified microfilaria includes vascular calcifications, ductal calcifications, dystrophic calcifications and artifact. Orientation of parasitic calcifications is not different from typical ductal distribution radiating out from the nipple. Vascular calcifications show a distinctive tram-track (railroad track) configuration paralleling the vessel wall. [15] Benign dystrophic calcifications can also be differentiated from those of parasitic diseases on the basis of their coarse, dense, irregular appearance [10].Laboratory diagnosis of filariasis is made by detection of microfilariae in the peripheral blood film, however it has also been documented that in endemic areas filariasis can exist without microfilaremia [20]. The coexistence of peripheral blood eosinophilia with microfilariae as also been reported. Additional tests include antifilarial antibodies for circulating parasite antigens, polymerase chain reaction and Fine needle aspiration cytology (FNAC) which is particularly useful in patients with mass lesions. [20] The parasitic calcifications reported in this study were incidental findings of dead calcified inactive worms hence additional extensive laboratory work up or invasive procedures were not necessary for confirmation. In the acute presentations with live parasites, patients often show marked clinical response to anthelminthic therapy within few weeks of administration.[1] Filarial breast calcifications appear to represent chronic sequela of infection, presenting months to years after exposure. Therefore, it is important to consider this diagnosis not only among people living in or emigrating from endemic areas but also in those who have travelled to or visited these areas at any time. [15] Even in non-endemic regions, despite the current global campaign to eliminate filariasis, the appearance of filarial infection on mammography is likely to be observed more frequently, because immigrants from areas where filariasis is endemic are settling in increasing numbers in developed countries. [11] In conclusion, Nigeria is one of the countries in the world with a high prevalence of lymphatic filariasis and this uncommonly manifests in the breast tissues as mammographic calcifications. Radiologists need to be conversant with characteristics of such mammographic parasitic calcifications in order to avoid misdiagnosis.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML