-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2016; 6(3): 95-97
doi:10.5923/j.ajmms.20160603.06

Individual Adjustment of the dose of Local Anesthetic for Spinal Anesthesia in Pregnant Women with Increased Body Mass Index
M. M. Matlubov
Samarkand State Medical Institute, Samarkand, JSC Republic Scientific Research Medical Center of Obstetrics and Gynecology, Tashkent, Uzbekistan
Correspondence to: M. M. Matlubov, Samarkand State Medical Institute, Samarkand, JSC Republic Scientific Research Medical Center of Obstetrics and Gynecology, Tashkent, Uzbekistan.
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of investigation was the assessment of hemodynamic status in response to subarachnoid injection of 0,5% hyperbaric solution of bupivakaine the individual dosage of which we have been calculated on the kilogram of body mass (1 group) and according to the morphometric indexes (height, body mass index, excess of body mass index) (2 group). 48 pregnant women at the age from 23 to 36 years old by gestation period of 36-39 weeks with body mass index of 25-34,9 kg/m2, with preserved adaptive possibilities of cardio-vascular system and delivered by abdominal method have been included in the investigation groups. It has been established that individual adjustment of the dose of local anesthetics for spinal anesthesia on the basis of morphometric indexes have been supplied high effective anesthesia and hemodynamic stability. Calculation of the dose due to body mass (0,2-0,15 mg/kg) is accompanied by significant hemodynamic disorders and as a result it is not reasonable for patients with high body mass index.
Keywords: Pregnancy, Overweight, Body mass index, Obesity, Spinal anesthesia, Hemodynamic, Abdominal delivery
Cite this paper: M. M. Matlubov, Individual Adjustment of the dose of Local Anesthetic for Spinal Anesthesia in Pregnant Women with Increased Body Mass Index, American Journal of Medicine and Medical Sciences, Vol. 6 No. 3, 2016, pp. 95-97. doi: 10.5923/j.ajmms.20160603.06.
Article Outline
1. Introduction
- For the present stage of the development of modern anesthesiology method of choice of anesthesia during abdominal delivery according to the absolutely most clinicians is spinal anesthesia (SA) [4, 5, 7]. Method is simple and high effective, allows us with minimal risk to carry out emergency surgical operations in patients with “full stomach”, to admit the presence of mother in the process of delivery, reduces risk of hypoxia and postanesthesia depression of the fetus. However the use of it in the patients with high body mass index (obesity) could be accompanied by significant hemodynamic disorders stipulated with the one side by high segmental sympathetic blockades and with the other by reducing adaptative possibilities from cardio-vascular system. At the same time the use of SA in patients with increased body mass index (BMI) during abdominal delivery has a number of features one of them is that fact during increasing body mass it is happened reducing the volume of subarachnoid cavity at the expense of increasing intra-abdominal pressure and extension of the volume of epidural cavity [4, 5]. In connection with it the use of standard dose of local anesthetics inevitably leads to high cranial distribution of the last ones with the development high segmental sympathetic blockage and arterial hypotension [1, 5].For the present time a number of appropriate protocols on individual selection of the dose of local anesthetics f local anesthetics or SA according to the height [3, 6] and also complex of morphometric indexes (height, BMI, excess of BMI) [1] well recommended themselves in the practical work have been existed. At the same time, as usual the recommendations on calculation of individual dose of local anesthetics (LA) only according to body mass have been taken place [2, 3, 5, 7].
2. Aim of Investigation
- Comparative assessment of hemodynamic indexes in response to subarachnoid injection of standard doses of local anesthetics calculated on the basis of body mass and doses of local anesthetics which calculated with taking into account individual morphometric characteristics in patients increased body mass index (BMI) and obesity.
3. Materials and Methods of Investigation
- 48 pregnant women at the age from 23 to 36 years old in the gestation periods of 36-39 weeks with high BMI and obesity (25-34,9 kg/m2) with saved adaptation abilities of cardio-vascular system under SA of 0,5% hyperbaric solution of bupivacaine in the systematic order have been carried out abdominal delivery. The excluding criterion from investigation was the presence of development factors of hypo- and hypertension in pregnant women. Surgical operations have been performed in the systematic order and duration of them was 25-40 minutes. Depending on the calculation method of the dose of subarachnoid injected bupivacaine all our investigated patients were divided into 2 groups. All patients were compared by anthropometric characteristics, degree of anesthetic risk and by the character of surgical intervention. Protocol of anesthetic manual in the both groups of patients with overweight and obesity was identical except dosing methods of local anesthetic. The level of subarachnoid puncture was in line with L2-L4. 19 women have been included in the 1-st group whom we subarachnoid injected 0,2-0,15 mg/kg or 2,5-3,2 ml of bupivacaine, 29 patients have been included in the 2-d group whom we subarachnoid injected 9,0-11,0 mg or 1,8-2,2 ml of bupivacaine. The dose of the local anesthetic we calculated on the basis of morphometric characteristics (height, BMI, excess of BMI) [1, 6], according to formula;
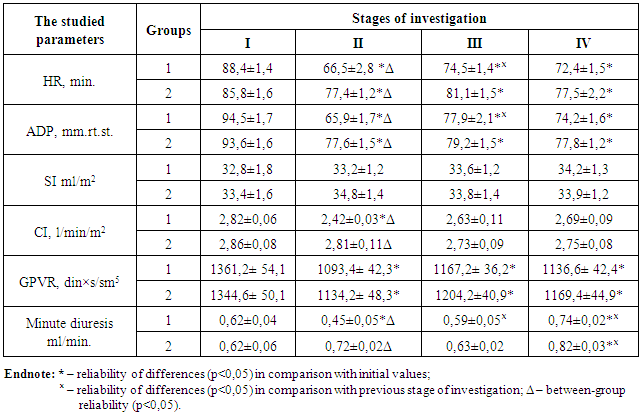
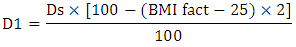 Where: D1 – Individual dose of local anesthetic calculated on height with correction to body mass:Ds – Standard dose of local anesthetic calculated on height: BMI fact – Real value of body mass index (for the concrete patient). In the both investigated groups premedication was included dimedrol 0,2 mg/kg and dexametazone 0,07 mg/kg which have been injected intravenous. With the appearance of the clear clinic signs of segmental sensor-motor blockade patients were imparted “left-uterine position” and the head fragment of operational table has been raised on 10-15° (Fovler’s position). After extraction of infant from uterus with the aim of decreasing psycho-emotional stress it has been injected valium intravenously (0,2 mg/kg). About the effectiveness of anesthesia we have been judged according to the generally accepted clinical signs. The level of sensor block has been assessed due to loss of pain sensitivity (pinprick test). The upper border of blockade has been assessed after its stabilization. The depth of motor blockade has been assessed with the use of P. Bromage scale. Central hemodynamic was studied by method of echocardiography with the use of Mindray apparatus. Strong index (SI), cardiac index (CI) and general peripheral vascular resistance (GPVR) have been studied. The average dynamic pressure (ADP), heart rate (HR) and saturation of hemoglobin (SpO2) have been controlled with the use of Schiller monitor. Minute diuresis also was studied. Investigation has been carried out in 4 stages: 1 – on the operational table; 2 – before skin incision; 3 – in the most traumatic stage of surgical operation (extraction of infant from uterus, operative exploration of abdominal cavity); 4 – after the end of surgical operation. All numerical values received during investigation have been processed by the methods of variation statistics with the use of Student’s criterion (by the use of Microsoft Excel program) and presented by way of M ± m, where M was the value of arithmetic mean and m was the standard error of the arithmetic mean. Statistically reliable values have been considered the differences at p<0,05. The received results have been presented in the table below.
Where: D1 – Individual dose of local anesthetic calculated on height with correction to body mass:Ds – Standard dose of local anesthetic calculated on height: BMI fact – Real value of body mass index (for the concrete patient). In the both investigated groups premedication was included dimedrol 0,2 mg/kg and dexametazone 0,07 mg/kg which have been injected intravenous. With the appearance of the clear clinic signs of segmental sensor-motor blockade patients were imparted “left-uterine position” and the head fragment of operational table has been raised on 10-15° (Fovler’s position). After extraction of infant from uterus with the aim of decreasing psycho-emotional stress it has been injected valium intravenously (0,2 mg/kg). About the effectiveness of anesthesia we have been judged according to the generally accepted clinical signs. The level of sensor block has been assessed due to loss of pain sensitivity (pinprick test). The upper border of blockade has been assessed after its stabilization. The depth of motor blockade has been assessed with the use of P. Bromage scale. Central hemodynamic was studied by method of echocardiography with the use of Mindray apparatus. Strong index (SI), cardiac index (CI) and general peripheral vascular resistance (GPVR) have been studied. The average dynamic pressure (ADP), heart rate (HR) and saturation of hemoglobin (SpO2) have been controlled with the use of Schiller monitor. Minute diuresis also was studied. Investigation has been carried out in 4 stages: 1 – on the operational table; 2 – before skin incision; 3 – in the most traumatic stage of surgical operation (extraction of infant from uterus, operative exploration of abdominal cavity); 4 – after the end of surgical operation. All numerical values received during investigation have been processed by the methods of variation statistics with the use of Student’s criterion (by the use of Microsoft Excel program) and presented by way of M ± m, where M was the value of arithmetic mean and m was the standard error of the arithmetic mean. Statistically reliable values have been considered the differences at p<0,05. The received results have been presented in the table below.
|
4. Results and Discussion
- Characterizing clinical duration of SA of the 1 group (n=19) it should been noted that the classic signs of full segmental sensor-motor blockade were developed in 6-8 minutes with the moment of subarachnoid injection of the calculated dose of local anesthetic and continued during 1,5-2 hours. Besides segmental level of sensor blockade was corresponded to Th4-Th5 dermatomes. In the 2 group of patients (n=29) the full segmental sensor-motor blockade was formed at the same periods, however the distribution of it in thoracic spine was not so significant and reached only to Th6-Th7 dermatomes which supplied quiet adequate anesthesia.Initial state of hemodynamic in the both investigated groups was characterized by moderately expressed tachycardia, reducing one-shot and minute heart productivity, however they were not overrun of their physiological variations. Eukinetic regime of blood supply has been taken place in all investigated women by us (table). Indexes which are indirectly characterized peripheral blood supply (GPVR and minute diuresis) also have been in the framework of their physiological variations (see table). Studying parameters in the both investigated groups were identical and reliably did not differ from each other. Before the skin incision against the background of the full segmental sensor-motor blockade in patients of the both groups (1, 2) classic clinic-functional manifestations of the central segmental blockades – reduction of HR, decreasing of ADP and GPVR (see table) which were reliably more significant in patients of the 1 group have been registered. So ADP and GPVR in patients of the 1 group have been decreased in 30,2% and 19,7% and HR has been reduced in 24,7%. At the same time in women of the 2 group ADP and GPVR have been decreased only in 17% and 16,7%, and HR has been reduced in 9,7%. Besides in patients of the 2 group CI has been left without any reliable difference reflecting adaptive possibilities of cardio-vascular system and in women of the 1 group this index has been reliably decreased until 2,42±0,03 l/min/m2. Accordingly minute diuresis has been changed – in patients of th2 group it has been increased in 16,1% and in women of the 1 group it has been reliably reduced in 27,4%. Restructuring of hemodynamic in the 1 group of women was required immediate vasopressor support and atropinization and also creation of the Fovler’s position with the aim of movement of bupivacaine solution to the caudal direction, intravenous injection of hydroxiethylstarch solutions. In the 2 group of patients vasopressor support, as a ruse, was not required.At the same time it is needed to mention that classic signs of segmental blockade (moderate reduction of ADP, GPVR, reducing HR) have been preserved in the both studied groups until termination of local anesthetic induced action (2-3 hours). Besides in the 1 group of women they as usual were carried more significant character. During all surgical operation in the both investigated groups female patients were remained calm without any complains. Signs of breathing depression we have not been determined, SpO2 was 96-98%. Thus individual selection of the dose of local anesthetic for pregnant women with increased BMI on the basis of morphometric indexes allow us to supply hemodynamic stability during all surgical operation at the same time supplying high quality of SA, however on the assumption of the safety of adaptive possibilities of cardio-vascular system.
5. Conclusions
- 1. Individual selection of the dose of local anesthetics for pregnant women with increased BMI on the basis of morphometric indexes where height, BMI and excess of BMI have been taken into consideration and allow us to provide hemodynamic stability during all surgical operation at the same time supplying a high quality of SA.2. Calculation of the individual dose of local anesthetic for SA on the basis of body mass (0,2-0,15 mg/kg) is accompanied by significant hemodynamic disorders and as a result it is not acceptable for patients with high BMI and obesity.3. The mandatory requirement of using SA during abdominal delivery for pregnant women with high BMI is a safety of adaptive possibilities of their cardio-vascular system.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML