-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2015; 5(5): 201-203
doi:10.5923/j.ajmms.20150505.02
A Study of Fibrinogen Level and C-reactive Protein in Type 1 and Type 2 Diabetes Mellitus and Their Relation to Glycemic Control
Mohammed S. M. Alnour1, Mahdi H. A. Abdalla2
1Department of Haematology, Faculty of Medical Laboratory Sciences, Alneelain University, Sudan
2Department of Haematology, Faculty of Medical Laboratory Sciences, Omdurman Ahlia University, Sudan
Correspondence to: Mahdi H. A. Abdalla, Department of Haematology, Faculty of Medical Laboratory Sciences, Omdurman Ahlia University, Sudan.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
The complications of diabetes mellitus (DM) are predominantly vascular which include the development of retinopathy, nephropathy and increased risk of cardiac, peripheral arterial and cerebrovascular disease. Fibrinogen and C reactive protein (CRP) are identified as a major independent risk factor of cardiovascular disease. This study aimed to determine fibrinogen level and CRP among diabetic patients, and their relations to glycemic control in Sudan. The study included 60 diabetic patients (30 type 1 DM and 30 type 2 DM patients) their fibrinogen level, CRP and haemoglobin (Hb) A1C were measured and compared with 30 normal subjects as control. Fibrinogen level was measured by Clauss modified method. CRP and HbA1C were measured using i-CHROMATM system. 73.3% of DM patients presented with poor glycemic control with Hb A1C greater than 7%. Our study revealed higher fibrinogen level and CRP among diabetic patients than the control, with further increase in the fibrinogen level among type 2 DM patients than type 1 patients. Our study also demonstrated significant correlation between fibrinogen level and CRP, and HbA1C level. In conclusion, our study revealed higher fibrinogen level and CRP among diabetic patients than the control, this finding suggested an increased cardiovascular risk among DM patients; the risk is increased with poor glycemic control.
Keywords: Diabetes Mellitus, Fibrinogen, CRP, HbA1C
Cite this paper: Mohammed S. M. Alnour, Mahdi H. A. Abdalla, A Study of Fibrinogen Level and C-reactive Protein in Type 1 and Type 2 Diabetes Mellitus and Their Relation to Glycemic Control, American Journal of Medicine and Medical Sciences, Vol. 5 No. 5, 2015, pp. 201-203. doi: 10.5923/j.ajmms.20150505.02.
Article Outline
1. Introduction
- Diabetes Mellitus (DM) is a group of metabolic diseases which is characterized by hyperglycemia resulting from defect in insulin secretion, insulin action, or both [1]. in 1985 an estimated 30 million people around the world where diagnosed with diabetes; in 2000 that figure rose to over 150 million, and in 2012 the international diabetes federation estimate 371 million people with diabetes, the number is projected to rise to 552 million by 2030 [2]. The complications of DM are predominantly vascular which include the development of retinopathy, nephropathy and increased risk of cardiac, peripheral arterial and cerebrovascular disease. The major types of diabetes are type 1, type 2 and gestational diabetes (GDM) [3]. Type 1 DM is characterized by destruction of the pancreatic beta cells, leading to absolute insulin deficiency. This is usually due to autoimmune destruction of the beta cells. Although it has long been called “juvenile diabetes” due to the more frequent and relatively straightforward diagnosis in children, the majority of individuals with type 1 diabetes are adults [4]. Type 2 DM results from a progressive insulin secretory defect on the background of insulin resistance. GDM which diagnosed during pregnancy is not clearly overt diabetes [5]. Fibrinogen and C reactive protein (CRP) are identified as a major independent risk factor of cardiovascular disease [6]. They are one of the positive acute phase reactants [7, 8] and both are markers of inflammation which are considered as predictive risk of myocardial infarction, stroke, peripheral arterial disease and sudden cardiac death [9]. Haemoglobin (Hb) A1C is used primarily to identify the average plasma glucose concentration over prolonged period of time (three to four month). Also it can be used as diagnostic test for DM, with a 6.5% cut –off point for diagnosing diabetes. So that Glycosylated hemoglobin in diabetic patients reflects the average blood glucose level, and will not be affected by variability in blood glucose in short time [10]. This study aimed to determine fibrinogen level and CRP among diabetic patients, and their relations to glycemic control in Sudan.
2. Materials and Methods
- Following informed consent ninety subjects were enrolled in this study: Thirty patients with type 1 DM and thirty patients with type 2 DM who attended Ibrahim Malik hospital at Khartoum state, Sudan; and thirty normal, non-diabetic subjects as controls. None of the patients were receiving anticoagulant therapy at the time of the study. Patients with recent surgery, trauma, autoimmune disease or malignancy were excluded from this study. Pregnant women and smokers were also excluded. Five ml of venous blood samples were collected from each subject: 2.5ml was collected in 3.8% tri-sodium citrate (9:1 vol/vol) for fibrinogen analysis. Samples were kept in ice until centrifugation at 2500 g for 30 minutes at 4°C, plasma samples were immediately frozen and stored at -80°C for subsequent analysis; and 2.5 ml in EDTA anticoagulant for CRP and HbA1C. Laboratory analyses were performed at the department of hematology, faculty of medical laboratory science, Alneelain University, Sudan.Fibrinogen level was measured by Clauss modified method using a test kit produced by (TECHOCLONE GMBH, AUTRRIA). The method uses functional assay based upon the time for fibrin clot formation, in brief, diluted plasma is clotted with high concentration of thrombin, and the concentration of fibrinogen is determined by comparing the plasma clotting time to a calibration curve of reference plasma with a series of dilutions (1:5 – 1:40). CRP and HbA1C were measured using i-CHROMATM system (Boditech–Korea). The test uses the sandwich immunodetection method. The antigen (CRP or HbA1C) is bound with an antibody in buffer and the antigen-antibody complexes are captured by antibodies that have been immobilized on the test strip as sample mixture migrates through nitrocellulose matrix. Signal intensity of fluorescence on detection antibody reflects the amount of the antigen captured and is processed by iCHROMATM Reader to show the concentration in the specimen. Statistical analysis was performed using statistical package for social science (SPSS) software. Evaluation of patient’s data was performed using the t-test. Results with p value < 0.05 were considered statistically significant.
3. Results
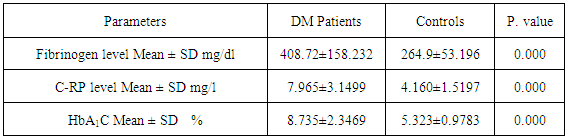
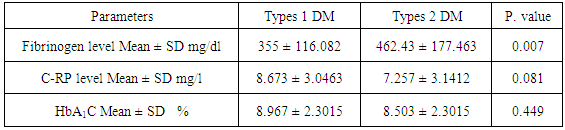
- The study included 30 type 1 DM patients their male: female ratio was 1.5, mean age was 5.77±25 Years, and mean disease duration was 8.26±3.97 Years; and 30 type 2 DM patients their male: female ratio was 1.5, mean age was 52±7.01 Years, and mean disease duration was 10±5.76 Years. 73.3% of DM patients presented with poor glycemic control with Hb A1C greater than 7%.Table 1 showed the results of fibrinogen, CRP, and HbA1C among DM patients and controls.
|
|
4. Discussion
- It is well known that Atherosclerotic vascular complication is a common cause of morbidity and mortality in DM patients [11]. The current study was conducted in Khartoum state among diabetic patients with type 1DM and type 2 DM. We examined the association of fibrinogen level and CRP, as a risk modifier for cardiovascular complication in diabetic patients, with the average plasma glucose concentration, determined by HbA1C. The study included 60 diabetic patients (30 type 1DM and 30 type 2 MB patients) their fibrinogen level and CRP were measured and compared with 30 normal subjects as control. Most of patients had poor glycemic control (73.3%); this frequency was higher compared to previous reports among different populations [12-14]. This result highlighted the urgent needs to develop an awareness plan as to reduce the incidence of diabetes complications in future. Our study revealed higher fibrinogen level and CRP among diabetic patients than the control. Similar findings were previously reported [14-18]. Fibrinogen and CRP are identified as a major independent risk factor for cardiovascular disease. Our finding suggested an increased cardiovascular risk in such patients. Fibrinogen was significantly higher among type 2 DM than type 1. Ljubic et al reported a significant increase in fibrinogen level as well as CRP in their study population [19], our finding suggested that type2 DM is more inflammatory and patients with type 2 DM are at higher risk of cardiovascular complication than type 1 DM patients. Our study observed a significant correlation between fibrinogen level and CRP, and HbA1C level. Similar finding was reported in previous study [18]. This finding highlighted that the risk of cardiovascular complication is further increased in diabetic patients with poor glycemic control.
5. Conclusions
- Our study revealed higher fibrinogen level and CRP among diabetic patients than the control. Fibrinogen level was further increased among type 2 DM patients than type 1 DM patients. A significant correlation was observed between fibrinogen level and CRP, and HbA1C level. Our finding suggesting an increased cardiovascular risk among DM patients, the risk is increased with poor glycemic control.
ACKNOWLEDGEMENTS
- Special thanks to the Staff of Haematology Department, Faculty of Medical Laboratory Sciences, Alneelain University.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML