-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2015; 5(5): 191-200
doi:10.5923/j.ajmms.20150505.01
Mindfulness - Based Cognitive Therapy; - Impact on Depressed Outpatients of the State Hospital Oyo State Ibadan, Nigeria
Afusat Olanike Busari
PhD, Department of Guidance & Counselling, Faculty of Education, University of Ibadan, Nigeria
Correspondence to: Afusat Olanike Busari, PhD, Department of Guidance & Counselling, Faculty of Education, University of Ibadan, Nigeria.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
This study investigates the impact of Mindfulness–Based Cognitive Therapy (MBCT) on depressed outpatients of the state Hospital in Oyo state Ibadan, Nigeria. The sample comprised of 32 men and women 18 years and above. The instrument used for screening was Beck Scale for Suicide Ideation (BSS) while Beck Depression Inventory–II (BDI–II) was used for data collection. The research design adopted for this study was Pre-Post experimental design. Four research hypotheses were formulated and tested at 0.05 level of significant. Analysis of covariance (ANCOVA) was the statistical tool employed for processing the data collected. Depressive symptoms and diagnostic status were assessed before and after the treatment phase. Self-reported symptoms of depression decreased from severe to mild levels in MBCT group while no significant decrease was recorded in the control group. This study provides further evidence that MBCT can be used successfully to reduce Symptoms of depression among the sufferer.
Keywords: Mindfulness, Cognitive Therapy, Impact, Depressed Outpatients
Cite this paper: Afusat Olanike Busari, Mindfulness - Based Cognitive Therapy; - Impact on Depressed Outpatients of the State Hospital Oyo State Ibadan, Nigeria, American Journal of Medicine and Medical Sciences, Vol. 5 No. 5, 2015, pp. 191-200. doi: 10.5923/j.ajmms.20150505.01.
Article Outline
1. Introduction
- Depression is a state of low mood and aversion to activity that can affect a person’s thoughts, behavior, feelings and sense of well-being, (Jonathan Hill 2014). Depressed people can feel sad, anxious, empty, hopeless, worried, worthless, guilty, irritable, hurt or restless (EhretM & Sobieray 2014). They may lose interest in activities that once were pleasurable, experience loss of appetite or over-eating, have problems concentrating, remembering details, or making decisions, and may contemplate, attempt or commit suicide. Insomnia, excessive sleeping, fatigue, loss of energy or aches, pains or digestive problems may also be present (Fitzgerald & Rodins 2014). Depressed mood is always a psychiatric disorder. It may be a normal reaction to certain life events, symptoms of some medical conditions, or a side effect of some drugs or medical treatments (Paul Aveyard 2014). In particular, after severe episodes, sub-syndromal levels of depression are common and persistent (Kennedy Abbott, & Paykel, 2004). In other patients, symptoms remain relatively stable at the level of full episodes over periods of more than 24 months (Mueller et al., 1996). Recent research has indicated that regardless of their presentation, i.e., whether patients continue to suffer from syndromal levels of the disorder or fluctuate between syndromal and sub-syndromal levels, chronic forms of depression are broadly homogeneous with regard to both their clinical and etiological features, while, at the same time, differing in important regards from episodic forms of the disorder (McCullough et al., 2003). For example, individuals suffering from chronic forms of depression have been found to be more likely to have a familial history of chronic depression (Klein et al., 1995), to be more likely to have suffered from early adversity (Lizardi et al., 1995), to be more likely to suffer from high levels of chronic stress and to be more likely to suffer from co-morbid disorders, particularly personality (Garyfallos et al., 1999; Pepper et al., 1995) and anxiety disorders (Weissman, Leaf, Bruce, & Florio, 1988). Most importantly, chronic forms of depression have been found to be significantly less responsive to treatment (Thase, Reynolds, Frank, & Simons, 1994) with reports of rates of responders to single modality treatments in trials aimed at chronic depression or based on samples with highly recurrent forms of depression at about 50% (DeRubeis et al., 2005).
2. What is Mindfulness
- Mindfulness refers to a psychological quality that involves bringing one’s complete attention to the present experience on a moment-to-moment basis, (Hofimann 2011) or involves paying attention in a particular way: on purpose, in the present moment, and non -judgmentally, or involves a kind of non-elaborative, nonjudgmental, present-center awareness in which each thought, feeling, or sensation that arises in the attentional field is acknowledged and accepted as it is (Russ Harris 2008) Bishop, Lau, and colleagues (2004) offered a two-component model of mindfulness: The first component [of mindfulness] involves the self-regulation of attention so that it is maintained on immediate experience, thereby allowing for increased recognition of mental events in the present moment. The second component involves adopting a particular orientation toward one’s experiences in the present moment, an orientation that is characterized by curiosity, openness, and acceptance (Bell 2009).In this two-component model, self-regulated (the first component) involves conscious awareness of one's current thoughts, feelings, and surroundings, which can result in meta -cognitive skills for controlling concentration (Hofimann, Sawyer, Witt & Oh 2010). Orientation to experience (the second component) involves accepting one's mind stream, maintaining open and curious attitudes, and thinking in alternative categories (developing upon Ellen Langer's research on decision-making). Training in mindfulness and mindfulness-based practices, oftentimes as part of a quiet meditation session, results in the development of a Beginner's mind, or, looking at experiences as if for the first time (Feider, Dimidjian & Segal 2012). Practicing mindfulness can help people to begin to recognize their habitual patterns of mind, which have developed out of awareness over time Melemis Steven, (2008) and this allows practitioners to respond in new rather than habitual ways to their life.. There is, thus, an important need for further refinement of treatments for those who have developed a more protracted course of the disorder.According to Jon Kabat-Zinn (2007), mindfulness can be defined as paying attention in a particular way on purpose in a present moment and non-judgmentally. Mindfulness is not a state of doing but a state of being in which you are fully aware of the present moment and do not evaluate your inner or outer environment. Mindfulness is a state of self-regulation of your attention and the ability to direct it towards breathing, eating, or something else. Curiosity, openness, and acceptance are all part of being mindful.Applications of mindfulness include emotional problems such as stress and anxiety; behavioral problems such as eating, parenting, and addiction; disorders such as depression, bipolar disorder, and borderline personality disorders; somatic problems including psoriasis, fibromyalgia, and chronic pain. People experience popping thoughts on the daily basis and many of these thoughts can be negative depending on the level of stress been experienced. To cope with negative popping thoughts, individual can use meditation to train him/herself to become aware of their wondering thoughts and bring back their attention to the present moment. People who are depressed, often have lots of negative popping thoughts about their past. A combination of mindfulness based stress reduction and cognitive therapy has been shown to be very effective for treatment of depression.Mindfulness-Based Cognitive Therapy (MBCT)Mindfulness–Based Cognitive Therapy that is designed to aid in preventing the relapse of depression, specifically in individuals with Major depressive disorder (MDD) (Chiase, Alberto, Callati, Raffaella, Serreti & Allessandro 2011). It utilizes traditional Cognitive behavioral therapy (CBT) methods and adds in newer psychological strategies, like mindfulness and mindfulness meditation. Cognitive methods could include educating the participants about depression (Khoury, Bassam, Lecomte, Tania, Fortin, Guillaume, Mosse, Marjolaine, Therien, Phillip, Bouchard, Vanessa, Chapleau, Marie-Andree, Paquin & Karine 2013). Mindfulness and mindfulness meditation, focus on becoming aware of all incoming thoughts and feelings and accepting them, but not attaching or reacting to them (Rapgay, Lobsang & Bystrisk Alexander 2009). Like CBT, MBCT functions on the theory that when individuals who have historically had depression become distressed, they return to automatic cognitive processes that can trigger a depressive episode (Wallace 2006). The goal of MBCT is to interrupt these automatic processes and teach the participants to focus less on reacting to incoming stimuli, and instead accepting and observing them without judgment. This mindfulness practice allows the participant to notice when automatic processes are occurring and to alter their reaction to be more of a reflection. Research supports the effects of MBCT in people who have been depressed three or more times and demonstrates reduced relapse rates by 50% (Hofmann, Sawyer & Fang 2012).In 1991 Bernard and Teasdalecreated a multilevel theory of the mind called “Interacting Cognitive Subsystems,” (ICS). The ICS model is based on Barnard and Teasdale’s theory that the mind has multiple modes that are responsible for receiving and processing new information cognitively and emotionally. Barnard and Teasdale’s (1991) theory associates an individual’s vulnerability to depression with the degree to which he/she relies on only one of the modes of mind, inadvertently blocking the other modes (Eleanor Rosch 2011). The central component of Barnard and Teasdale’s ICS is meta -cognitive awareness. Meta -cognitive awareness is the ability to experience negative thoughts and feelings as mental events that pass through the mind, rather than as a part of the self (Bell 2009). Individuals with high meta -cognitive awareness are able to avoid depression and negative thought patterns more easily during stressful life situations, in comparison to individuals with low meta-cognitive awareness (Maniacauasgar, Parker & Perich 2011). Meta-cognitive awareness is regularly reflected through an individual’s ability to decenter. Decentering is the ability to perceive thoughts and feelings as both impermanent and objective occurrences in the mind (Eleanor Rosch 2007). Several definitions of Cognitive-behavioral therapy (CBT) is considered to be one of the most effective and most researched methods of treatment for stress related disorders. However, a meditation approach called mindfulness-based cognitive therapy (MBCT) is quickly gaining more popularity in treatment of various disorders including depression. MBCT has the potential to improve one’s well-being, mindfulness, emotional regulation, positive mood, and spiritual experience while reducing stress, anxiety, and other problems. Eisendrath suggests that applying MBCT to treat depression can be a very effective approach (Chiase, Alberto, Callati, Raffaella, Serreti & Allessandro 2011).MBCT was originally developed as a relapse prevention program to help people stay free of depression once they have fully recovered from an episode. In the study about depression treatment methods, many more people who were treated with MBCT have stayed free of depression (about twice as many). These results were confirmed by a repeat study. Other studies have showed that the results achieved by MBCT were equivalent to the results achieved by antidepressants (Piet, Hougoard 2011). MBCT prioritizes learning how to pay attention or concentrate with purpose, in each moment and most importantly, without judgment (Herbert, james, Evans & Forman 2011). Through mindfulness, clients can recognize that holding onto some of these feelings are ineffective and mentally destructive. MBCT is an intervention program developed to specifically target vulnerability to depressive relapse. Throughout the program, patients learn mind management skills leading to heighten meta-cognitive awareness, acceptance of negative thought patterns and an ability to respond in skillful ways. During MBCT patients learn to decenter their negative thoughts and feelings, allowing the mind to move from an automatic thought pattern to conscious emotional processing (Manicavasgar, Parker & Perich 2011). Almost all the participants were taken antidepressant medication as at the commencement of this programme however none of the participants had previously received some form of psychotherapy or counseling. In order to fill this gap the current study utilizes mindfulness-based cognitive therapy to reduce relapse in depression among the outpatients of the hospital of study.Evidence of Reduced Depressive Symptoms, Anxiety with MBCTKunyken et al 2008 in his randomized controlled trial of 123 patients with recurrent depression treated with antidepressant received maintenance antidepressant alone or adjunctive MBCT with support to taper/discontinue antidepressant therapy found that adjunctive MBCT was as effective as maintenance antidepressants in reducing relapse/ recurrence rates but more effective in reducing residual depressive symptoms and improving quality of life; He also found out that 75% in the MBCT group discontinued antidepressant after the treatment. Testifying to the effectiveness of MBCT, when exposed to randomized controlled trials 19 out patients with residual depressive symptoms following a depressive episode MBCT or treatment as usual there was significant reduction on depressive symptoms and these improvements were maintained over a 1-month follow-up period (Kingston et al 2007). Again MBCT resulted in a significant reduction in anxiety scores on a Beck Anxiety Inventory (BAI) compared with wait-list controls when 14 patients with bipolar disorder who had no manic episode in the previous 6months and in less than a week of depressive symptoms in the last 8weeks. Using uncontrolled trials Eisendrath et al (2008) lend credence to the effectiveness of MBCT on 15 patients with treatment resistant depression. He confirmed that MBCT significantly reduced anxiety and depression, increased mindfulness and decrease rumination and anxiety were associated with decreased depression. In his own uncontrolled trials Finucane and Mercer, (2006) treated 13 patients with recurrent depression and anxiety with MBCT and the result indicated that MBCT significantly reduced depression on Beck Anxiety Inventory, BAI and Beck Depression Inventory (BDI-II). Also in his own research Kenny and Williams (2007) exposed 46 depressed patients who had not fully responded to standard treatments to MBCT. The result reveals that MBCT significantly reduced depression scores. Ree and Craigo (2007) confirmed that MBCT significantly improved symptoms of depression, anxiety, stress and insomnia, and improvement in insomnia were maintained at a 3-month follow up among 26 outpatients with mood and anxiety disorders.
3. Objectives of the Study
- The main objective of this study is to assess the impact of mindfulness-based cognitive therapy in the management of depressive symptoms of outpatients of state hospital in Oyo state in Ibadan Nigeria.The other objectives include;-1. To examine the effectiveness of mindfulness – based cognitive therapy in the treatment and the control group.2. To evaluate the impact of treatment outcome on participants’ depressive symptoms based on gender.3. To assess the impact of MBCT on the depressive symptoms of the participants based on marital status.4. To determine the impact of MBCT on the depressive symptoms of the participants based on religion.
4. Research Hypotheses
- The following null hypotheses were formulated and tested to guide the study at 0.05 level of significant1. There is no significant main effect of treatment on depressive symptoms of the participants.2. There is no significant main effect of gender on depressive symptoms of the participants. 3. There is no significant main effect of marital status on depressive symptoms of the participants. 4. There is no significant main effect of religion on depressive symptoms of the participants.
5. Methods
- DesignThe research design adopted for this study was a pre-post-test quasi experimental design, using 2×2×2 factorial matrix. The two refers to the treatment which comprises one experimental group and the control group. The treatment and the control group makes up the row. The first major column consists of the gender of the participants varying at two levels of male and female while the other major column connotes marital status separated into single and married. This design was adopted in order to establish cause and effects.Sample and Sampling TechniquesParticipants were recruited through local advertisements and posters pasted round the hospital where the treatments programme took place. Interested individuals were screened with Beck Scale for Suicidal Ideation (BSSI) after which eligibility for participation was assessed. Inclusion criteria were (a) a history of at least three previous episodes of Major Depression or Chronic Depression for at least two years, (b) a current diagnosis of Major Depression or presence of residual symptoms following a full episode of depression over the last two weeks or suffering from five or more symptoms. (c) a history of suicidal ideation (including thoughts of methods of suicide) or suicidal behavior (d) adequate written and spoken English to complete all study measures, (e) not currently in individual or group psychotherapy and no current ongoing meditation practice, and (f) age between 18 and 55. Thirty Two (32) depressed outpatients attending Adeoyo State Hospital were finally selected to participate in the study. Out of the participants 10 (31.25%) were males while 22 (68.75%) were females, concerning their marital status 7 (21.88%) were single while 25 (78.12%) were married, of married participants 16 (50%) were co- habiting. The religion affiliation of the participants shows that 13 (40.63%) were Christians and 19 (59.37%) were Muslims. Almost half of the participants 14 (43.8%) were in their middle age. As at the beginning of the treatment programme28 (87.5%) almost all the participants were taken antidepressant medication at the beginning of this programme. Participants were randomly allocated to MBCT (with programme holding at the Adeoyo State Hospital Ring road in Ibadan while the CONTROL GROUP were depressed outpatients of Adeoyo State Hospital Yemetu in Ibadan) after eligibility was ascertained.
6. Instrument
- Two instruments were utilized in this study. They are;-Beck Scale for Suicide Ideation (BSS; Beck & Steer, 1991)BSS was used as screening device to select the participants of the study. The BSS was used to measure presence and severity of suicidal ideation. The self-report questionnaire comprises 21 groups of statements including a screening section that contains five items specifically designed to identify suicidal ideation in active or passive form. Individuals whose answers in the screening section indicate suicidal ideation were asked to answer 14 further items assessing the extent of their wish to die. Two further items asked for information about previous suicide attempts. The total score for the 21 items is 42. The higher the score the participants obtained, the greater the symptoms of suicidal ideation. In order to establish the pilot study, the instrument was administered to 10 depressed outpatients of a replica hospital other than the targeted hospital. The data collected was subjected to Guttman Split–Half reliability procedures. It recorded a Cronbach coefficient alpha of 0. 87.Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996)Self-reports on the BDI-II was used to measure severity of current depressive symptoms pre- and post-treatment. The BDI-II contains 21 statements, assessing symptoms over the preceding two weeks. Beck, Steer, and Brown report excellent internal consistency in both patient and student samples. The manual of the scale indicates that scores between 1-10 is considered to be ‘‘Normal’’, 11-16 is considered to be “Mild Mood Disturbance”, 17-20 is regarded as “Borderline Clinical Depression”, 21-30 is considered as “Moderate Depression”, 31-40 is “Severe Depression” while scores above 40 is “extreme Depression” All the participants of this study had scores above 31 which indicates that they were severely depressed prior to the commencement of the treatment programme. The researcher undertook the re-validation of the instrument by pilot–testing it on another group of depressed patients different from the participants of the study. The test –retest techniques was adopted in the revalidation process and it yielded a reliability index of 0.73.
7. Procedure
- The study had received full approval of the Ministry of Health, Department of Planning, Research & Statistic Division of Oyo State. Research Ethical Committee (Ref: AD 13/479/619). Thus the official consent and approval was obtained for the programme. The treatment programme commenced with the introduction of participants to each other and introduction of therapists to the participants. The participants were informed that the treatment programme will cover a period of 8 weeks of 2 hours per session in a week. The experimental sessions started with the preamble and orientation for the participants, which includes the introductory talk to establish rapport and enabling environment for the programme. The objectives of the programme and the benefits to be derived by the participants were also discussed. The participants were informed that to achieve significant positive results with the treatment of depression they should be willing to practice daily meditation for at least 30 minutes in a day. Information was also given to the participants that mindfulness based meditation includes body scanning, mindfulness stretching, some elements of yoga, mindful breathing, [mindful eating and other daily mindful practices. Participants were informed that much of the practice would be done outside of classes, where the participants will use guided meditations and attempt to cultivate mindfulness in their daily lives. The therapists also sought for the co-operation of the participants. The following Skills and Practices were taught in Mindfulness-Based Cognitive Therapy for eight weeks consecutively;-• Automatic pilot (Acting without conscious awareness)• Dealing with barrier.• Mindfulness of the breath and body.• Awareness of attachment and aversion.• Acceptance of thoughts and emotions as fleeting events.• Decentering or re-perceiving.• Awareness of sign of relapse, develop more flexible, deliberate responses at time of potential relapse.• Awareness of intention as a skill of dealing with future depression.
8. Treatment
- First and foremost, the researcher introduced herself as facilitator and other class- support personnel with whom she will coordinate the training sessions. Participants were warmly received and introduced to one another in a friendly manner devoid of strict regimentation. Participants were informed of the duration of the programme (eight weeks) and that each session would be held for a maximum of two hours. On this note, a time table for the training session was drawn with full consultation with the participants. The pre-test measure was administered to both the treatment and the control group participants. Attendance record as well as phone contacts of the participants were taken. SESSION 1;- The therapist discussed with the participants that MBCT is an intervention programme developed to specifically target vulnerability to depressive relapse. She explained to the participants what depression is, the negative effects of depression and why the participants should not allow depression and its symptoms to relapse. She further discusses with them that distractions and ruminations make people work in an auto-pilot or acting without conscious awareness. The participants were taught that when they are mindful, they are likely to control their emotions and be creative. That mindfulness is a flexible state of mind in which individual is actively engaged in the present, noticing new things and sensitive to context. It can be seen as keeping one’s consciousness alive to the present reality. The therapists discussed the characteristics of mindfulness such as observing, describing, participating fully, being non-judgmental and focusing on one thing at a time with the participants. As take home assignment, the participants were asked to write those things they feel are making them to be depressed. SESSION 2:- Those things the participants identified as the causes of their depression in the previous session formed the basis of discussion in this session. The participants were trained on how to deal with barrier. They were taught that everyday mindfulness allows an individual to develop insight into psychological functioning and to respond skillfully to new situation. Mindfulness in deep meditation provides insights into the nature of mind and the causes of suffering. These insights such as awareness of how impermanent things really are, helps an individual become less entangled in his/her ruminations and thereby foster mindfulness. They were taught that mindfulness can help an individual step out of their conditioning or imaginations or daydreams and see things just the way they are. Both the therapists and the participants discuss how mindfulness reduces depression, increases a greater sensitivity to one’s environment. It is taught to enhance creativity, problem-solving techniques and openness to new information. SESSION 3:- Mindfulness of the breath and body was discussed with the participants. They were trained in the awareness of breathing meditation. Awareness of attachment and aversion was also discussed. The participants were asked to practice breathing meditation for 30 minutes after the therapists had trained them in the skills. Corrections were made where and when necessary. The participants also received training on how to work with intense physical sensation. The therapist and the participants discuses breathing meditation as a way of reducing depressive relapse. The participants were trained that meditation refers to a variety of practices that intentionally focus attention to help the practitioner disengage from unconscious absorption with thought and feelings. They were also taught to differentiate between concentrative mediation in which practitioner focus attention on a single object such as body part, or external object in mindfulness meditation, the participants focus their attention to a wide range of objects (such as breath, body, emotions). SESSION 4:- In this session the participants were taught to be sensitive and observant to the happenings in their environment. They were also taught to be creative and innovative. They were informed that a mind ruminating in the past thoughts or future inauguration may not be creative because it takes careful observation of the present happening to discover better ways to handle things. The participants were also taught to avoid bias because an individual beclouded by beliefs, assumptions, expectations and desire such are more prone to attaching meaning to things than seeing things the way they are. To be mindful connotes that when an individual observe things, describe things, they should keep an open mind to those things. The moment a person attach meaning to an action or feeling, the mind begins to race thoughts and the emotions are stimulated and a person is likely to be lost from his/her present happening to his/her imaginations. This situation is likely to stimulate negative emotions which can be harmful to the individual’s health and relationship with others. SESSION 5:- This session witnessed training in the acceptance of thoughts and emotions as fleeting events. Explicit instructing to practice acceptance were included in the breathing meditation and the 3minutes breathing space. The participants were taught in self-compassion which means acceptance of thoughts without judgement and softening of self-criticism. They were also trained on how to buffer negative self-feelings, prevents being overwhelm with negative emotions and how to reduce negative reactions in ways that are distinct from self-esteem. SESSION 6:- In this session, the participants were taught decentering or how to re-perceive their negative thoughts and feelings, and allowing their mind to move from an automatic thought pattern to conscious emotional processing. The clients were trained in cognitive change awareness. This is also called meta-cognitive. This aspect of training involves the development of a “distance” or “decentred” perspective in which clients experience their thoughts and feelings as “mental events” rather than as true, accurate versions of reality. This is thought to introduce a “space” between perception and response that enables clients to have a reflective rather than a reflexive or reactive response to situations, which in turn reduces vulnerability to psychological, processes that contribute to emotional suffering. This is capable of reduce risk of depressive relapse.SESSION 7: In this session the therapists discussed awareness of intention as a skill of dealing with future depression with the participants. They were taught that mindfulness is not an unconscious act. It connotes bringing to consciousness those things happening to individual at present moment. It is a skill that an individual must consciously learn and imbibe so that individual can consciously and intentionally decide to take note of the actual happenings around him/her. The participants were taught to avoid operating in an auto-pilot where individuals body carrying out their routine duty without the actual involvement of their minds. The therapists gave example of a situation where an person goes to the hospital and find it difficult to remember the route to his/her resident because he/she was ruminating on the discussion he/she just had with the doctor in the hospital concerning his/her state of health. SESSION 8:- The therapist led the participants to reflect on the effect of the therapeutic session. The therapists accomplished this by asking questions based on the experience the participants have been exposed to determine their level of comprehension. To make it more effective some of the previous sessions were rehearsed to facilitate lasting retention by the participants. Post-test measure was administered on both the participants and the control group. Responses obtained were subjected to data analysis.
9. Data Analysis
- Analysis of Covariance was the statistical tool utilized in this study. This statistical tool was utilized because it has ability to control errors, adjust treatment means, partition a total covariance, estimate missing data, correct initial mean differences between the experimental and the control group.
10. Results
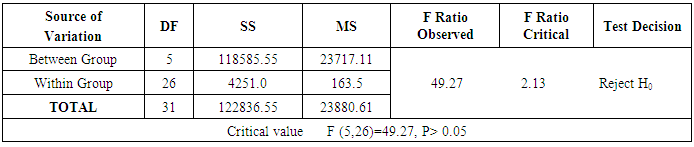
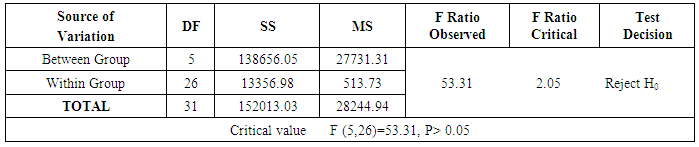
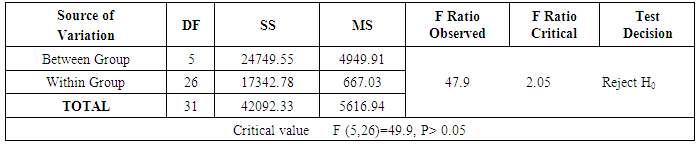
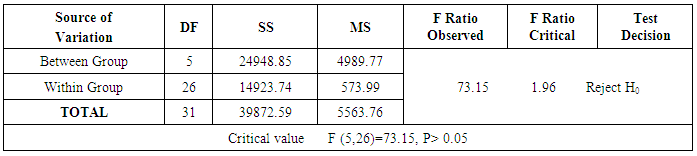
- The result as shown in table 1 indicated that there was significant main effect of treatment on the participants depressive symptoms. The null hypothesis was therefore not sustained. It was evident as shown in the analysis of covariance in Table 1 that there was significant decrease in the level of depressive symptoms as indicated on the Post-test scores of Participants (F 5, 26)=49.27 P>0.05).As revealed in table 2, the post treatment outcome of Male and Female participants indicated significant main effect of treatment on their depressive symptoms. Thus the null hypothesis was not supported.The Post-Treatment outcome as indicated in table 3 showed that there existed significant main effect of treatment on depressive symptoms of the participants. Thus the null hypothesis was not accepted.The compared outcome of Pre-post treatment revealed that there was significant main effect of treatment on depressive symptoms of the participants. It follows therefore that the tested hypothesis was not upheld.
|
|
|
|
11. Findings
- The following are the findings of this study;-1. There was significant main effect of treatment on the participants depressive symptoms2. The post treatment outcome of Male and Female participants indicated significant main effect of treatment on their depressive symptoms. 3. There existed significant main effect of treatment on marital status on depressive symptoms of the participants.4. There was significant main effect of treatment on religion on depressive symptoms of the participants.
12. Discussion
- This study investigated the impact of MBCT in the reduction of symptoms of depression in currently symptomatic patients who suffer Chronic and recurrent depressive symptoms. The results of hypothesis one showed that treatment with MBCT significantly reduced self-reported symptoms of depression from severe to mild levels, while levels of depression remained unchanged in the control group. This result lend support to the studies of Chiase et al (2011) that MBCT has the potential to improve one’s well-being, mindfulness, emotional regulation, positive mood, and spiritual experience while reducing stress, anxiety, and other problems. Eisendrath further suggests that applying MBCT to treat depression can be an effective approach. This study also corroborates that of Maniacauasgar, Parker & Perich (2011) which says that individuals with high meta-cognitive awareness are able to avoid depression and negative thought patterns more easily during stressful life situations, in comparison to individuals with low meta-cognitive awareness. The result obtained in this study is not by accident because the treatment programme really emphasizes meta-cognitive awareness in individual participants as it is regularly reflected through an individual’s ability to decenter. The participants were also trained that ‘”decentering” is the ability to perceive thoughts and feelings as both impermanent and objective occurrences in the mind (Eleanor Rosch 2007). The findings of this current research corroborates the work of Eisendrath et al (2008) who lend credence to the effectiveness of MBCT on 15 patients with treatment resistant depression. He confirmed that MBCT significantly reduced anxiety and depression, increased mindfulness and decrease rumination and anxiety were associated with decreased depression.The results obtained from this study also indicate significant difference in the decrease of depressive symptoms of male and female participants. The reason for this is not far- fetched taken into consideration the fact that women more than men easily release pent up emotions Again the practice of regular meditation can produce lasting effects on attention, executive functioning (Lutz, Slagter, Dunne, & Davidson, 2008; Slagter et al., 2007; Tang et al., 2007) and emotion regulation (Nielsen &Kaszniak, 2006). Systematic training of these functions through meditation may be particularly helpful in patients suffering from chronic depression where vulnerability processes such as rumination are likely to have acquired a habitual and automatic character and are more likely to occur when cognitive control is undetermined. The participants were engaged in regular meditation during the treatment programme which was a form of exercise, exercise allows individuals to improve their health while building new relationships with others and bolstering the sense of community that comes with exercising as a group (Lopresti, Hood and Drummond 2013). Group activities can lower depression by increasing depressed individuals’ ability to interact with others. Exercise also increases individuals’ self-confidence by promoting social skills that people with depression often lack and interrupts the cycle of isolation from the general population that can further increase depression. Exercise fosters non-demanding behaviors while allowing people to socialize and identify themselves as part of the general. Again there was a general notion that females have advantage over males because of their susceptibility and receptive nature to behavioural change. The results obtained is therefore in line with several researchers who have worked with males and females, for instance, Lovell, Lee and Brotheridge (2009) found significant gender differences between female physicians and males in interpretation of non- verbal communication. The study of Kumar and Lal (2006) also supported this finding when they observed that females scored higher than their male counterparts in self–efficacy. The implication of this finding is that female participants have good and excellent adjustment level when compared to their male participant counterparts. Again MBCT involves engaging in series of home- work and assignment which the researcher observed were judiciously undertaking by the female participants. Infact, almost half of the participants (47%) reported that they have dropped antidepressants for the MBCT.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML