S. M. Raysul Haque 1, Shabareen Tisha 1, Munmun Mustafa 2, M. Omar Rahman 1
1School of Public Health, Independent University Bangladesh, Dhaka, Bangladesh
2Department of Community Medicine, Bangladesh Medical College, Dhaka, Bangladesh
Correspondence to: Shabareen Tisha , School of Public Health, Independent University Bangladesh, Dhaka, Bangladesh.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
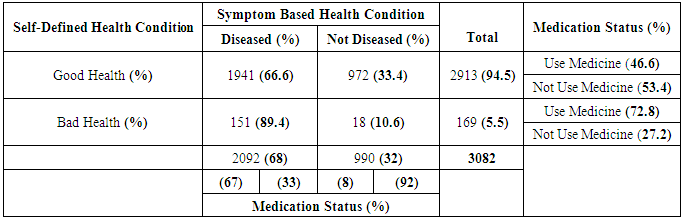
s A clear conception about the medication use pattern help us to determine the disease pattern as well as policy and budget making of a country for health sector. A developing country like Bangladesh where no prescription is essentially needed to purchase medicine, a population based study is essential to explore medication use pattern in the community. The purpose of this study is to reveal the influence of self- reported health on medication use amongst adults in Bangladesh considering symptom based health conditions as acute and chronic morbidity along with other relevant socio-demographic factors such as age, sex, income, site, level of education, marital status, employment status etc. “IUB Health and Socio Economic Survey” 2013 was used for this purpose. The sample size for this study was 3085 adults, randomly selected from four districts of the country. The result shows that 5.5% of the total study population reported bad health and 72.8% (out of 5.5%) took medicines although 10.6% of them have no symptom-based morbidity. On the other hand 94.5% reported as good health but 46.6% (out of 94.5%) consume medicines though 66.6% of them have at least one symptom-based acute or chronic morbidity. These simple figures allow us to consider that self-reported health is more practical and realistic predictor for medication use. Step wise logistic regression analysis was applied to examine the influence of self- reported health on medication use as well as other relevant variables. In the final model the results of the analysis show that self-reported health is positively and statistically significantly (P=0.010 & odds ratio = 2.018) associated with the likelihood of an adult person will take medicine after controlling for all other potential factors. So it can be concluded that the self-reported bad health group has two times higher medicine consumption than self-reported good health group even after controlling symptom based health conditions-acute and chronic morbidities along with other relevant socio-demographic factors. Self-reported health at a practical level is a very important predictor of medicine use for Bangladesh. This result may have important impact on health policy implication and treatment strategy at community level in Bangladesh.
Keywords:
Self-reported Health, Medication use pattern, Bangladesh
Cite this paper: S. M. Raysul Haque , Shabareen Tisha , Munmun Mustafa , M. Omar Rahman , Pattern of Medication Use and Its Association with Self-Reported Health in, Bangladesh, American Journal of Medicine and Medical Sciences, Vol. 5 No. 1, 2015, pp. 31-41. doi: 10.5923/j.ajmms.20150501.07.
1. Introduction
Bangladesh is one of the poor and overcrowded countries in the world [1]. Poverty, educational status and social exclusion are the greatest threats to their well-being especially in health sector in rural areas [2] In spite of this socio-economic status due to well-designed and target oriented public health interventions, such as, immunization, oral rehydration therapy, family planning, nutritional health programs, life expectancy at birth have been increased from 45 years to 62 in the last three decades [3], though it’s not in a satisfactory and sustainable level. Despite of having overall success in increasing life expectancy and reaching MDGs (millennium development goals) [4] Bangladesh still lacks comprehensive structures that can provide basic information on disease pattern and medication use in the general population especially in rural areas, cause rural people have problems both in availability and access in health systems [5]. Mainly hospital data are available for medicines that are prescribed for different diseases [5]. Usually hospital data are not representative for a particular community. In such scenarios, population-based, cross-sectional studies are important to provide information, as well as to determine the self-perception of health along with socio-demographic and clinical characteristics of the population and to examine their association with medication consumption [6, 7]. Medications are dynamic therapeutic tools used in the understanding of health and disease process which is responsible for wellbeing issues of human especially an important part of the increased life expectancy and excellence of life [8]. World Health Organization (WHO) has specifically emphasized the availability of essential drugs as a health indicator in developing countries [9]. In developing economies, social class, inequalities can have an additional impact on expanding the right to access to medicines and their rational use [10]. The use of medicines is influenced by demographic structure, socioeconomic, behavioral, cultural, biological factors, and the individualities of the pharmaceutical markets and government policies regarding drug manufacturing to marketing [11-13]. So to increase the life expectancy as well as the quality of health and to know more about the disease pattern we have to have a very clear picture about the medication use pattern and this set of factors (socio-economic, demographic and biological factors) need to be investigated to provide a better considerate role of drugs in the perspective of public health.As we have mentioned earlier it is recognized that the population-based assessments are suitable way for scrutinizing the health condition and performance of health systems [14]. The results obtaining from these studies are useful for health planning especially for a target community; it also provides valuable information for national health policies, pharmaceutical regulation, and sensible use of medicines [15]. Many studies have already conducted focusing on a specific group of medicine which provide information only about that particular drugs and its impact but in practical we found a very few large scale population-based studies on overall medication use pattern and its association with relevant factors. In case of Bangladesh there is no previous large scale study available addressing this particular issue.In general these population-based studies have pointed to a higher consumption of drugs among those with higher income group [11, 12, 13, 16, 17], among more educated people [12, 18], particularly in women [11, 12, 13, 19], especially with increasing age [11, 12, 13] and with a higher number of chronic diseases [11, 13, 17]. Considering all these research evidence in mind we want to explore the pattern of medication use among adults in four districts of Bangladesh and factors that might be associated with the use of medications. We have also considered other important factors that are mentioned in literatures and have some relation with medication consumption. So this paper will bring up the facts in variation of medication use as well as variation in disease pattern in population level which will give us a ground level picture regarding health status of the people of Bangladesh and the factors responsible for it particularly self-perception of health along with symptom based health conditions. Self-defined health condition is essentially a very important determinant of medicine use as no prescription is practically needed to purchase any sorts of medicine in most South Asian countries, including Bangladesh [20] whereas peoples of developed countries can’t even think about medicine purchase without physician’s advice in the form of prescription except the OTC (over the counter drugs - are non-prescription drugs sold in convenient stores, grocery stores and health shops). Corrupted drug sellers sell almost 90% of the stocked drugs without prescription, even the sedatives are also being traded like fast food in Bangladesh [21]. According to the Bangladesh chemist and druggist association on 2004 there were about 30,000 legal and more than 70,000 illegal drugstores and these are alleged to sell medicines without registered doctors' prescription [21]. As we can easily purchase medicines, self-perception regarding health condition play a vital role in medicine consumption along with well-established symptom based health conditions.
2. Research Hypothesis
The hypothesis considered in this paper is self-reported health is an important predictor for medicine consumption beside acute and chronic morbidity as it is already established that people will take medication when he or she will be badly affected by either acute or chronic cases irrespective of their socio-demographic status. Here we are focusing on the individual perception of health, disease and its relationship with medication consumption considering all other relevant variables.
3. Data and Method
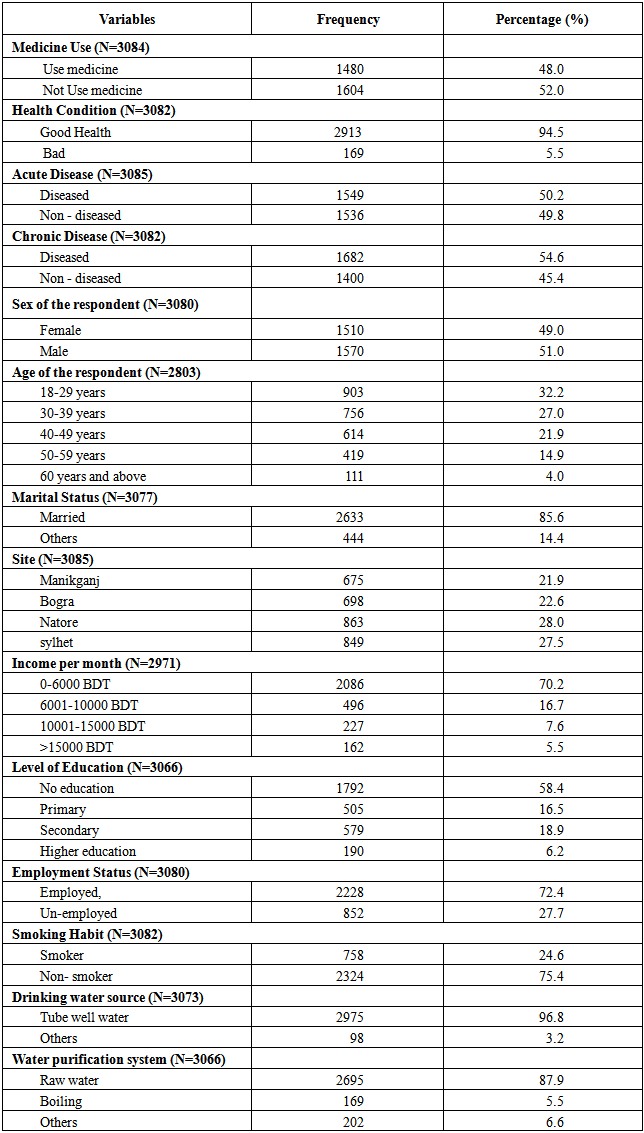
This is a cross-sectional population-based study that used data from the “IUB Health and Socio Economic Survey” 2013. The survey was performed under the authority of Independent University Bangladesh (IUB). The study performed in four districts (Manikganj, Bagura, Natore, Sylhet) of Bangladesh. Demographic, economic and clinical information were obtained by face-to-face interviews conducted at the participants' residence from 5th January -12th January, 2013 using a pre-tested questionnaire. In this particular study the primary outcome is the prevalence of medication consumption during the past 30 days. Eligible participants were adult residents of those four districts of Bangladesh, aged 18 and above. Initially those four districts, Manikganj, Bagura, Natore, Sylhet were purposively selected, then three villages from each district were randomly selected and then again proportionately household were selected randomly from each villages of that four districts. By this way we have covered 1310 households of four districts - 323 household from Manikganj, 299 from Bogra, 349 from Natore and 339 from Sylhet districts. Total numbers of participants are 3085 adults. Medication use is our dependent variable, outcome is whether they took at least one drug thirty days prior to the interview or not. The question was “Did you use any medicine in the last thirty days?”. Three sets of independent variables are analyzed: In case of health-related variables, general health condition (bad or good health), acute morbidity (diseased or non-diseased), chronic morbidity (diseased or non-diseased), Smoking habit (smoker, nonsmoker), drinking water source (tube well or others) and water purification system (boiling, raw water or others) were considered. In case of demographic variables we have considered, gender (female and male); age (18-29, 30-39, 40-49, 50-59 and 60 years or more); marital status (currently married, others) and Site (Manikganj, Bagura, Natore, Sylhet). Regarding socioeconomic variables, level of education (no education, primary, secondary and higher education); average household income per month (0-6000 BDT, 6001-10000 BDT, 10001-15000 BDT and more than 15000 BDT) and employment status (employed or un-employed) are considered.The analysis is done into two parts and into three steps. Firstly, here we have explored the pattern of medication consumption among those who took at least one medicine 30 days prior to the survey and what was the purpose of their medicine intake, thus we also get a disease pattern. Secondly univariate analyses are done for both dependent and independent variables. Then, bivariate analysis is done to examine the association between the dependent variable and all other independent variable separately. Finally, multivariate analysis is done by fitting the logistic regression model for medicine consumption to examine the impact of self-reported health after controlling the other relevant factors. This is done by following a step-by-step procedure and we included the factors in the logistic regression model those are found to be statistically significant in the bivariate analysis except sex of the respondent and income. Though they are not found significant in bivariate analysis but previous relevant studies suggests these two variables as sex of the respondent [11, 12, 13, 19] and income [11, 12, 13, 16, 17] are very important determinant of medicine use. So we also include these two variables in logistic regression model.In first step we have considered medicine consumption and self-reported health as bad health in reference to good health and in second step we also include age of the respondent as 30-39, 40-49, 50-59, 60 years or more in reference to 18-29 group; marital status as currently married in reference to other marital status; sex of the respondent as female with the reference of male and level of education as primary, secondary and higher education group with the reference to no education group. In third step we have considered site as Manikganj, Bagura and Sylhet in reference to Natore; average monthly income as 6001-10000 BDT, 10001-15000 BDT and more than 15000 BDT categories with the reference of 0-6000 BDT group and employment status as employed in reference to un-employed along with the variables of previous step. In fourth and the final step we also include acute morbidity as diseased with the reference to no disease; chronic morbidity as diseased in reference to non-diseased and smoking habit as smoker in reference to nonsmoker.
4. Results
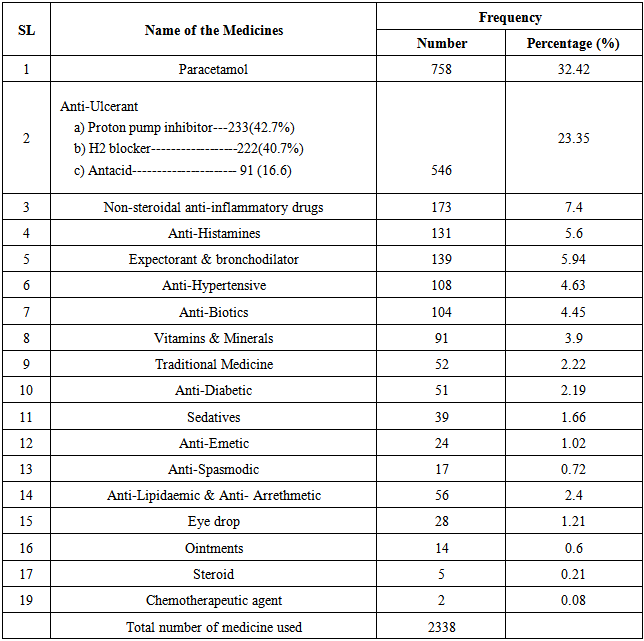
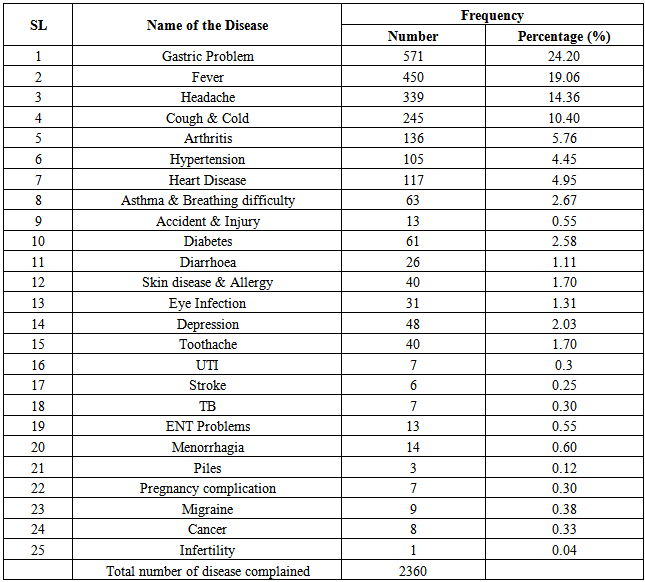
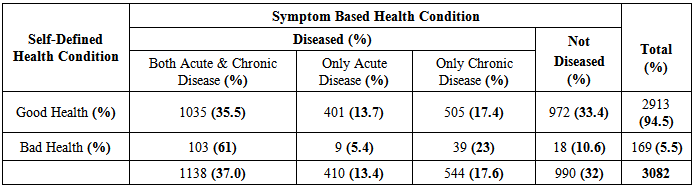
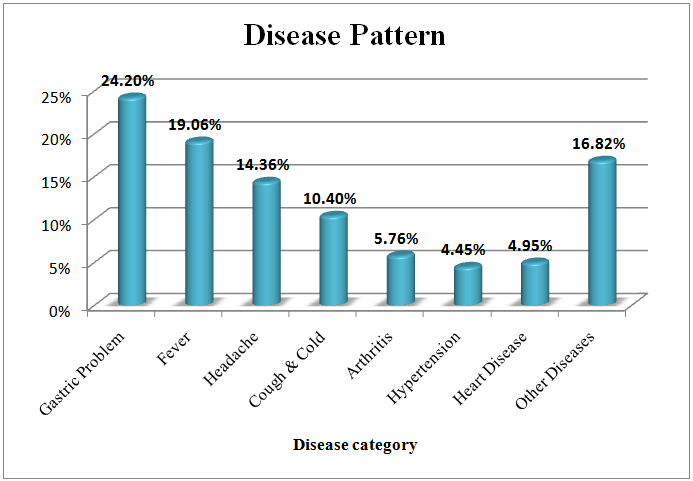
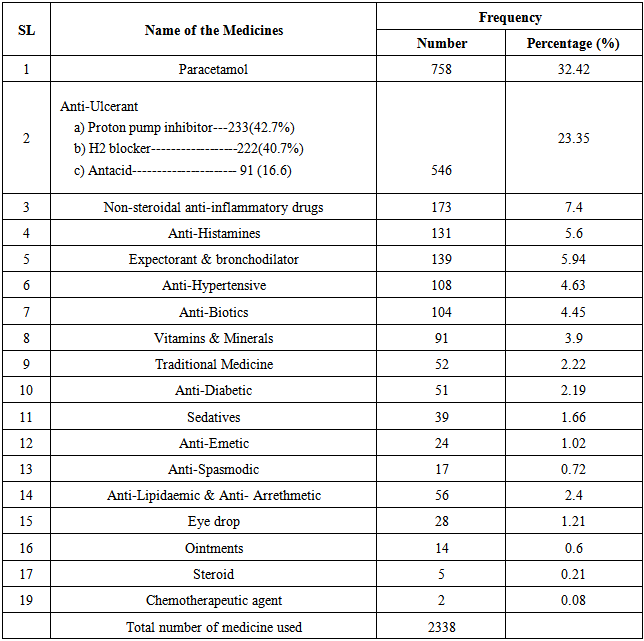
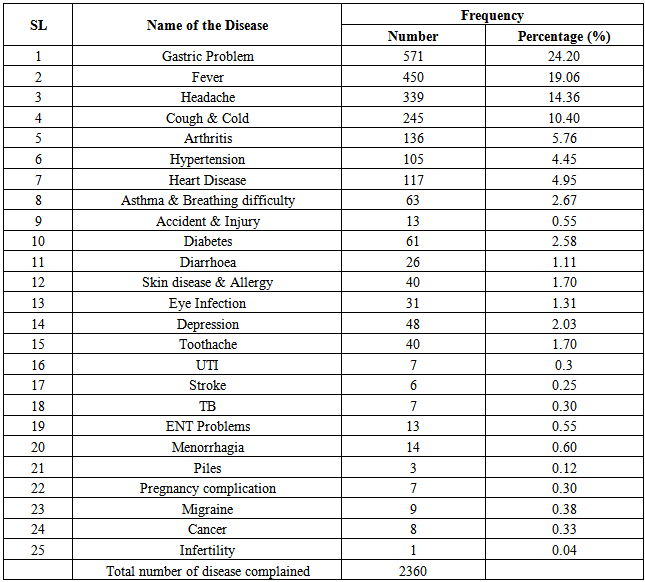
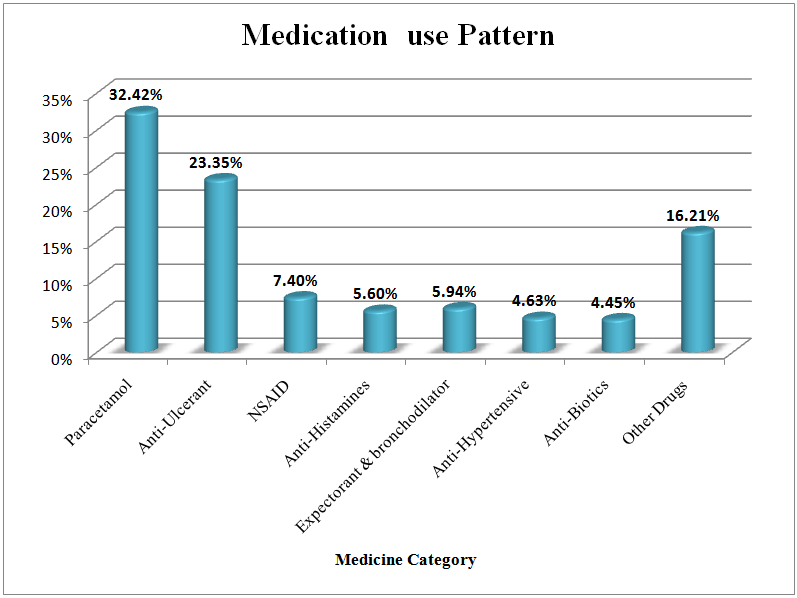
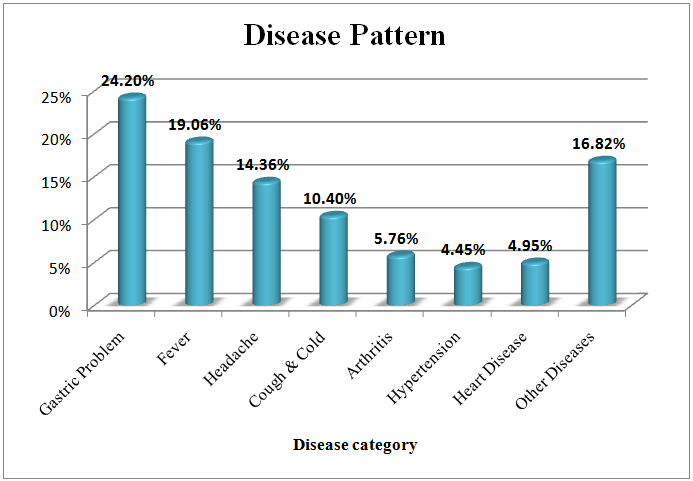
The study included 3085 people who are of 18 years or above and 51% (1570) of them are men and rest are female which is also representative of national male female ratio. According to table 3, among the study population, 48% (1480) took at least one medicine one month prior to the survey. Now we are going to explore the total medication taken by those 1480 individuals.As per table - 1 a total nineteen types and 2338 individual numbers of medicines were used. Highest frequency goes for Paracetamol which is 32.4% (758) and lowest for Chemotheraputic agent which is 0.08% (2). Second, third, fourth and fifth highest are for Anti-ulcerant (23.3%), Non-steroidal anti-inflammatory drugs (7.4%), Expectorant & Bronchodilator (5.9) and Anti-Histamines (5.6%) which is also represented by figure - 1. Table - 2 shows the study population were suffered from different types of diseases as per the cause of medicine uptake. A total twenty five types and 2360 individual numbers of diseases were detected. Gastric problem is the highest in prevalence which is 24.2% (571) and Infertility is the lowest which is 0.04% (1). Second, third, fourth and fifth highest are for Fever (19%), Headache (14.3%), Cough & Cold (10.4) and Arthritis (5.7%) which is also represented by figure-2. This disease pattern is representative of medicine consumption.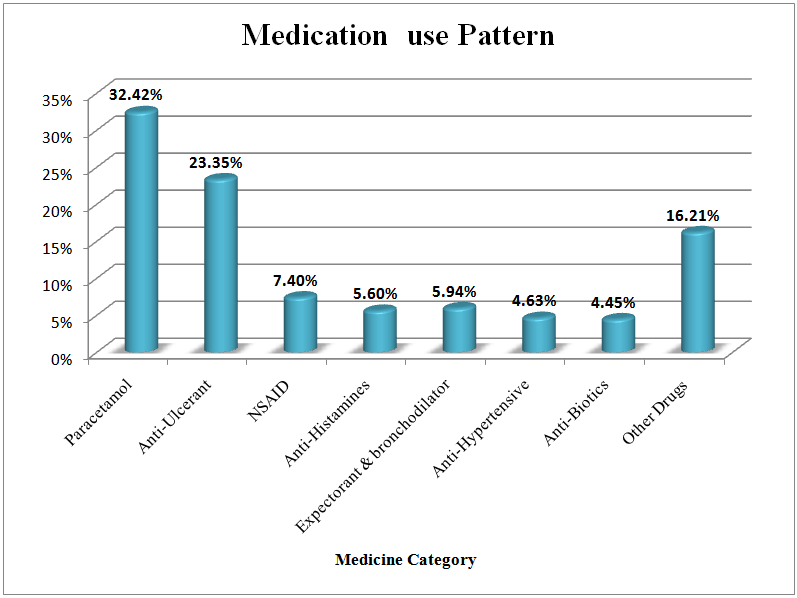 | Figure 1. Medication Use pattern |
 | Figure 2. Disease Pattern as per medication consumption |
Table 1. The prevalence of medication use by the individuals 18 years and above
 |
| |
|
Table 2. Disease prevalence as per the reason of medication consumption for the individuals, 18 years and above
 |
| |
|
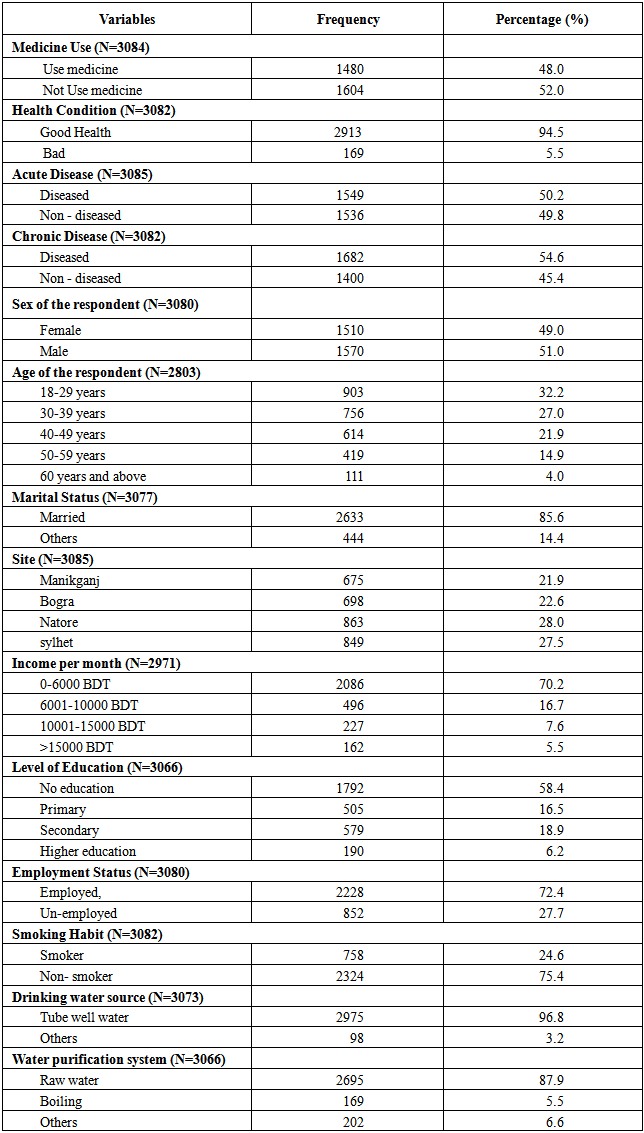
Now we are going back to table-3 which describes the profile of both dependent and independent variables. According to this table 94.5% (2913) are in good health condition as per their own perception that is self-reported health, in this particular case our question was, “What is your health condition?” We have also assessed them based on acute and chronic symptoms and created the variable acute and chronic morbidity. As few people have both acute and chronic morbidity, out of total study population, 50.2% are reported as acute and 54.6% as chronic morbidity. We have categorized the age and income as shown in this table. Married group consists 85.6% and employed group 72.4%. 24.6% are smoker while level of education categorized as no education (58.4%); primary (16.5%); secondary (18.9%) and higher as 6.2%. Regarding site, highest 28% and lowest 21.9% lived in Natore and Manikganj respectively. In case of water sources 96.8% use tube-well water while 87.9% drink raw water.Table 3. Frequency distribution of selected independent and dependent variables
 |
| |
|
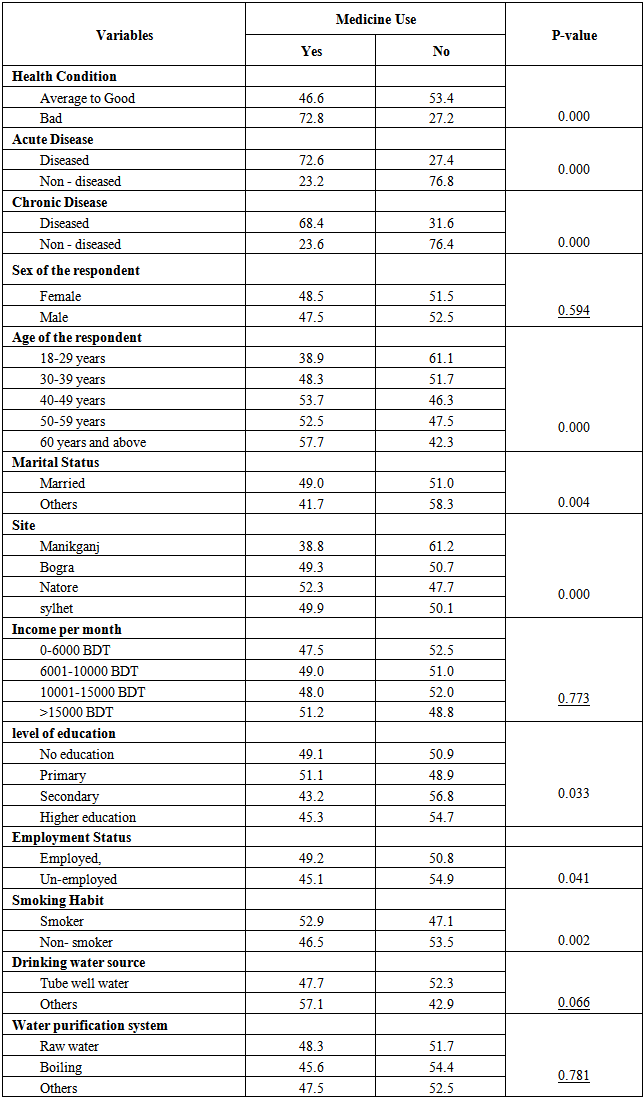
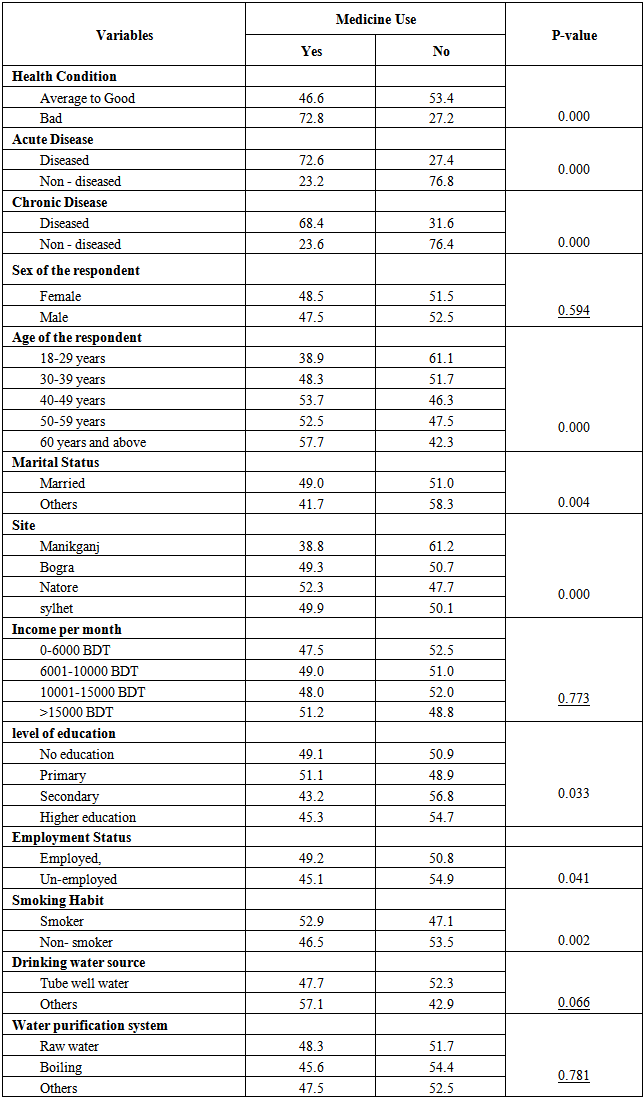
Table - 4 represents the results obtained from the bivariate analysis for medication use with all independent variables. Out of all independent variables four appears insignificant as p-value is greater than 0.05. These four variables are sex of the respondent, income per month, drinking water source and water purification system. It is to be noted that the p-values for these four variables are 0.594, 0.773, 0.066 and 0.781 respectively. Out of remaining nine significant variables medicine consumption is certainly high in bad health group, acute diseased and chronic diseased group which is 72.8%, 72.6% and 68.4% respectively. Under the age group, those who are 60 years and above have highest medicine consumption that is 57.7% and 18-29 years group have lowest medicine consumption that is 38.9%. In case of both employment and marital status, medicine consumption is higher for employed and married group in comparison to unemployed and other marital status (non-married, divorcee etc.) group. Medicine consumption is slightly higher for smokers (52.9%) than nonsmokers. Within the level of education primary education group has highest medicine consumption that is (51.1%) and the secondary education group have the lowest medicine consumption (43.2%) and no education and higher education group have (49.1%) and (45.3%) medicine consumption respectively. Medicine consumption in case of site, Natore hold the highest position that is (52.3%) and Manikganj stand for lowest position that is (38.8%). Medicine consumption in other two places are similar that is Bogra (49.3%) and Sylhet (49.9%) respectively.Table 4. Examining the association between Medicine consumption and selected independent variable: A bivariate analysis
 |
| |
|
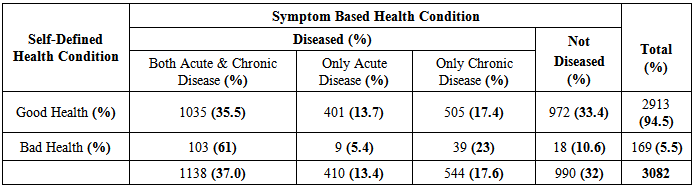
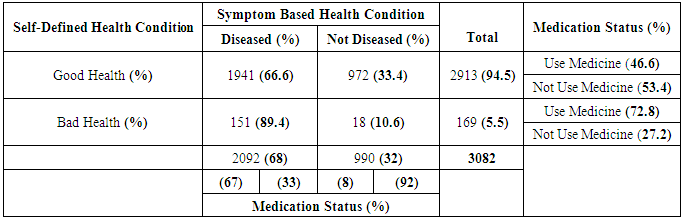
According to table 5.1, 5.5% of the total study population reported as bad health and within this group considering symptom based status 61%; 5.4% and 23% have acute & chronic; only acute and only chronic morbidity respectively, although 10.6% had no symptom based morbidity. On the other hand 94.5% of the study total study population reported as good health although 35.5%; 13.7% and 17.4% had acute & chronic; only acute and only chronic morbidity respectively and only 33.4% had no symptom based morbidity.Table 5.1. Symptom Based Health Condition (acute and chronic morbidity) and self-defined health condition among study population
 |
| |
|
According to table 5.2, 5.5% of the total study population reported bad health although 10.6% of them had no symptom based acute or chronic morbidity and 72.8% (out of 5.5%) took medicines. On the other hand 94.5% reported as good health although 66.6% of them had at least one symptom based acute or chronic morbidity but only 46.6% (out of 94.5%) consume medicines. On the basis of symptom based morbidity 68% were suffering from either acute or chronic or both morbidity and rest 32% had no symptom based morbidity. 67% were taking medication among this 68% study population and 8% (within that 32%) take medicines who had no symptom based morbidity.Table 5.2. Symptom Based Health Condition and self-defined health condition in aspect of medication consumption
 |
| |
|
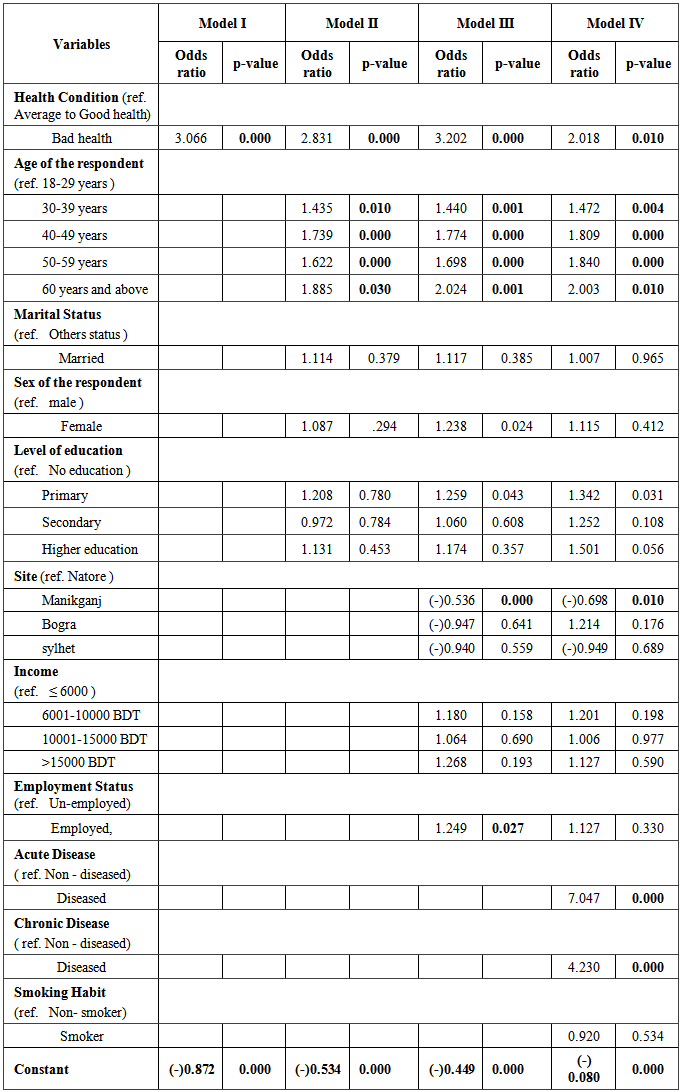
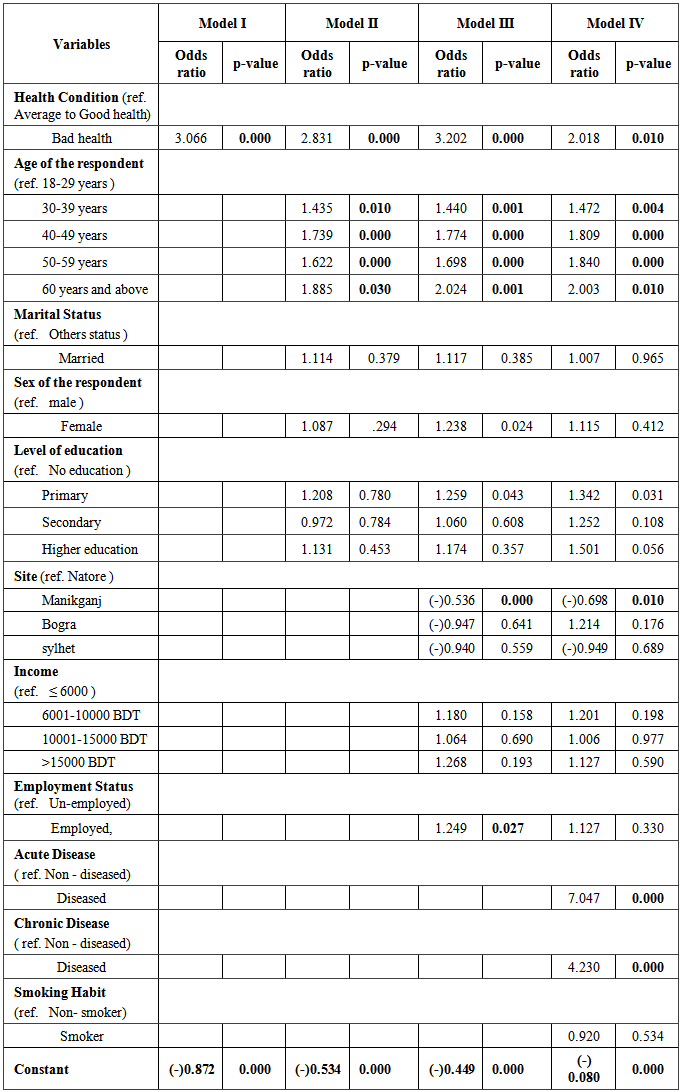
In Table 6, Model I presents the first logistic model for Medicine consumption along with self-reported health represented by bad health. It is found that self-reported health condition has a significant (p-value=0.000) positive impact on medicine use. With the reference of good health group, bad health group have 3.066 times higher medicine consumption.Table 6. Step wise Logistic regression models for medicine consumption after controlling all other factors - A multivariate analysis
 |
| |
|
Model II in Table 6 represents the second logistic model for medicine consumption where we include age of the respondent, sex of the respondent, marital status and level of education along with variables considered in Model I. After considering all these variables, self-reported health still remains significant for medicine consumption where bad health group has 2.831 times higher consumption than good health group and p=0.000. All the age groups of the respondent have a dose response effect on medicine consumption in comparison to ref. group that is 18-29 years group and found statistically significant. Sex of the respondent, marital status and level of education have no significant effect on medicine consumption.Model III in table 6 presents the third logistic model for medicine consumption where we include site; average monthly income and employment status along with all variables considered in Model II. After including these three variables, self-reported health, still remains highly significant for medicine consumption. The p-value is still 0.000 for bad health group. Here, bad health group have 3.202 times higher medicine consumption than good health group. In case of Manikganj, people take 47% less medicine than that of Natore and it is statistically significant and those who are employed take 24% more medicines than unemployed people and it is also statistically significant. Age has the same effect like the previous model. For the first time sex of the respondent seems significant for medicine consumption as p=0.024. Income has no such effect on medicine consumption here. Considering education, primary education group have 25% more medicine consumption than no education group and it is statistically significant as p=0.043. Model IV in table 6 represents the last logistic model for medicine consumption where we include acute morbidity, chronic morbidity and smoking along with all variables considered in Model III. After considering all eleven variables in model IV, self-reported health still remains highly significant (p=0.010) for medicine consumption. Still bad health group have 2.018 times higher consumption of medicine than good health group. Here acute morbidity and chronic morbidity found to have significant effect on medicine consumption as odds and p values are (p=0.000 & odd=7.047) and (p=0.000 & odd=4.230) respectively. Smoking is not found to be a significant predictor for medicine consumption. We find the similar response for age of the respondent and for Manikganj in this model. In case of education the primary group takes 1.342 times higher medicines than no education group and it is also statistically significant since p-value is 0.031. Secondary and higher education group and employed group haven’t proven statistically significant for medicine consumption here.
5. Discussion
In this particular study we have explored the pattern of medication use in Bangladesh as well as disease pattern and the influence of self-reported health on medication use, over all other relevant factors. Here we have considered symptom based health condition as acute and chronic morbidity, two most well established factor for medication consumption. Our study also suggests that these two are particularly very important determinants for medication consumption as both acute and chronic morbidity are proven statistically very highly significant and odds ratios are 7 and 4 respectively for the medication consumption with their reference group, but a country like Bangladesh where availability of medication is not particularly related with physicians’ advice in the form of prescription, self-reported health is practically a vital predictor for medicine consumption. Our study also suggest that self-reported health is proven highly significant after controlling the most two important predictors, acute and chronic morbidity along with other relevant socio-demographic factors and the odds ratio is still 2.018 with the reference group. This indicates that only symptom based morbidity are not satisfactory enough to predict medicine consumption in community level in developing countries as self-perception of own health which is self-reported health, has proven an effective predictor for medicine consumption. In case of medicine consumption pattern among the study population, 48% which is nearly half, take at least one medicine one month prior to the survey. By this way we have found the pattern of medicine consumption and also the disease pattern for the reason they took medicines. On the basis of consumption highest frequency goes for Paracetamol (32.4%) and then Anti-ulcerant (23.3%) and Non-steroidal anti-inflammatory drugs or painkiller (7.4%). Simultaneously highest frequency of disease goes for Gastric problem and then Fever (19%) and Headache (14.3%). These medicine and disease patterns are representative for each other’s.An interesting finding in our study is we didn’t find any relation between income level and medicine consumption, which is an established fact. One possible explanation could be like this, most of the top frequently used drugs are relatively chap as for example one strip of Paracetamol costs only 15 to 20 BDT and anti-ulcerant for 20 to 40 BDT and these drugs are also available in the out-patient unit of public hospitals and in most of the studies (not exactly like ours) the top frequently used drugs are (oral contraceptive, antibiotics, analgesics) [22-25] which are relatively expensive. Like the other studies we also find significant dose response effect of age on medicine consumption. Another interesting finding is we didn’t find a significant effect of education (except primary education group) on medicine consumption. Regarding limitation of our study, first one is we are using a cross-sectional data instead of longitudinal data. Using a longitudinal data we can easily track the changes of self-reported health status over time and test it on medicine consumption along with other relevant variables. Second one is site; here we have covered only four districts of Bangladesh, if we can cover more than we might get more precious result.
6. Conclusions
We can sum up by saying that self-reported health is a practical and time demanding predictor for medicine consumption beside symptom based morbidity in a country like Bangladesh where availability of medicine in terms of physician’s prescription is not mandatory like the developed countries. Self-perception in any issues especially in health plays a huge role as we have seen that, once someone didn’t feel that he or she is sick then he or she didn’t go for any medicine uptake. In practical we have also seen that usually patients are not taking all the medicines prescribed by the physicians rather they took only those matches with their complains and up to the disappearance of the particular complains but not to the extend prescribed by the physicians. This also supports the role of self-reported health for the medicine consumption. Further large scale research, specially mixed method (both qualitative & quantitative) is needed to address this issue as we haven’t found much evidence on community or population level.
ACKNOWLEDGEMENTS
We would like to thank the authority of Independent University Bangladesh for permitting us to use the “IUB Health and Socio Economic Survey-2013”.
References
| [1] | UNFPA. Population and reproductive health country profiles: Bangladesh, 2003. Available from;http://www.unfpa.org/profile/banglade5h.cfm. |
| [2] | Help-Age International. Uncertainty rules our lives: the situation of older people in Bangladesh. Chiang Mai, Thailand: Help-Age International; 2000. p. 19. |
| [3] | Ahmed SM, Hadi A, Roy RO, Sarkar M, Chowdhury AMR, Revisiting the health of the population: agenda for the future. Dhaka: BRAC Research and Evaluation Division; 2001. |
| [4] | http://www.bd.undp.org/content/bangladesh/en/home/library/mdg/publication_1/, accessed on 24th September, 2014. |
| [5] | M Rahman1, MM Islam, MR Islam, G Sadhya, MA Latif, Disease Pattern and Health Seeking Behavior in Rural Bangladesh, Faridpur Med. Coll. J. 2011; 5(1):32-37. |
| [6] | WHO. Introduction to drug utilization research. 2003. http://apps.who.int/medicinedocs/en/d/Js4876e/ , accessed on 25th September, 2014. |
| [7] | Lee D, Bergman U, Strom BL, Kimmel SE, Hennessy S, Studies of drug utilization. In Pharmacoepidemiology (5-edn), Wiley-Blackwell: Oxford, UK, 2012; 379–401. |
| [8] | Arrais PSP, Medicines consumption and adverse reactions - A population-based study, Fortaleza: UFC Issues; 2009. |
| [9] | World Health Organization, The rational use of drugs, Geneva, 1987. |
| [10] | Ratanawijitrasin S, Soumerai SB, Weerasuriya K.D, National medicinal drug policies and essential drug programs improve drug use? A review of experiences in developing countries. Soc Sci Med, 2001; 53:831-44. |
| [11] | Loyola Filho AI, Uchôa E, Guerra HL, Firmus JOA, Lima-Costa MF, Prevalence and factors associated with self-medication: results of Bamburgh project, Rev Public Health 2002; 36:55-62. |
| [12] | Bertoldi AD, Barros AJD, Hallal PC, Lima RC, Use of medicines in adults: prevalence and individual determinants, Rev Public Health 2004; 38:228-38. |
| [13] | Arrais PSP, Brito LL, ML Barreto, HLL Coelho, Prevalence and determinants of medicines consumption in Fortaleza, Ceará, Brazil. Cad Public Health 2005; 21:1737-46. |
| [14] | Barros MBA, Health household surveys: potentials and challenges. Rev Bras Epidemiol 2008; 11 Suppl 1:6-19. |
| [15] | Rozenfeld S, Valente J, Studies of drug use - technical considerations for collecting and analyzing data, Health Serv Epidemiol 2004; 13:115-23. |
| [16] | Bertoldi AD, Barros AJD, Wagner, Rooss-Degnan D, Hallal PC, A descriptive review of the methodologies used in household surveys on medicine utilization, BMC Health Serv Res 2008; 8:222. |
| [17] | Paniz VMV, Fassa AG, Facchini LA, Bertoldi AD, Piccini RX, Tomasi, Access to medicines in continuous use in adults and elderly in the South and Northeast regions of Brazil, Cad Public Health 2008; 24:267-80. |
| [18] | Ribeiro AQ, Rozenfeld S, Klein CH, CC Cesar, Acurcio FA, Survey on the use of medicines by elderly retirees, Belo Horizonte, MG. Rev Public Health 2008; 42:724-32. |
| [19] | Castro SS, Pellicioni AF, Cesar CLG, Carandina L, Barros MBA, Alvez MCGP, Drug use by people with disabilities in areas of São Paulo. Rev Public Health 2010; 44:601-10. |
| [20] | http://www.lonelyplanet.com/bangladesh/practical-information/health accessed on 13th October, 2014. |
| [21] | M Babu, Factors contributing to the purchase of Over The Counter (OTC) drugs in Bangladesh: An Empirical study, The Internet Journal of Third World Medicine. 2007 Volume 6 Number 2. |
| [22] | López J, González M. Utilización de medicamentos por estudiantes de farmacia de la Universidad de Granada. Farm Clin 1997; 14:90-7. |
| [23] | Cabrita J, Ferreira HS, Iglesias P, Baptista TM, Rocha E, Silva LAl, Study of drug utilization among students at Lisbon University in Portugal. Pharmacoepidemiol Drug Saf, 2002; 11:333-4. |
| [24] | Marques-Vidal P, Medicine usage and handling in a sample of Portuguese students. Revista da Faculdade de Medicina de Lisboa 2005; 10:279-84. |
| [25] | Acocella CM, Using diaries to assess nonprescription drug use among university students. J Drug Educ, 2005; 35:267-74. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML