-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2014; 4(6): 283-286
doi:10.5923/j.ajmms.20140406.15

Study of Serum Hepcidin, Iron and Ferritin in Chronic Hepatitis C Patients
Fatma Saffeyeldin Mohamed1, Mirhan M. Elkady2, Mona El-Fedawy El-Saied3, Wael F. Sedik4, Aml El-sayed Abdou Yehia5
1Department of Tropical Medicine, Faculty of Medicine (for girls), Al-Azhar University, Cairo, Egypt
2Department of Clinical Pathology, Faculty of Medicine (for girls), Al-Azhar University, Cairo, Egypt
3Department of Internal Medicine, Faculty of Medicine (for girls), Al-Azhar University, Cairo, Egypt
4Department of Medical Biochemistry, Faculty of Medicine, Minia University, Egypt
5Department of Microbiology and Immunology, Faculty of Medicine (for girls), Al-Azhar University, Cairo, Egypt
Correspondence to: Fatma Saffeyeldin Mohamed, Department of Tropical Medicine, Faculty of Medicine (for girls), Al-Azhar University, Cairo, Egypt.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Chronic hepatitis C (CHC) is often associated with increased serum iron and ferritin which may cause more liver damage and rapid progression to cirrhosis and hepatocellular carcinoma. Hepcidin, a hepatic hormone which inhibits iron absorption, is considered the main regulator of iron metabolism. Reduced serum hepcidin in CHC patients is thought to be the main cause of these changes. Aim: The aim of this study was to assess changes in serum hepcidin, ferritin and iron in chronic HCV patients. Subjects and Methods: Serum hepcidin, ferritin and iron were studied in 45 patients with CHC and 25 healthy controls. Results and Conclusions: Serum hepcidin was significantly lower while serum iron and ferritin were significantly higher in CHC patients than controls.
Keywords: Chronic hepatitis C (CHC), Hepcidin, Ferritin, Iron
Cite this paper: Fatma Saffeyeldin Mohamed, Mirhan M. Elkady, Mona El-Fedawy El-Saied, Wael F. Sedik, Aml El-sayed Abdou Yehia, Study of Serum Hepcidin, Iron and Ferritin in Chronic Hepatitis C Patients, American Journal of Medicine and Medical Sciences, Vol. 4 No. 6, 2014, pp. 283-286. doi: 10.5923/j.ajmms.20140406.15.
Article Outline
1. Introduction
- Hepatitis C virus infection is one of the main causes of chronic liver disease worldwide [1]. Hepatitis C viral infection affects more than 200 million people worldwide, but most of them have no idea about their infection or of their ensuing hepatic disease [2].The long-term hepatic impact of HCV infection is highly variable from minimal changes to chronic hepatitis, cirrhosis and hepatocellular carcinoma [3]. Patients with CHC frequently develop mild to moderate iron overload [4].Many experimental and clinical studies, though not all, suggest that excessive iron in CHC is a cofactor promoting the progression of liver damage and increasing the risk of fibrosis, cirrhosis, and HCC [5, 6]. Hepatic iron concentration has been inversely associated with the response to antiviral therapy [7, 8].Chronic hepatitis C often appears to be associated with disturbances in iron homeostasis, with elevated serum ferritin and hepatic iron stores in approximately 50% of patients [9]. However, little is known about the mechanism of excess iron accumulation during chronic HCV infection [10].The importance of iron as a co-morbid factor in CHC is emphasized by several reports of greater fibrosis, and greater risks of HCC development with more hepatic iron [11]. Conversely, iron reduction has consistently been associated with reductions in serum ALT levels, severity of hepatic necro-inflammation, and risk of development of HCC. Iron reduction has also led to improved responses to IFN-based therapy of CHC [7].Many hypotheses explained the accumulation of iron in CHC, by the local release of iron from necrotic hepatocytes and HCV-induced perturbation of liver iron homeostasis [12].With the discovery of hepcidin, the liver has emerged as the central organ in the regulation of systemic iron homeostasis [12]. Hepcidin is a 25-aminoacid peptide hormone primarily synthesized by hepatocytes and it negatively controls two critical steps of iron homeostasis: duodenal absorption and the release from macrophages [13, 14].At the molecular level, hepcidin binds to ferroportin, the membrane iron exporter highly expressed by enterocytes and macrophages [10]. This results in ferroportin internalization and degradation and hence reduction of iron entry in the plasma compartment [14].Hepcidin expression is modulated by iron stores, so that it decreases in iron deficiency to facilitate iron absorption while it increases in iron repletion to prevent pathological overload. Hepcidin expression is also induced by inflammation and suppressed by hypoxia and anemia [15, 16].Disruption of hepcidin regulation has been postulated as a possible mechanism causing iron overload in acquired conditions, including alcoholic liver disease and CHC [8]. Studies in animal and cellular models have suggested that HCV infection may directly modulate hepcidin expression by HCV-induced reactive oxygen species (ROS) [17].
2. Subjects and Methods
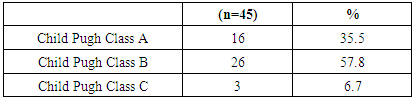
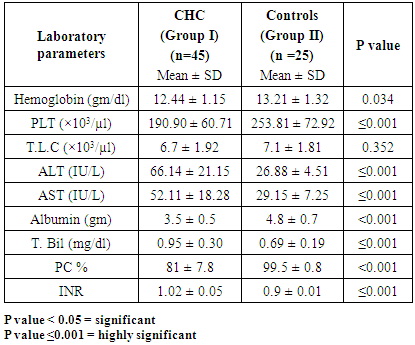
- This study was carried out on 45 chronic HCV patients selected from Internal and Tropical Medicine Departments Clinics and inpatients at Alzhraa University Hospital, Al-Azhar University, Cairo, Egypt and 25 healthy volunteers as controls.Patients with severe anemia or other causes of chronic liver disease (CLD) were excluded from the study.Participants were classified into two groups: • Group I: included 45 patients with chronic HCV infection. • Group II: Included 25 healthy controls.All participants were subjected to full history taking; thorough clinical examination; abdominal ultrasound and the following laboratory tests liver function tests (total/direct bilirubin, alanine aminotransferase (ALT), aspartate aminotransferase (AST), total proteins, and albumin), prothrombin time (PT), INR, complete blood count (CBC), Serum iron, transferrin saturation and ferritin. Also; HCVab & PCR, HBsAg & HBcAb were done.Assessment of serum hepcidin: blood samples were collected from each participant by venipuncture in empty centrifuge tubes: incubated in water bath at 37°C for 15 minutes then centrifuged at 3500 rpm. Sera were separated and stored at – 80°C until measurements of serum hepcidin levels. The quantitative detection of commercially available Human Hepcidin (Hepc) ELISA Kit was performed. The quantitative sandwich enzyme immunoassay technique provided by AMS Biotechnology (Europe) Ltd, UK. Catalogue Number: E01H0051, according to the manufacturer’s instructions. Informed oral consent was obtained from all participants before starting the study.Statistical Analysis: Data were expressed as mean±SD and percentages. Continuous variables were compared between the two groups with Student’s “t” test. Categorical variables were compared by X2 test, and the Fisher exact test when appropriate. One-sided analysis of variance (ANOVA) was used to assess differences among the two studied groups. P-value of less than 0.05 was considered significant. Data analysis was performed with the SPSS Statistical Package, version 20.
3. Results
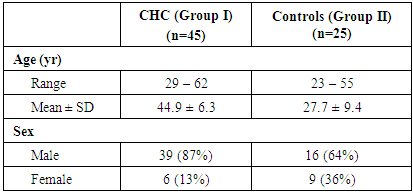
- Patients with CHC(Group I) included 39 males and 6 females while Group II included 16 males and 9 females as controls, their mean ages were 44.9 ± 6.3 in Group I and 27.7 ± 9.4 in Group II (Table 1).
|
|
|
|
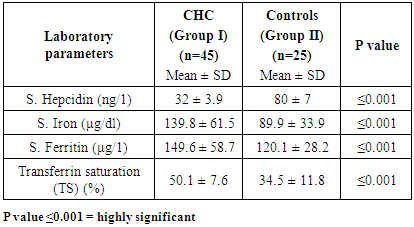
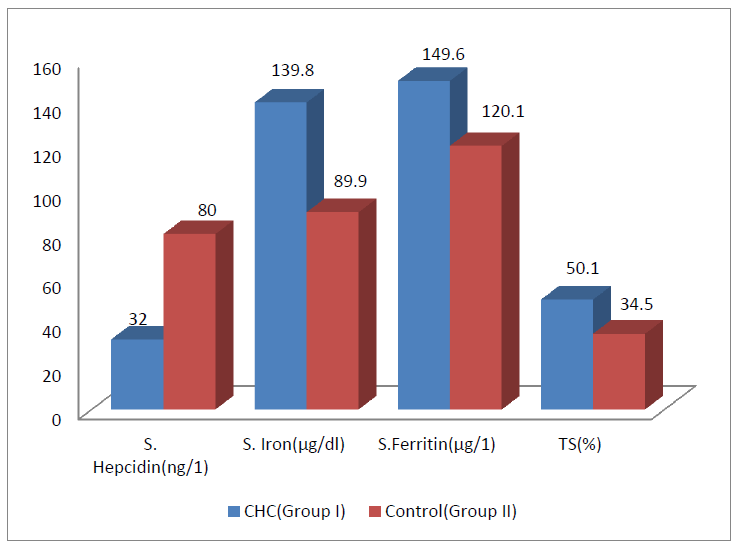 | Figure (1). Hepcidin and iron, ferritin and transferrin saturation in CHC patients and control group |
4. Discussion
- The hepatic hormone hepcidin is the major regulator of iron metabolism which inhibits iron absorption and recycling from erythrophagocytosis [19].Patients with CHC often have increased iron, a condition associated with reduced response to antiviral therapy, more rapid progression to cirrhosis, and development of hepatocellular carcinoma [20, 21].This study demonstrated that hepcidin level was significantly lower in Chronic HCV patients than controls. This goes in agreement with Guo et al. [11] and Lange et al. [22] they speculated that hepcidin expression in HCV is determined by the opposing effects of hepcidin-suppressive viral factors and the hepcidin stimulation by iron load.Low level of hepcidin leads to iron overload leading to inflammation and liver fibrosis [21]. However, our results were not in agreement with Fujita et al. [23] who found that hepcidin levels did not differ significantly from those in healthy controls, likely because of both methodological imprecision and the very low number of controls enrolled.Serum iron, ferritin and transferrin saturation were significantly higher in CHC patients compared to the control group and these findings were in agreement with Hörl and Schmidt [21] who found a strong correlation between serum hepcidin, serum ferritin, transferrin and iron levels.Our findings were also in agreement with Deicher and Hörl [24] who performed a comprehensive analysis of the role of serum ferritin and its genetic determinants in the pathogenesis and treatment of CHC and stated that elevated serum ferritin levels may reflect a systemic inflammatory state as well as increased iron storage, both of which may contribute to an unfavorable outcome of chronic hepatitis C (CHC).As regards levels of hepcidin, serum iron and ferritin, our results were also in agreement with Girelli et al. [25] who demonstrated that CHC hepcidin concentrations were significantly lower than those of controls. Hepcidin down regulation is associated with iron accumulation and increased serum ferritin. Also, our results were in agreement with Vagu et al. [26] who found that, Patients with chronic hepatitis C (CHC) often have elevated serum iron markers, which may worsen liver injury.
5. Conclusions
- Serum hepcidin level in patients with HCV was significantly lower compared to controls. The consequences of this dysregulation of the hepcidin expression by CHC is an important mechanism in increased iron load in those patients and this may have significant implications for the management of chronic HCV infection. Improvement for hepcidin regulation may be beneficial for HCV patients with iron overload. Further studies and also follow up of CHC patients are needed to refine on hepcidin regulation in the full clinical spectrum of HCV.
6. Recommendations
- Further studies are recommended to understand hepcidin’s molecular control and to determine if supplementation of hepcidin is beneficial in CHC patients. Studies also should be carried out on the role of iron depletion in the treatment of hepatitis C in patients with raised iron concentration.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML