-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2014; 4(6): 250-255
doi:10.5923/j.ajmms.20140406.10
Clinical Use of ACE Inhibitors
Levinra V. Vijiakumar
Faculty of Medicine, Universitas Udayana, Denpasar, Bali, Indonesia
Correspondence to: Levinra V. Vijiakumar, Faculty of Medicine, Universitas Udayana, Denpasar, Bali, Indonesia.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
This paper is to acknowledge hypertension as a leading cause of death in the world today. This condition is often called as a ‘”silent killer” because its symptoms can go undetected or untreated until damage to the body has occurred. Infact, if it is left uncontrolled, it can raise the risk of dementia, heart attack, heart failure, kidney failure, stroke, and vision loss. There are several other classes which are commonly used in treating hypertension which includes ACE inhibitors, diuretics, angiotensin-receptor blockers, beta-blockers and calcium-channel blockers. However, ACE (angiotensin-converting enzyme) inhibitors are used by millions of people every day as it is most prescribed and preferred by doctors today. ACE inhibitors are also widely used to treat other medical conditions such as after a heart attack (in the absence of heart failure) and people with diabetes with or without kidney disease. ACE inhibitors can be used in combination with two or more drugs from different classes at a time. Indeed, many people with high blood pressure will require two or more drugs to bring their blood pressure down to a normal level.
Keywords: Hypertension, ACE inhibitors, Heart failure
Cite this paper: Levinra V. Vijiakumar, Clinical Use of ACE Inhibitors, American Journal of Medicine and Medical Sciences, Vol. 4 No. 6, 2014, pp. 250-255. doi: 10.5923/j.ajmms.20140406.10.
Article Outline
1. Introduction
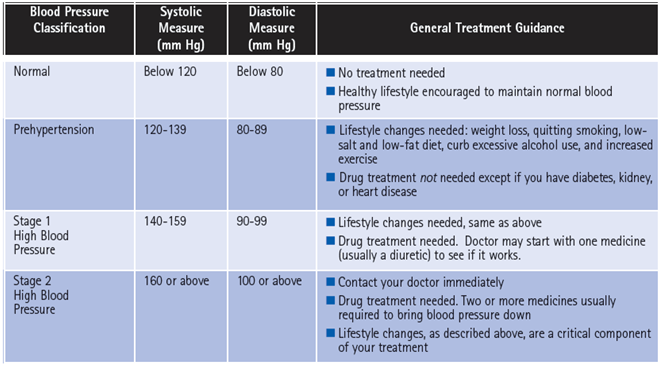
- High blood pressure or hypertension is a leading cause of death in the world today [1]. This condition is often called a ‘”silent killer” because its symptoms can go undetected until damage to the body has occurred [1]. Because of this, it is one of the most significantly under-diagnosed and under-treated medical conditions [1]. If left uncontrolled, it can raise the risk of dementia, heart attack, heart failure, kidney failure, stroke, and vision loss [1]. It is estimated that hypertension causes 4.5% of current global disease burden in both developing and developed countries [1]. Today hypertension-induced cardiovascular risk continue to rise globally as cardiovascular disease contributes to one-third of global mortalities (7.1 million premature deaths) and is a leading and increasing contributor to the global disease burden [1].The ACE inhibitor has been used for the therapy of cardiovascular diseases since it was discovered in the late 1970s and has been extensively studied and researched ever since [2, 6]. The ACE inhibitor was first discovered by scientists by exploring the role of the renin-angiotensin system (RAS) based on clinical settings and animal experiments [2, 6]. This has sparked interest based on the renin-angiotensin system (RAS) in other diseases as well [2]. Since excess angiontensin II affects the systemic blood pressure, coronary and renal circulation, in long term it induces myocardial and renal tubular necrosis [2, 3, 6]. Therefore, there is a need for drugs that could interfere with angiotensin II activities [2, 3]. Over time, it was then established that by suppressing the angiotensin II release by inhibiting ACE is an effective treatment for hypertension and heart failure [2, 3]. They also reduced morbidity and mortality only by lowering high blood pressure [2, 3].Patients with high or uncontrolled hypertension have significant risk of complications such as coronary artery disease, cerebrovascular disease, hypertensive retinopathy, chronic kidney disease, and cardiovascular disease [2, 4, 12]. Hence, it is important to treat hypertension to prevent future complications [1, 4, 12]. The use of ACE inhibitors plays an important role in the treatment of heart failure as it improves the cardiovascular system and reduces the progression of the disease and ultimately death itself [1, 2, 12]. In the aspect of health care system, this could prove to be beneficial as ACE inhibitors improves the outcome and duration of life in heart failure patients and in long term reduces health costs [2].However, as more extensive studies and experiments being performed to explore the benefits and areas to be improved of an ACE inhibitors it is clear that innovative new classes of drugs will be discovered to lend a helping hand in many areas of medicine [2, 6]. This opportunity is encouraged in an area such as heart failure where the condition is widespread and its morbidity and mortality rates are increasing worldwide [2, 6].
2. Literature Review
2.1. Clinical Indication of ACE Inhibitors
- An ACE inhibitor is a drug used primarily to treat hypertension and congestive heart failure [1, 5, 11]. ACE inhibitors functions by inhibiting angiotensin-converting enzyme, a component of the blood pressure-regulating renin-angiotensin system [5, 6]. This component decreases the tension of blood vessels and blood volume, finally reducing blood pressure [5, 6]. Currently most commonly used ACE inhibitors are perindopril, captopril, enalapril, lisinopril, and ramipril [5, 6]. ACE inhibitors are used primarily to treat hypertension, although they may also be prescribed for cardiac failure, diabetic nephropathy, chronic renal failure, renal involvement in systemic sclerosis, left ventricular systolic dysfunction and acute myocardial infarction [5, 6, 12].The function of an angiotensin-converting enzyme (ACE) inhibitor is to reduce the activity of the renin-angiotensin-aldosterone system [5, 6]. One of the mechanism is to maintain the blood pressure by releasing renin (a type of protein) from cells in the kidney [5, 6]. The secretion of renin produces another protein called angiotensin which signals the adrenal gland to produce a hormone called aldosterone [5, 6]. When there is a drop in blood pressure (hypotension), the body compensates by activating this system in response to overcome hypotension [5, 11]. This system is also activated when there is a problem with the salt-water balance of the body, such as decreased sodium concentration in the distal tubule of the kidney [6, 12]. Besides that, the body also requires this system to overcome conditions such as decreased blood volume and when there is stimulation of the kidney by the sympathetic nervous system [5, 6]. When these situations occur, the kidneys release renin, which acts as an enzyme and cuts off all but the first 10 amino acid residues of angiotensinogen (a protein made in the liver that circulates in the blood) [5, 6]. These 10 residues are then known as angiotensin I. Angiotensin converting enzyme (ACE) then removes a further two residues which converts angiotensin I into angiotensin II [5, 6].Angiotensin II is found in the pulmonary circulation, as well as in the endothelium of many blood vessels [6, 13]. The system in general aims to increase blood pressure by increasing the amount of salt and water the body retains although angiotensin also function to constrict blood vessels (a potent vasoconstrictor) [6, 13].ACE inhibitor inhibits the conversion of angiotensin I to angiotensin II [6, 12]. Therefore, the arteriolar resistance is lowered and the venous capacity is increased [6, 12]. This causes an increase in cardiac output, cardiac index, stroke work, and volume, thus lowering the renovascular resistance and leads to an increased natriuresis (excretion of sodium in the urine) [6, 13]. Concentration of renin will increase in the blood due to negative feedback of conversion of angiotensin I to angiotensin II [6, 12]. Therefore angiotensin I will increase in concentration as angiotensin II will decrease [6, 12]. This causes aldosterone to decrease which reduces sodium reabsorption [6, 12]. Bradykinin will also increase due to less inactivation that is done by ACE (angiotensin-converting enzyme) [6].
|
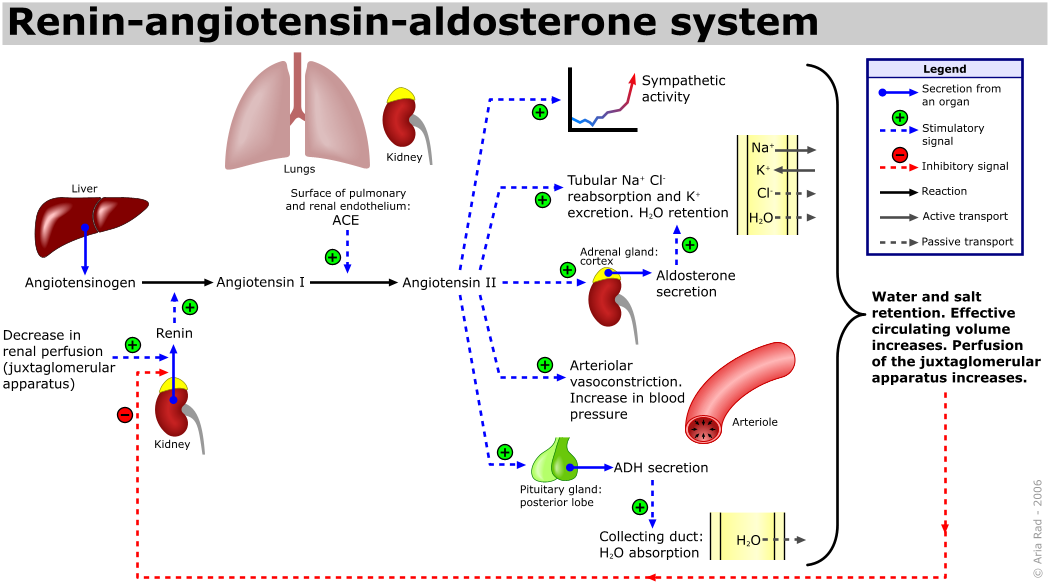 | Figure 1. Role of renin-angiotensin-aldosterone system (Rad 2006) |
2.2. Adverse Effects
- Every drugs has its benefits and its shortcomings. The same concept implies with ACE inhibitors [6]. It is common to encounter drug reactions such as hypotension, high potassium concentration (hyperkalemia), headache, dizziness, fatique, nausea, and renal impairments in patient on ACE inhibitors therapy [5, 6, 11]. ACE inhibitors may also elevate pain related to inflammation. This condition is caused by the accumulation of bradykinin that occurs after ACE is inhibited [5]. One of the most common symptoms encountered in patients on ACE inhibitors therapy is a persistent dry cough [5, 6]. This is due to the increase in bradykinin levels caused by the ACE inhibitors [5, 6]. Patients with these complaints are then switched to angiotensin II receptor antagonists (ARB) to reduce or even eliminate this symptom [6, 7]. In rare cases such as rash and taste disturbances have been reported in patients on ACE inhibitors therapy [5, 6]. This condition is believed to have occurred more prevalent with the use of captopril and it is associated to its sulfhydryl moiety. This has led to a decreased use of captopril in clinical settings, although it is still preferred in several procedures such as scintigraphy of the kidney. Another significant adverse effect of all ACE inhibitors is the renal impairment [6, 11]. This is caused by the effect on angiotensin II-mediated homeostatic functions, such as renal blood flow [6, 11]. Renal blood flow may be affected by angiotensin II due to its vasoconstriction properties at the efferent arterioles of the glomeruli of the kidney, thereby increasing the glomerular filtration rate (GFR) [6]. Hence, by reducing angiotensin II levels, ACE inhibitors may reduce GFR, a marker of renal function [6]. To be specific, they can induce or exacerbate renal impairment in patients with renal artery stenosis [6]. This is especially a problem if the patient is taking an NSAID and a diuretic at the same time [6]. When the three drugs are taken together, there is a very high risk of developing renal failure [6]. ACE inhibitors may also cause hyperkalemia [6]. A patient that consumes ACE inhibitors leads to suppression of angiotensin II which then leads to a decrease in aldosterone levels [6]. Since aldosterone is responsible for the excretion of potassium, ACE inhibitors could indirectly cause retention of potassium which leads to hyperkalemia [6, 11]. A severe allergic reaction also can take place that affects the bowel wall and secondarily cause abdominal pain [6]. This anaphylactic reaction however is very rare [6]. Some patients could develop angioedema due to increased bradykinin levels [6]. There appears to be a genetic predisposition toward this adverse effect in patients who degrade bradykinin more slowly than average [6]. In pregnant women, consumption of ACE inhibitors during the first trimester can cause major congenital malformations, stillbirths, and neonatal deaths [6, 8]. Fetal abnormalities that could occur includes hypotension, renal dysplasia, anuria/oliguria, oligohydramnios, intrauterine growth retardation, pulmonary hypoplasia, patent ductus arteriosus, and incomplete ossification of the skull [6, 8]. Overall, about half of newborns exposed to ACE inhibitors are adversely affected and present with risk with birth defects [8].
2.3. Contraindications and Precautions
- The ACE inhibitors are contraindicated in patients with previous history of angioedema, renal artery stenosis or hypersensitivity to ACE inhibitors [6].ACE inhibitors should also be avoided in women who are likely to become pregnant [5, 6, 8]. In many countries, ACE inhibitors are labelled with a warning concerning the risk of birth defects when taken during the second and third trimester [5, 8]. Potassium supplementation could be given to patients due to the hyperkalemic effect of ACE inhibitors however it should be used with caution and under medical supervision [6]. Drug interactions should also be carefully monitored to avoid unwanted adverse effects [6].
2.4. Therapuetic Recommendations
- All ACE inhibitors have similar antihypertensive efficacy when equivalent doses are administered [5, 6]. The main focus should be given on the differences in all ACE inhibitors especially with captopril, the first ACE inhibitor [5]. Captopril has a shorter duration of action and an increased incidence of adverse effects [4]. Captopril is also the only ACE inhibitor which is capable of passing through the blood–brain barrier, although the significance of this characteristic has not been shown to have any positive clinical effects [4]. One of the agents in the ACE inhibitor class, ramipril has the ability to reduce the mortality rates of patients who suffered a myocardial infarction, and to slow the subsequent development of heart failure [4, 10]. Ramipril's additional benefits may be shared by some or all drugs in the ACE inhibitor class [4, 10]. However, ramipril currently remains the only ACE inhibitor for which such effects are actually evidence-based [4, 10].
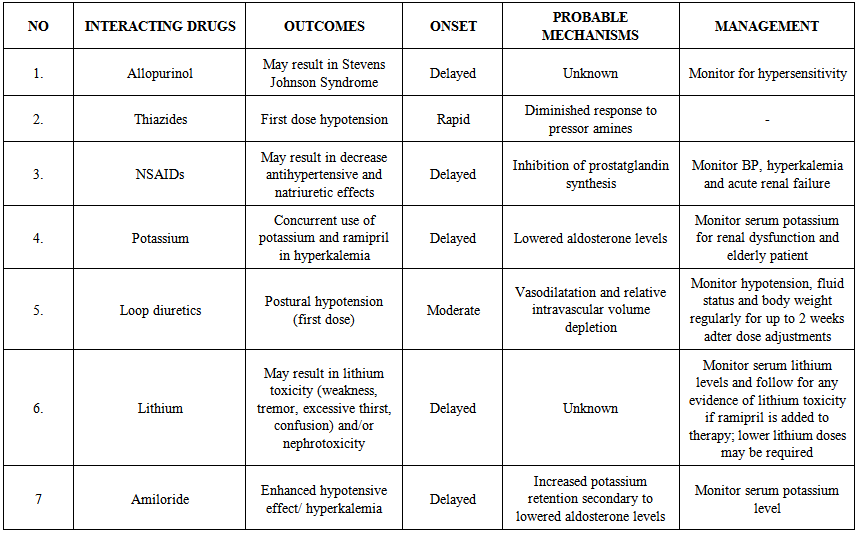 | Table 2. Clinically significant drug interactions of ACE inhibitors (Prabhu 2005) |
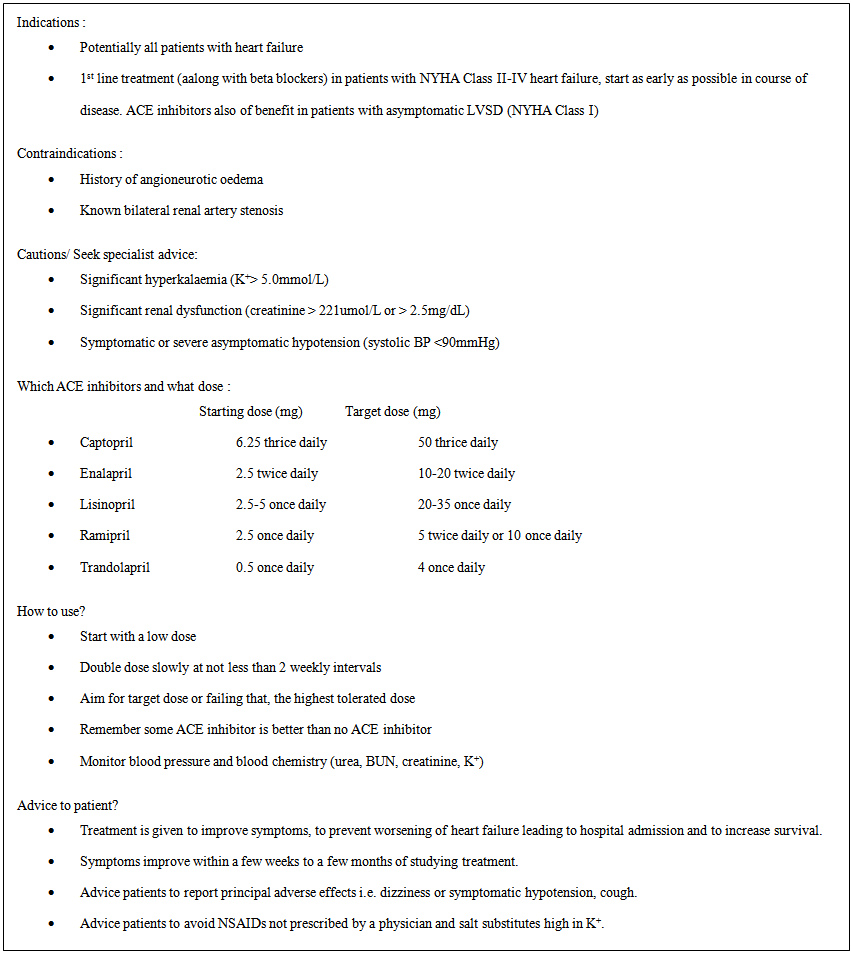 | Table 3. Practical guidance on the use of ACE inhibitors (McMurray, 2005) |
3. Conclusions
- After discussing the points of view, it has been concluded that an ACE inhibitor is a pharmaceutical drug used primarily for the treatment of hypertension and congestive heart failure. Angiotensin-converting enzyme inhibitor plays an important role in reducing the activity of the renin-angiotensin-aldosterone system hence lowering the blood pressure. A persistent dry cough is a relatively common adverse effect that is believed to be associated with the increases in bradykinin levels produced by ACE inhibitors. However, patients who experience this cough are often switched to angiotensin II receptor antagonists. Each ACE inhibitors have its own strengths with different starting dosages. Therefore, it is important to educate patients about the adverse effect of the prescribed drug and consult them to regularly check their blood pressure to monitor if there is any improvement or worsening of symptoms. Hence, the dosage should be adjusted according to the clinical response that is experienced by the patients.
ACKNOWLEDGEMENTS
- First of all, I would like to show my gratitude to the Lord because with his blessings I have managed to complete my paper entitled "Clinical Use of ACE Inhibitors”.With pleasure, I, Levinra V. Vijiakumar, would like to convey my heartiest thank you to Dr. Ida Ayu Ika Wahyuniari, M. Kes, the supervisor for my paper work whose encouragement, guidance, and support from the initial to the final level enabled me to develop an understanding of the topic and successfully complete my paper work. Last but not least I hope that my writing would be beneficial to the readers as how it was for me.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML