-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2014; 4(4): 123-125
doi:10.5923/j.ajmms.20140404.04
Abdominal Aortic Graft Causing Recurrent Aortoduodenal Fistula as a Rare Cause of Gastrointestinal Bleeding: Case Report
Renelus Benjamin, Axiyan Maihemuti, Flood Michael
Morehouse School of Medicine, Internal Medicine Department, Division of Gastroenterology. Atlanta, GA. 30310
Correspondence to: Renelus Benjamin, Morehouse School of Medicine, Internal Medicine Department, Division of Gastroenterology. Atlanta, GA. 30310.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Background: Aortoenteric fistula( AEF) is a rare and deadly vascular complication usually secondary to aortic aneurysmal graft repair causing massive bleeding. Recurrent AEF, years after the initial repair, is an even rarer occurrence. Case presentation: We present a case of a 58 year old male with history of abdominal aortic aneurysm, who was brought to the emergency department (ED) after being found unresponsive with a visual approximation by EMT of 500ml of bright red blood per rectum. Unlike many previous case reports our patient’s recurrent fistula occurred years after second repair in 2012. Conclusions: Although rare, abdominal aortic aneurysm (AAA) repair can form enteric fistula causing massive bleeding which is a medical emergency. Patient can present with hemodynamic instability. Urgent vascular imaging and repair is necessary for the management.
Keywords: Abdominal aorticgraft, Aortoenteric fistula, Aortoduodenal fistula, Gastrointestinal bleed
Cite this paper: Renelus Benjamin, Axiyan Maihemuti, Flood Michael, Abdominal Aortic Graft Causing Recurrent Aortoduodenal Fistula as a Rare Cause of Gastrointestinal Bleeding: Case Report, American Journal of Medicine and Medical Sciences, Vol. 4 No. 4, 2014, pp. 123-125. doi: 10.5923/j.ajmms.20140404.04.
1. Introduction
- Aortoenteric fistula (AEF) arises when there is a direct communication between the aorta and GI tract that can lead to significant amount of bleeding [1]. AEF are rare but maintain a high clinical burden with mortality rate of 30% if recognized and treated early, and imminent death if unrecognized [2]. AEF are categorized as either primary or secondary. Secondary aortoenteric fistula (SAEF) can be rare complications of AAA repair (table 1). Reoccurrences are even rarer, usually befalling within a few months of the initial repair [2]. We present a case of recurrent SAEF two years after its initial occurrence repair.
2. Case
- A 58 year old male is brought to the ER after being found unresponsive with a visual approximation by first responders of 500ml of bright red blood per rectum. Medical history is significant for atherosclerotic infrarenal AAA with graft repair in 1997, and subsequent SAEF repair in 2012 with 16mm, antibiotic-soaked Dacron patch. Patient was subsequently lost to follow up after the procedure. Upon arrival to the emergency department the patient was non responsive. Vitals showed hemodynamic instability with tachycardia to 140s and systolic blood pressure in 70s. He had a well healed midline scar without pulsatile mass. Hematochezia was present during rectal examination. While being stabilized in the emergency department, the patient’s hemoglobin was 7.1 g/dl, however, dropped acutely to 5.7 g/dl within 3 hours.Emergent IV access with two large bore IV catheters, endotracheal intubation and CTA with contrast was performed.CTA revealed retroperitoneal fat stranding surrounding the repaired aorta (Fig.1) along with enlarged significantly irregular infrarenalabdominal aortic aneurysmal sac (Fig 2) suggestive of aortic aneurysm leakage vs contained rupture. Patient was taken to the OR for emergent endoscopy and exploratory laparotomy. EGD and colonoscopy did not identify source of bleeding. Laparotomy revealed aortoduodenal fistula along with graft adhesions which were subsequently lysed. Repair of recurrent aortoduodenal fistula with explantation of infected graft, Oversewing of aortic stump and distal aorta, resection of distal duodenum, and temporary closure over open abdomen. Subsequent roux-en-Y duodenojejunostomy and placement of a feeding jejunostomy tube was done for the patient. He was admitted to the ICU post-operatively.
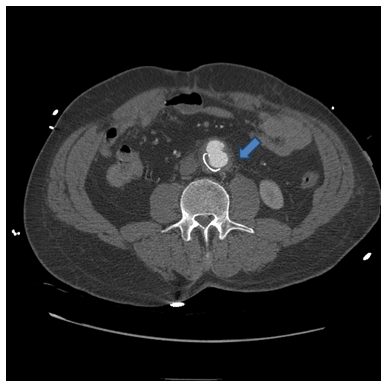 | Figure 1. Retroperitoneal fat stranding surrounding the repaired aorta with irregular outpouching |
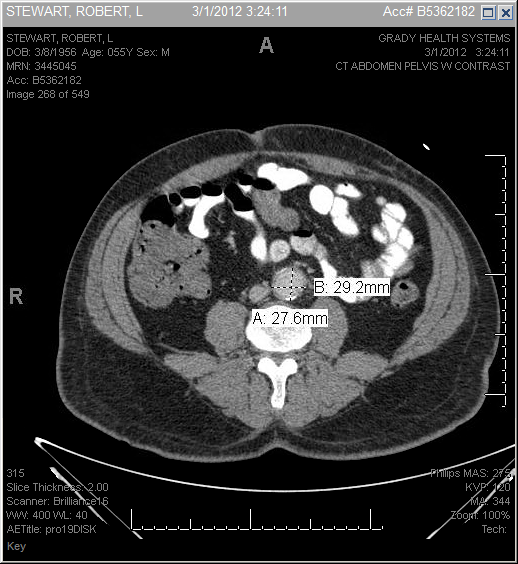 | Figure 2. Enlarged, irregular infrarenal abdominal aneurysmal sac |
3. Discussion
- SAEF occurs when there is an inappropriate communication between the aorta and adjacent GI tract causing massive bleeding. It is an infrequent but disastrous complication of open abdominal aortic repair. The incidence of SAEF after graft placement vary depending on the source, however all cite a range within 0.3-2.6% [3-4]. Recurrence of graft associated SAEF, as in our case, are exceptionally rare, with usual reoccurrences transpiring within 2-5 months [2]. SAEF is most prevalent form of fistula formation and usually stems from infected aortic graft eroding into the adjacent bowel causing significant bleeding [5]. Although rare, SAEFs are extremely deadly carrying a heavy mortality rate of 33% if caught early and treated with emergent surgery [2]. Imminent death occurs if undiagnosed and/or untreated. Collectively most primary and secondary AEF occur in the duodenum [6].Patients with SAEF may present with varied complaints. Most will present with complaint of abdominal or back pain, while others may have signs of infection including fever, leucocytosis, tachycardia [1]. The standard triad of abdominal pain, pulsatile abdomen and GI hemorrhage is seen <25% of the time [5]. While the majority of patients with SAEF present with symptoms of upper GI bleeding such as hematemesis, or melena, only 7% of patient’s with graft enteric fistula present with bright red blood per rectum [7] as seen in our patient.Prompt diagnosis is key to the management of SAEF. One should have a high suspicion of SAEF in patients with history of graft repair and significant bleeding. An emergent Esophagogastroduodenoscopy (EGD) should be done to identify possible location of bleeding (usually within the duodenum) [6]. If results of the EGD is inconclusive yet suspicion of SAEF remains high, contrast enhance CT angiography should be undertaken in order to identify inflammatory changes surrounding the aortic graft consistent with infection and fistula formation. Despite advancing diagnostic tools, timely diagnosis of SAEF continues to be a challenge among clinicians. With sensitivity of endoscopic studies such as colonoscopy and EGD being as low as 8% and 24% respectively [6]. Contrast-enhanced CT scan (confirmatory test for SAEF) carries a sensitivity rate of only 45% [6]. Given these limitations new studies are involving the use of virtual CT providing a 3 dimensional picture of the abdominal aorta [7-8].Treatment of SAEF includes emergent surgical repair of the graft and fistula as in our patient. There is limited data suggesting lower mortality in those who received additional surgical procedures with repair including debridement drainage and sac irrigation [10]. Despite treatment, prognosis for this condition is poor with over half of patients dying [8] (Table 1).
4. Conclusions
- SAEF is a rare yet deadly cause of GI bleed. Key to survival include early diagnosis and prompt surgery. Clinicians should consider SAEF in patients with history of graft placement who present with signs or symptoms of infection, or massive GI bleed. Early endoscopic studies are crucial to identifying source of bleeding, however given low diagnostic sensitivities, clinicians should not rely on these results alone. Advanced imaging with virtual CT provides promise in diagnosing this complex condition. Ultimate treatment involves vascular and general surgical repair.
ACKNOWLEDGEMENTS
- We would like to acknowledge Grady Memorial Hospital for providing unique cases to build upon medical knowledge.
References
| [1] | Hyett B.H., Saltzman J.R. 2012). Chapter 155. Upper Gastrointestinal Bleeding. n cKean S.C., Ross J.J., Dressler D.D., Brotman D.J., Ginsberg J.S. Eds), Principles and Practice of Hospital Medicine. J. Breckling, Ed., The Analysis of Directional Time Series: Applications to Wind Speed and Direction, ser. Lecture Notes in Statistics. Berlin, Germany: Springer, 1989, vol. 61. |
| [2] | Wong R., Pollack MJ. Recurrent aortoenteric fistula. Am J Gastroenterol 2007Jul; 02(7):1547-8. |
| [3] | Busuttil SJ, Goldstone J. Diagnosis and management of aorto-enteric fistulas. SeminVascSurg 2001;14:302–11. |
| [4] | Kuestner LM, Reilly LM, Jicha DL, Ehrenfeld WK, Goldstone J, Stoney RJ. Secondary aortoenteric fistula: contemporary outcome with use of extraanatomic bypass and infected graft excision. J VascSurg 1995;21:184–95. |
| [5] | Doney M., Vilke G., The Journal of Emergency Medicine. 2012; 43(3):431-34. |
| [6] | Lemos DW, Raffetto JD, Moore TC, Menzoian JO. Primary aortoduodenal fistula: A case report and review of the literature. J Vasc Surg. 2003;37:686–9. |
| [7] | Pipinos II, Carr JA, Haithcock BE, et al. Secondary aortoenteric fistula. Ann VascSurg 2000;14:688–96. |
| [8] | Yoshimoto K., Shiiya N., Onodera Y., Yasuda K J. Secondary aortoenteric fistula. J VascSurg. 2005; 2(4):805. |
| [9] | Le GrecaLatteri S, Scala V, Sofia M, Russello D. Recurrent aortoduodenal fistula. Ann VascSurg. 011 Apr; 2 (3): 86.e7-386. |
| [10] | Moulakakis KG, Sfyroeras GS, Mylonas SNJ et al. Outcome after Preservation of Infected Abdominal Aortic Endografts. EndovascTher. 2014 Jun;21(3):448-55. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML