-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2014; 4(4): 114-122
doi:10.5923/j.ajmms.20140404.03
Assessment of Lipoxin A4 and High Sensitivity c-reactive Protein in Patients with Bronchial Asthma with or without Gastro-eosophageal Reflux Disease
Mahmoud A. Moneim1, Adel A. El-Shennawy2, Ahmed H. Wahba2, Nasr H. Khalil3, Khalid El-Mola4, Mostafa A. Hawary4, Ahmed Fathi5, Khalid F. Said5
1Internal Medicine Department, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
2Chest Department, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
3Fellow of Chest Disease, Cairo, Egypt
4Tropical Medicine Department, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
5Clinical Pathology Department, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
Correspondence to: Mahmoud A. Moneim, Internal Medicine Department, Faculty of Medicine, Al-Azhar University, Cairo, Egypt.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Lipoxins are lipoxygenase interaction products of arachidonic acid metabolism have been identified in human subjects with many varieties of respiratory illness, it can been synthesized by nasal polyps and bronchial tissues. the aim of the current study to assess the value of lipoxin A4 (LxA4) and high sensitivity c-reactive protein (hsCRP) in patients with bronchial asthma with or without gastro-esophageal reflux disease (GERD). For this purpose, 60 patients suffered from different grades of bronchial asthma, classified into three groups, group 1, 20 patients with mild persistent asthma, group 2, 20 patients with moderate persistent, and group 3, 20 patients with severe persistent asthma phenotype. 10 healthy subjects was taken as a control group. The followings were done for all subjects, pulmonary function tests (FEV1, FVC and SVC), total leukocytic count and eosinophilic count, serum lipoxin A4, high-sensitivity c.reactive protein, and upper gastro-esophageal endoscopy (for patients group only). From this study, the serum LxA4 level showed a significant progressive decline from mild to severe asthma groups with mean values, 1.006 ± 0.061,0.677 ± 0.078 and 0.351 ± 0.075, (P>0.002), more-ever, there was a significant decrease in its values in patients with GERD when compared with those without. (P<0.002) while hs.CRP showed a negative correlation with LxA4 and positive correlation with eosinophilic count and percentage. in conclusion, defective LxA4 generation in patients with asthma may be determine the degree of its severity the reason for the asthmatic patients whose illness become more serious.
Keywords: Internal medicine, Lipoxin A4, hsCRP, Bronchial asthma, GERD
Cite this paper: Mahmoud A. Moneim, Adel A. El-Shennawy, Ahmed H. Wahba, Nasr H. Khalil, Khalid El-Mola, Mostafa A. Hawary, Ahmed Fathi, Khalid F. Said, Assessment of Lipoxin A4 and High Sensitivity c-reactive Protein in Patients with Bronchial Asthma with or without Gastro-eosophageal Reflux Disease, American Journal of Medicine and Medical Sciences, Vol. 4 No. 4, 2014, pp. 114-122. doi: 10.5923/j.ajmms.20140404.03.
1. Introduction
- Lipoxin A4 (LxA4) is an anti inflammatory mediator having protective action and a role in restoration of tissue homeostasis after inflammation.(1). It has a potent anti-inflammatory properties with cell type specific actions on leukocytes endothelia, and other stromal cells. (2).Also, it was detected in broncho-alveolar lavage ((BAL)) and in pleural fluid from patients with chronic inflammatory lung diseases. (3)The aim of the work was to assess the value of LxA4 in patients with bronchial asthma of different grades of severity with or without GERD, and to explore the association between LxA4 and hs.CRP in those patients.
2. Subjects and Methods
- In our study patients with bronchial asthma were classified according to GINA (4) guidelines into mild persistent (group 1), moderate (group 2) and severe persistent (group 3); 20 patients in each group. Patients were classified again according to the level of control, into controlled, partially controlled and uncontrolled 10 healthy subjects were taken as a control. Patients and control, were subjected to history taking, clinical examination with special stress on chest and gastrointestinal systems, routin laboratory investigations, as liver and renal functions, fasting and 2h. postprandial blood sugar, also, total leukocytic count, easinophilic count, serum lipoxin A4 level, and high sensitivity C.reactive protein, pulmonary function tests {forced expiratory volume, (FEV.) forced vital capacity (FVC), and slow vital capacity (SVC)}.Assay Principle for lipoxin A4:This is an ELISA for the quantitative analysis of LXA4 levels in biological fluid. This test kit operates on the basis of competition between the enzyme conjugate and the LXA4 in the sample for a limited number of antibody binding sites.The sample or standard solution is first added to the microplate. Next, the diluted enzyme conjugate is added and the mixture is shaken and incubated at room temperature for one hour. During the incubation, competition for binding sites is taking place. The plate is then washed removing all the unbound material. The bound enzyme conjugate is detected by the addition of substrate which generates an optimal color after 30 minutes. Quantitative test results may be obtained by measuring and comparing the absorbance reading of the wells of the samples against the standards with a microplate reader at 450nm or 650nm. The extent of color development is inversely proportional to the amount of LXA4 in the sample or standard. For example, the absence of LXA4 in the sample will result in a bright blue color, whereas the presence of LXA4 will result in decreased or no color development.Product Features and assay principle of hsCRP:The Diazyme High Sensitive C-Reactive Protein (hsCRP) Assay has a linear range of 0.20 - 20 mg/L that extends below the measurement range typical of most conventional CRP assay's. This lower range of measurement may include the evaluation of conditions thought to be associated with inflammation in otherwise healthy individuals.Assay PrincipleThe assay is based on a latex-enhanced turbidimetric immunoassay method. When an antigen-antibody reaction occurs between CRP in a sample and anti-CRP antibody which has been sensitized to latex particles, agglutination results. This agglutination is detected as an absorbance change (570 nm), with the magnitude of the change being proportional to the quantity of CRP in the sample. The actual concentration is then determined by interpolation from a calibration curve prepared from calibrators of known concentration.Intended useThe Diazyme High Sensitivity C-Reactive Protein (hsCRP) Assay is for the in vitro quantitative determination of C-reactive protein (CRP) in human serum and plasma on automated clinical chemistry analyzers. Measurement of CRP is of use for the detection and evaluation of inflammatory disorders and associated diseases, infection and tissue injury. For in vitro diagnostic use only (oxford biomedical research 2010 - 2014).Selection of patientsPatients with systemic diseases. as collagen diseases, liver diseases, renal diseases, cardiac diseases, infectious diseases and malignancies, were excluded. None of patients in this study was on regular steroids either systemic or inhaled (patients who were off steroid), only used as a reliever, beside the traditional treatment of bronchial asthma e.g bronchodilators.
3. Results
- 1) Weight: In the group of patients with mild bronchial asthma, weight ranged from 45 to 101 kgs (Mean ± SD: 77.63 ± 17.4). In the group of patients with moderate asthma, weight ranged from 53 to 99 kgs (Mean ± SD: 73.3 ± 14.65). In the group of patients with severe asthma, weight ranged from 52 to 135 kgs (Mean ± SD: 80.3 ± 20.88). In the group of normal subjects, weight ranged from 50 to 102 kgs (Mean ± SD: 78.4 ± 18.89).
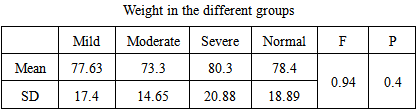 There was no significant difference between the four groups as regards the weight F = 0.94, P = 0.4.
There was no significant difference between the four groups as regards the weight F = 0.94, P = 0.4.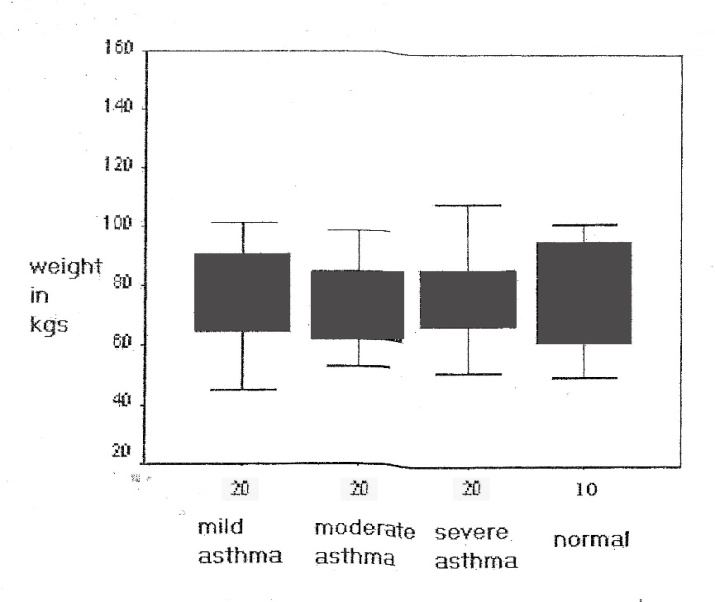 | Figure 1. Weight distribution in patients with bronchial asthma and normal subjects. there was insignificant difference between the four groups |
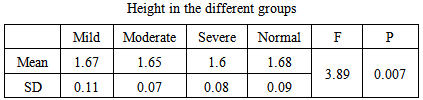 There was significant difference between the four groups as regards the Height F = 3.89, P = 0.007.
There was significant difference between the four groups as regards the Height F = 3.89, P = 0.007.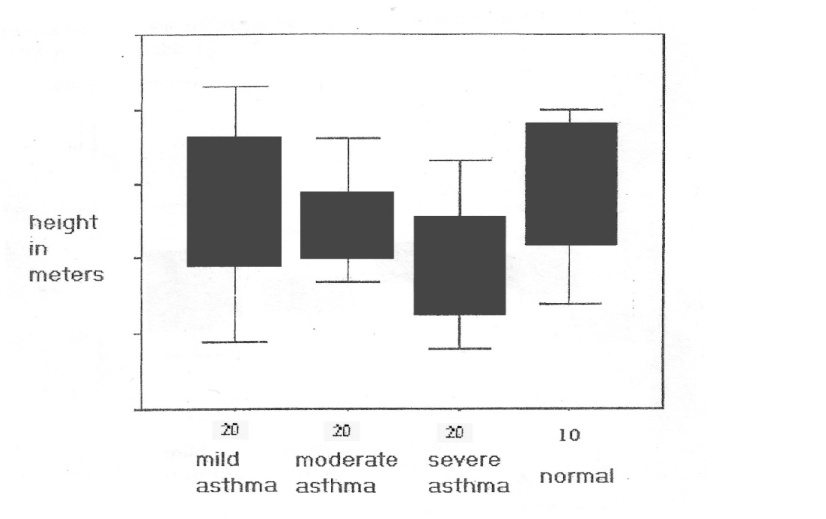 | Figure 2. Height distribution in patients with bronchial asthma and normal subjects |
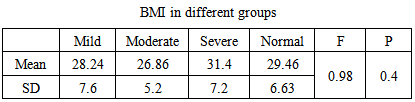 There was no significant difference between the four groups as regards BMI F = 0.98, P = 0.4.
There was no significant difference between the four groups as regards BMI F = 0.98, P = 0.4.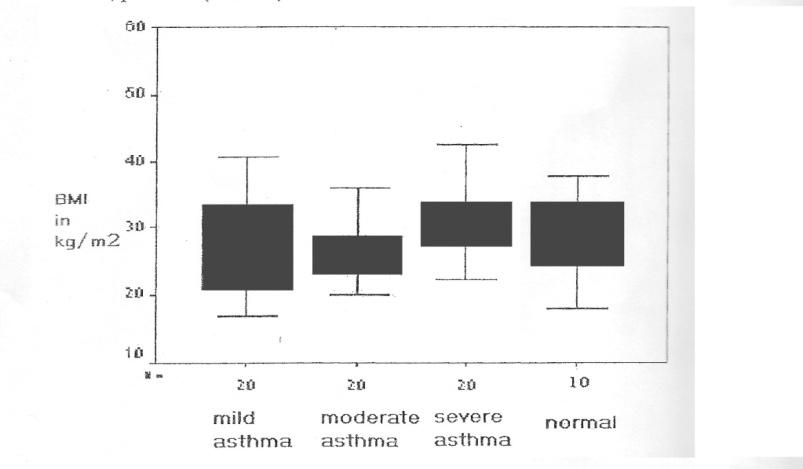 | Figure 3. BMI distribution in patients with bronchial asthma and normal subjects. there was insignificant difference between the four groups |
 v There was insignificant difference between the mean values of T.L.C. in the studies groups.
v There was insignificant difference between the mean values of T.L.C. in the studies groups. F = 0.74
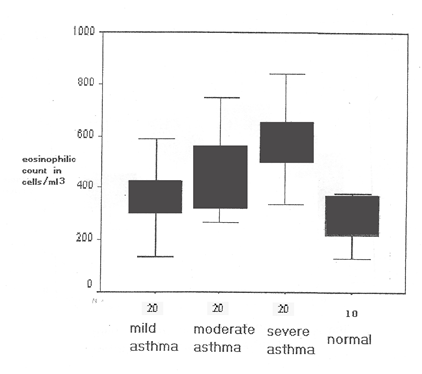
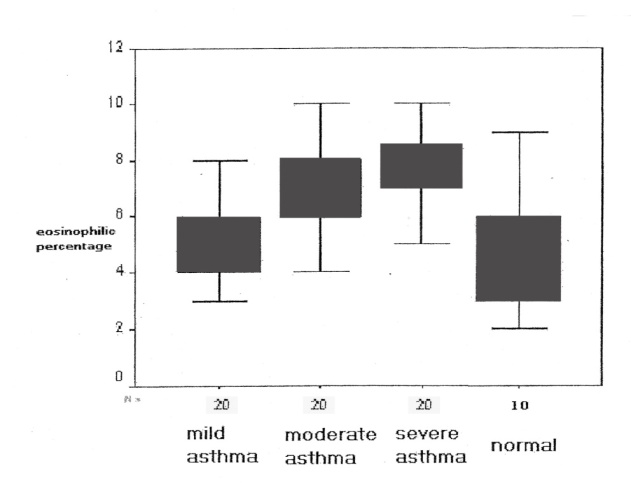
F = 0.74 P = 0.7 v While there was significant statistical difference between the mean values of the eosinophilic count in different groups, F = 6.58 P < 0.001.
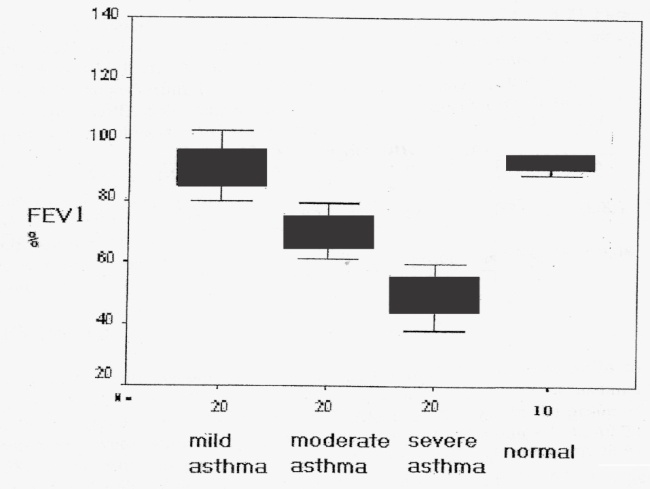
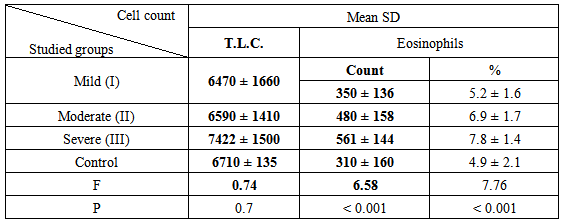
P = 0.7 v While there was significant statistical difference between the mean values of the eosinophilic count in different groups, F = 6.58 P < 0.001.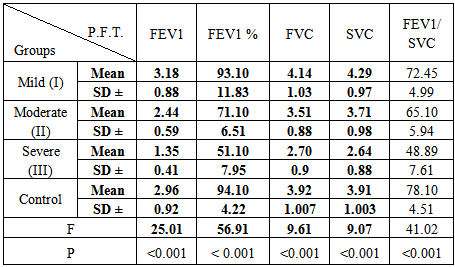 There were significant differences between the mean values of pulmonary function tests in the studied groups, where, FEV1: F = 25.01 and P < 0.001, FEV1 %: F = 56.91 and P < 0.001FVC: F = 9.61 and P < 0.001SVC: F = 9.07 and P < 0.001FEV1 / SVC: F = 41.02 P < 0.001
There were significant differences between the mean values of pulmonary function tests in the studied groups, where, FEV1: F = 25.01 and P < 0.001, FEV1 %: F = 56.91 and P < 0.001FVC: F = 9.61 and P < 0.001SVC: F = 9.07 and P < 0.001FEV1 / SVC: F = 41.02 P < 0.001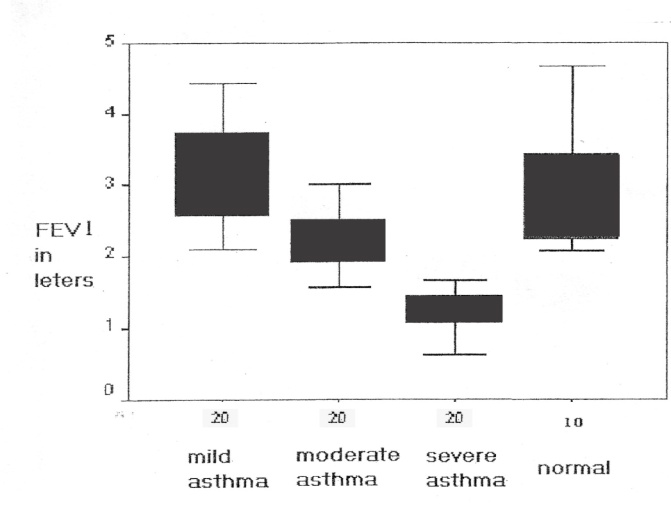 | Figure 6. Box plots showing the FEV1 in patients with bronchial asthma and normal subjects. There were significant differences between eosinophilic count in the four groups f = 25.01 p < 0.001 |
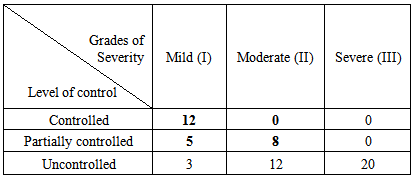 Distribution of patients in this study according to the level of control as GINA guidelines.7) The mean values of plasma lipoxin A4 levels (ng / ml) in studied groups:-
Distribution of patients in this study according to the level of control as GINA guidelines.7) The mean values of plasma lipoxin A4 levels (ng / ml) in studied groups:-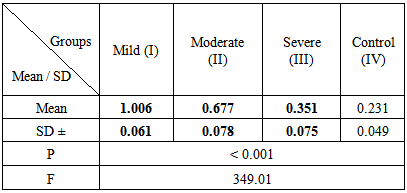 There was statistically significant progressive decrease in plasma LxA4 from mild to severe asthma groups.P < 0.001F = 349.018) Relation between LxA4 and severity of asthma:-
There was statistically significant progressive decrease in plasma LxA4 from mild to severe asthma groups.P < 0.001F = 349.018) Relation between LxA4 and severity of asthma:-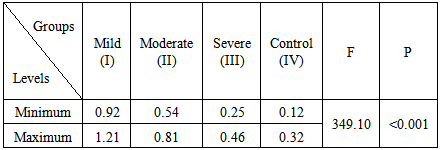 9) T-values of relation between LxA4 levels in studied groups:-
9) T-values of relation between LxA4 levels in studied groups:-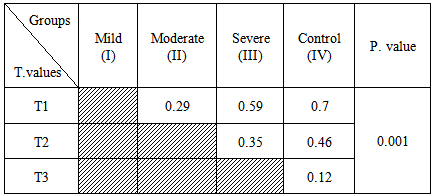 v T1 (relation between group I and other groups)v T2 (relation between group II and groups, (III and IV)v T3 (relation between group III and group IV) Which were significant with P values < 0.00110) Relation between the mean values of LxA4 and control level of patient, groups:-
v T1 (relation between group I and other groups)v T2 (relation between group II and groups, (III and IV)v T3 (relation between group III and group IV) Which were significant with P values < 0.00110) Relation between the mean values of LxA4 and control level of patient, groups:-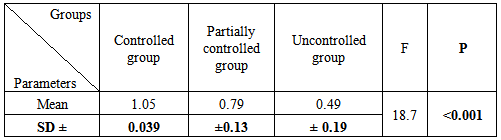 From this table there was statistical significant decline in the mean values of LxA4 from controlled to uncontrolled asthmatic groups, (F= 18.7, P < 0.001)11) T.values of relation between LxA4 levels and level of control in patients groups:-
From this table there was statistical significant decline in the mean values of LxA4 from controlled to uncontrolled asthmatic groups, (F= 18.7, P < 0.001)11) T.values of relation between LxA4 levels and level of control in patients groups:-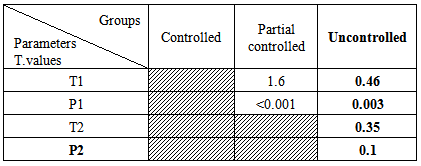 T1 represent the relation between the control group and another two groups, which were 1.6 and 0.46 with P1.values, 0.001 and 0.003 in partially controlled and uncontrolled groups respectively.While T2 represent the relation between partially controlled group and uncontrolled group which was 0.35, with P2.value 0.1 which non significant.12) Lipoxin A4 and its relation to pulmonary function tests:-
T1 represent the relation between the control group and another two groups, which were 1.6 and 0.46 with P1.values, 0.001 and 0.003 in partially controlled and uncontrolled groups respectively.While T2 represent the relation between partially controlled group and uncontrolled group which was 0.35, with P2.value 0.1 which non significant.12) Lipoxin A4 and its relation to pulmonary function tests:-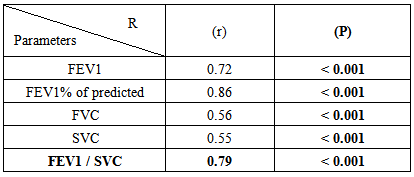 There was a significant positive relation between pulmonary function tests and LxA4 with P.< 0.001.13) Statistical analysis of hsCRP between the studied groups:-
There was a significant positive relation between pulmonary function tests and LxA4 with P.< 0.001.13) Statistical analysis of hsCRP between the studied groups:-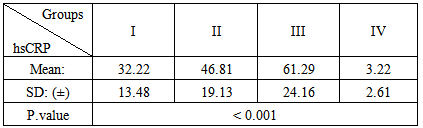 P significantly <0.05hsCRP showed a significant increase in patients groups when compared to control where the mean values were, 32.22 ± 13.48, 46.81 ± 19.13, and 61.29 ± 24.16 in groups I,II,III respectively while in control group was 3.22 ± 2.61 with P.value<0.001.14) Correlation between LxA4 and hsCRP in the patients groups:-
P significantly <0.05hsCRP showed a significant increase in patients groups when compared to control where the mean values were, 32.22 ± 13.48, 46.81 ± 19.13, and 61.29 ± 24.16 in groups I,II,III respectively while in control group was 3.22 ± 2.61 with P.value<0.001.14) Correlation between LxA4 and hsCRP in the patients groups:-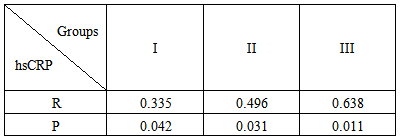 P. significantly < 0.05.There was a negative correlation between LxA4 and hsCRP, where in group I, (r = 0.335, P = 0.042), in group II, (r = 0.496, P = 0.033), and in group III, was (r = 0.638, P = 0.011)15) Distribution of patients groups with asthma in relation to GERD:-
P. significantly < 0.05.There was a negative correlation between LxA4 and hsCRP, where in group I, (r = 0.335, P = 0.042), in group II, (r = 0.496, P = 0.033), and in group III, was (r = 0.638, P = 0.011)15) Distribution of patients groups with asthma in relation to GERD:-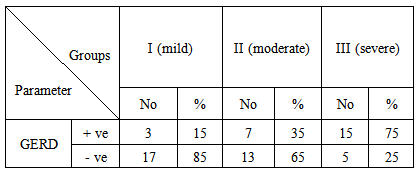 This table showed the percentage of positive cases with GERD in asthmatics as follow, 15% in group I, 35 % in group II, and 75 % in group III.16) The mean values of LxA4 in patient’s groups in relation to GERD:-
This table showed the percentage of positive cases with GERD in asthmatics as follow, 15% in group I, 35 % in group II, and 75 % in group III.16) The mean values of LxA4 in patient’s groups in relation to GERD:-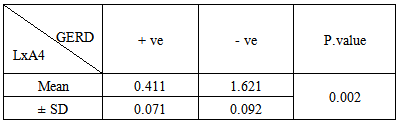 P. significant < 0.05.This table Showed the significant changes in LxA4 between patients as regard to GERD (P=.002) where the mean value of LxA4 was 0.411 ± 0.071 in asthmatic patients with prominent severity of GERD, while the mean value of LxA4 was 1.621±0.092 in asthmatic patients without GERD.
P. significant < 0.05.This table Showed the significant changes in LxA4 between patients as regard to GERD (P=.002) where the mean value of LxA4 was 0.411 ± 0.071 in asthmatic patients with prominent severity of GERD, while the mean value of LxA4 was 1.621±0.092 in asthmatic patients without GERD. 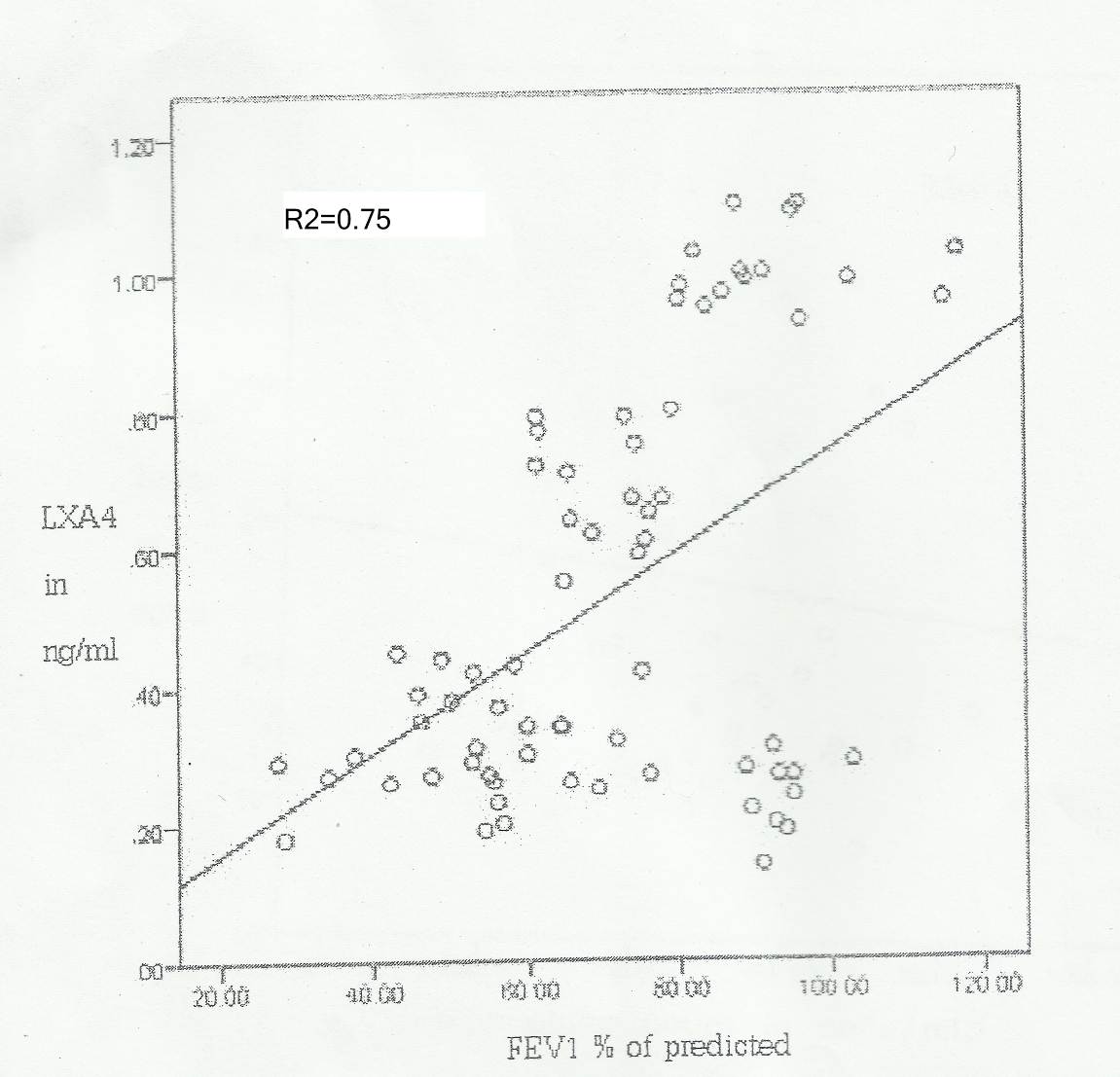 | Figure 8. Scatter plot describing the relation between plasma lipoxin A4 & FEV1% of predicted |
 equation 1t = 11.381 p < 0.001 R2 = 0.7575% of the changes in the plasma level of lipoxin A4 can be predicted by knowing thevalue of FEV1% as R2 = 0.75
equation 1t = 11.381 p < 0.001 R2 = 0.7575% of the changes in the plasma level of lipoxin A4 can be predicted by knowing thevalue of FEV1% as R2 = 0.75 (figure 8)II - Relation of lipoxin A4 with pulmonary function tests:
(figure 8)II - Relation of lipoxin A4 with pulmonary function tests: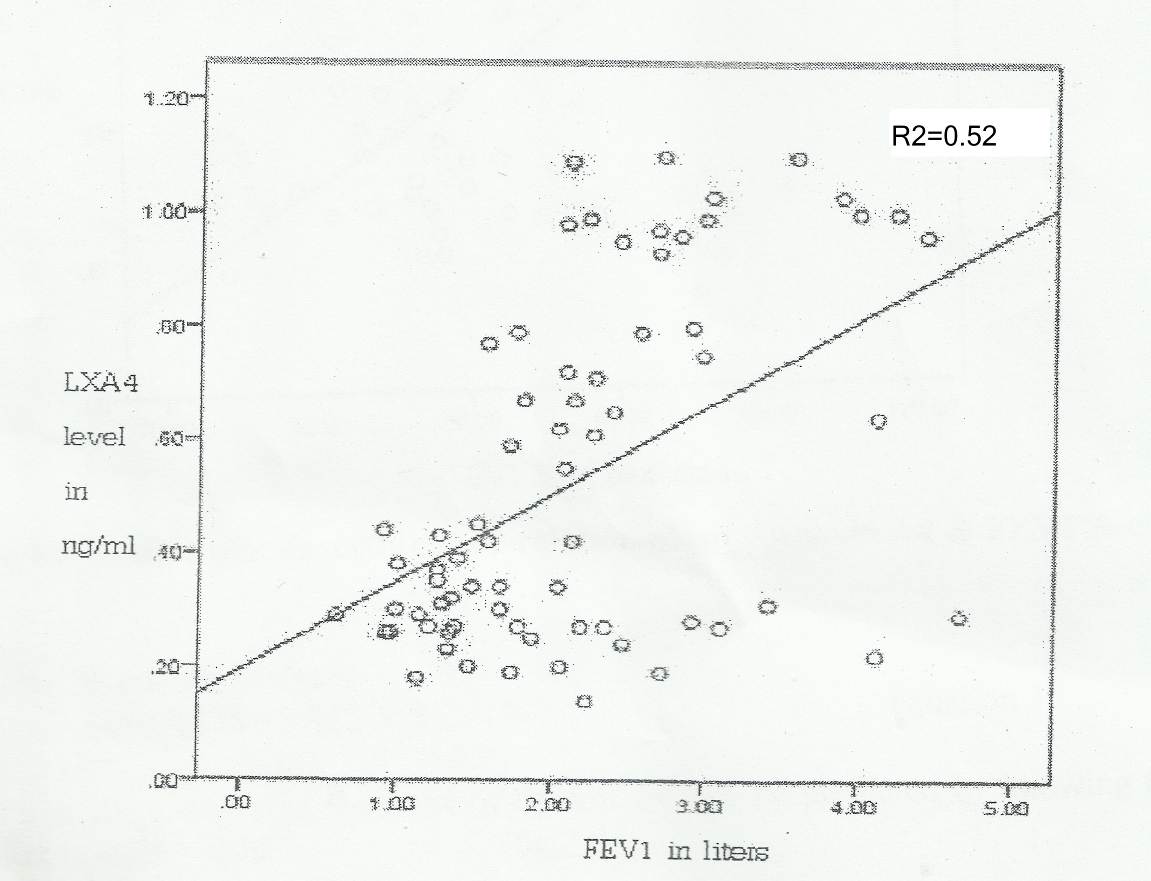 | Figure 9. Scatter plot describing the relation between plasma lipoxin A4 & FEV1 |
 equation 2t = 7.166 p < 0.001 R2 = 0.5252% of the changes in the plasma level of lipoxin A4 can be predicted by knowing thevalue of FEV1 as R2 = 0.52
equation 2t = 7.166 p < 0.001 R2 = 0.5252% of the changes in the plasma level of lipoxin A4 can be predicted by knowing thevalue of FEV1 as R2 = 0.52 (fig 9)
(fig 9)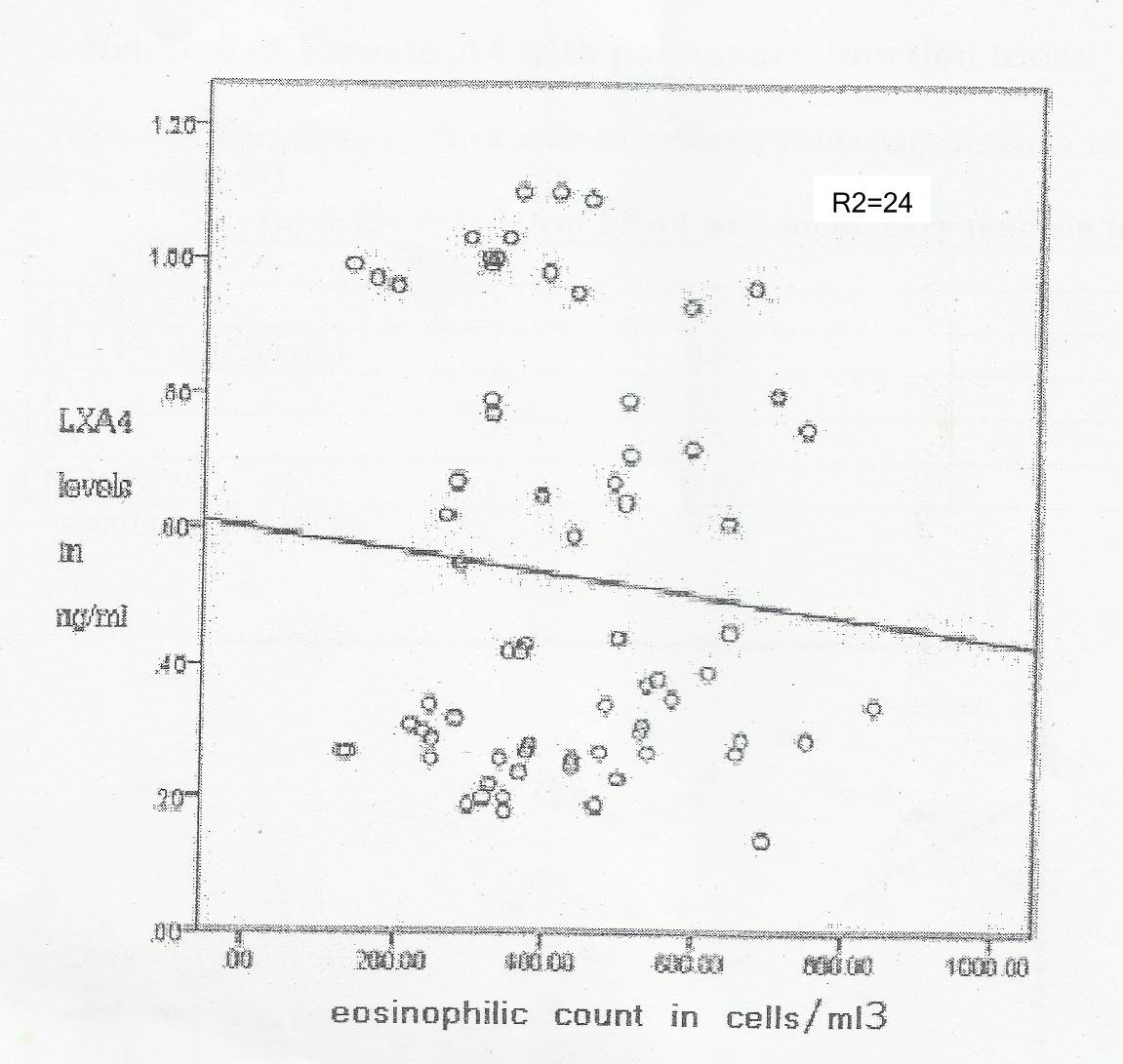 | Figure 10. Scatter plot describing the relation between plasma lipoxin A4 & eosinophilic count in peripheral blood |
 equation 3t = 3.489 p= 0.001 R2=24 24% of the changes in the plasma level of lipoxin A4 can be predicted by knowing thevalue of eosinophilic count as R2 = 24
equation 3t = 3.489 p= 0.001 R2=24 24% of the changes in the plasma level of lipoxin A4 can be predicted by knowing thevalue of eosinophilic count as R2 = 24 (fig 10)
(fig 10)4. Discussion
- Inflammatory diseases of the lung and airways have significant medical and economic burden; bronchial asthma has the highest morbidity among the inflammatory lung diseases (5).The resolution phase of an inflammatory response is an active and orchestrated process, similar in complexity to the onset and maintenance of inflammation (6).Lipoxin A4 (LxA4) has a potent anti-inflammatory properties with cell type specific actions on leukocytes, endothelia, epithelia and other stromal cells (7).The aim of this work was to clarify and asses the value of LxA4 and hs-CRP in asthmatic patients with and without gastro-esophageal reflux disease (GERD), and its correlation with the grades of severity and control. for this purpose, 60 patients having bronchial asthma of different severity ; classified into three groups ; group 1, (mild form), group 2 (moderate), and group 3, (severe form). 20 patients in each, 10 healthy subjects were served as a control.In our study; there was increased level of LxA4 in asthmatic groups more than the control with P. value< 0.001, more-ever, there was significant progressive decline of LxA4 from mild to sever form of asthma, where the mean values were 1.006± 0.061, 0.677± 0.078, and 0.351± 0.075, in groups 1, 2 and 3 respectively with P<0.001 ; these results come in accordance with (6) where they decided that the patients with mild asthma phenotype are considered fighters, having capability of producing anti-inflammatory mediator LxA4 to counter-balance the pro-inflammatory ones, thus abating the inflammatory process, resulting in a mild form of asthma, while patients with severe asthma are weak fighter seems incapable of achieving enough levels of LxA4 to resolve the inflammation, resulting in a severe asthma phonotype.These finding reinforce the hypothesis of an imbalance regulation between pro-inflammatory and anti-inflammatory components involved in the pathogenesis of bronchial asthma (7). Also the mechanisms underlying pathological airway response in sever asthma phenotype include LxA4 biosynthetic enzymes and receptors. Also, (8) and (9), where they found that samples of activated whole blood and supernatant induced sputum from individuals with severe asthma, generated significantly less LxA4 did samples from subjects with mild or moderate asthma.In the present study, LxA4 showed statistically significant positive relation with pulmonary function tests. specially FEV1 and FEV1 % of predicted, where FEV1 was known to be directly related to the air-way characteristics. By using linear regression analysis, (Figure 1), (equation I) it was demonstrated that 75 % of the changes in the level of LxA4 can be predicted by knowing the value of FEV1% predicted as, R2=0.75, and (Figure 2), (equation II) 52% of the changes in LxA4 level can be predicted by knowing the value of FEV1 as R2=0.52, coinciding with the present study, (8) and (9). found that LxA4 level correlated positively with pulmonary function tests, suggesting a link between biosynthetic capacity of this bioactive lipid mediator and air-flow obstruction, specially in asthma patients, while, (10), who mentioned that the association between LxA4 and pulmonary function tests is significant only with FEV1 and not with other tests.As regard to eosinophilic count in different groups, LxA4 showed a significant inverse relation with eosinophilic count and its percentage, by using linear regression analysis (Figure 3), (equation III) it was demonstrated that 24% of changes in LxA4 can be predicted by knowing the value of eosinophilic count as R2=0.24. This result come in accordance with (7), who found that LxA4 is a natural pro-resolving mediator, significantly increased the natural killer cells-mediated eosinophil apoptosis and decreases air-way inflammation, so there was a negative correlation between eosinophilic count and LxA4 level in peripheral circulation in patients with asthma. In addition, these finding indicate that innate Lymphoid cells (ILCs) including natural killer (NK) cells can participate in regulation of allergic air way responses and ILCs are targets for LxA4 to decrease air-way inflammation and mediate the catabasis of eosinophilic response. In another point, LxA4 levels were insignificantly different between patients with controlled and partially controlled asthma in the same group, while it was significant between controlled and uncontrolled patients in one group in comparison with other groups, this denoting that LxA4 related to grades of severity and not the control of asthma.This findings coincide with (10), where they mentioned that the control classification of asthma is completely different from severity classification, where the severity may change over months or years, where as control can be changed from week to another, so, the change of LxA4 in connected and related to degree of severity and not to the level of control of the same group.As regard to hs-CRP, in this study, there was a negative correlation between LxA4 and hs.CRP levels in patients group; and this finding come in accordance with (11), who found that hs.CRP is an acute phase protein, was increased gradually in asthmatic patients from mild to sever degrees and with deterioration of respiratory functions. These finding explore the relationship between blood eicosanoids (e.g. LxA4) and one of acute phase protein (hsCRP) and its pathogenic role in Bronchial Asthma.In our study, the plasma LxA4 levels were significantly decreased in asthmatic patients with recurrent and manifested GERD symptoms specially in severe asthma phenotypes; this come in accordance with (12), who showed that the administration of LxA4 to rats with gastritis that had been pre-treated with asprin and rofecoxib significantly reduced the severity of gastric mucosal damage, denoting that LxA4 has a protective effect on gastro-esophageal mucosa, and abolishing the GRED symptoms.Also, (13),(14), mentioned that the Bio-synthesis and mobilization of LxA4 decreased from epithelial and stromal cells in patients with severe asthma phenotype associated with GRED, hence the symptoms of reflux become more prominent than the other forms which may be due to the lack of protective mechanism of LxA4 on gastro-esophageal mucosa. Also, (15), mentioned that LxA4 known to resolve the injury by reducing the release of inflammatory cytokines specially interleukin 6 (IL6) and induce the proliferation of basal epithelial cells. in addition, LxA4 prevent acute inflammation by presenting the migration of neutrophils into the damaged area, hence, promotes restoration of damaged layers, and inhance the healing so LxA4 considered a protective agent specially in asthmatic patients with GERD. In conclusion, insufficient generation of LxA4 and defective Lipoxin counter –regulation may be the reason for the asthmatic patients whose illness become more serious; also, there were negative correlations between LxA4 in one side and hs.CRP, easinophilic count and severity of GERD in the other side.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML