-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2014; 4(3): 102-104
doi:10.5923/j.ajmms.20140403.04
Enteropathy-Type T Cell Lymphoma Complicating Undiagnosed Celiac Disease in a Saudi Adult: Case Report
Mohamed-Elbagir K Ahmed1, Khalid Nabrawi2, Abdul Rahman Al Shehri3, Wajih Ahmed Siddiqui4
1Professor, Department of medicine, King Khalid University, P O Box 641, Abha, Kingdom of Saudi Arabia (KSA)
2Consultant gastroenterologist, Aseer central hospital, P O Box 34, Abha, KSA
3Consultant haematologist, Aseer central hospital, P O Box 34, Abha, KSA
4Haematology specialist, Aseer central hospital, P O Box 34, Abha, KSA
Correspondence to: Mohamed-Elbagir K Ahmed, Professor, Department of medicine, King Khalid University, P O Box 641, Abha, Kingdom of Saudi Arabia (KSA).
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Background:Celiac disease (CD) is an autoimmune disorder triggered by dietary gluten in genetically susceptible individuals, and it affects about 1% of the population in Europe and North America. There are scarce data regarding the prevalence of celiac disease in Saudi Arabia, but a recent study has shown a seroprevalence of 1.5% among 204 healthy blood donors.We present an adult Saudi patient who developed lymphoma on top of undiagnosed Coeliac.Pateint Presentation:A 70-y-old man was admitted complaining of a generalized abdominal pain for the past five days prior to admission. He reported having significant weight loss over the past 3 months. Clinical examination revealed a thin man with conjunctival pallor and generalised abdominal tenderness but no abnormal findings in all systems. Investigations including abdominal CT scan, coeliac markers, enteroscopy, and histopathology confirmed the diagnosis of T-cell lymphoma on top of undiagnosed celiac disease.Conclusions: Celiac disease may remain undiagnosed till complications occur. A high index of suspicion should be applied to diagnose this disease knowing that sensitive markers for it are now available.
Keywords: Celiac disease, Lymphoma, Saudi arabia
Cite this paper: Mohamed-Elbagir K Ahmed, Khalid Nabrawi, Abdul Rahman Al Shehri, Wajih Ahmed Siddiqui, Enteropathy-Type T Cell Lymphoma Complicating Undiagnosed Celiac Disease in a Saudi Adult: Case Report, American Journal of Medicine and Medical Sciences, Vol. 4 No. 3, 2014, pp. 102-104. doi: 10.5923/j.ajmms.20140403.04.
1. Introduction
- Celiac disease (CD) is an autoimmune disorder triggered by dietary gluten in genetically susceptible individuals, and it affects about 1% of the population in Europe and North America 1. Its prevalence has been underestimated, but it is now considered one of the most common genetic disorders in the West with a prevalence of 1%-2.67% [1-3]. Until the 1990s, the prevalence of CD in the middle East and North America was considered low. However, with the introduction of sensitive serological markers such as anti-endomysial antibodies (AEA), anti-transglutaminase antibodies, and anti-gliadin antibodies (AGA), CD has been more readily reported from developing countries and its prevalence seems similar to that of Western countries [4-7]However, there are scarce data regarding the prevalence of celiac disease in Saudi Arabia [8], but a recent study has shown a seroprevalence of 1.5% among 204 healthy blood donors [9].In addition, another recent study provides evidence of a high seroprevalence of CD in a group of school-aged children in 3 regions of Saudi Arabia. Although intestinal biopsies were not available, the high specificity of IgA anti-EMA indicated one of the highest celiac disease prevalence rates in the world. [10] The diagnosis of celiac disease requires a small intestinal biopsy with characteristic histological findings, including intraepithelial lymphocytosis, crypt hyperplasia, and villous atrophy [4].
2. Patient Presentation
- A 70-y-old man was admitted complaining of a generalized colicky abdominal pain for the past five days prior to admission. This was associated with constipation and few episodes of greenish vomiting. There was no fever and no respiratory, cardiac, neurologic or urinary symptoms. He reported having recurrent childhood diarrhoea, and recently, a poor appetite and significant weight loss over the past 8 months. His past medical history was significat for intestinal bilharzia 16 years ago for which he received praziquantel few years ago, and also appendicectomy 3 years back. He is neither diabetic nor hypertensive. He does not smoke and never consumed alcohol. His medications included analgesics and multivitamines.Physical examination reveaed a thin man with conjunctival pallor but no jaundice. There was no lymphadenopathy, clubbing, or stigmata of chronic liver disease. Cardiac, respiratory, and central nervous sysytem examinations were unremarkable. The abdomen was mildly distended without organomegaly or ascites. Examination of the lower limbs was unremarkable.
3. Investigations
- Complete blood count showed the following: Hb: 10.2 grams/dl (hypochromic & microcytic), TWBC of 7.6 with 58% lymphocytes, and platelet count of 475,000. The coagulation profile was within normal.Biochemistry tests showed blood urea of 50 mg/dl, serum creatinine of 1.0 mg/dl, Sodium of 133 mmol/dl, and K of 3.8 mmol/dl. The liver function tests were as follows: total bilirubin; 0.8 mmol/dl, serum albumin: 3.2 G, Alanine transferease (ALT): 56 units, Glutamyl transferase: 61 units, Alkaline phosphatase of 552 units and lactate dehydrogenase was 147 units.Chest X-ray and ECG were within normal.CT abdomen ( Fig 1) revealed multiple mesenteric lymph nodes and thickening of the jejunum and ilium and mild splenomegaly. No liver abnormality.
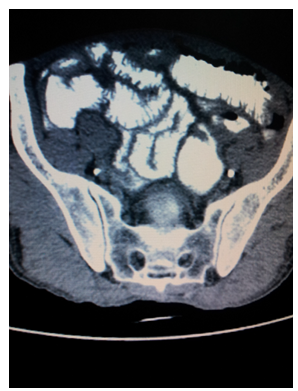 | Figure 1. CT scan showing small bowel thickening and ulceration |
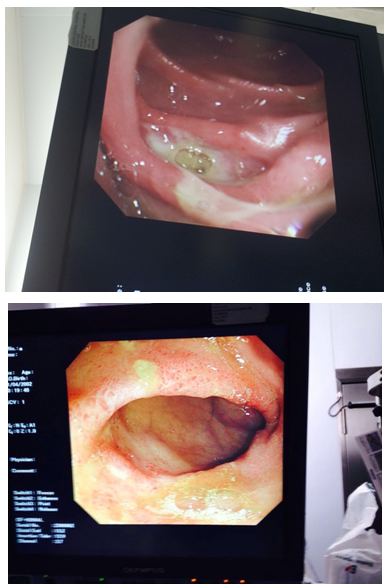 | Figure 2. Endoscopy showing oedema and ulceration of the upper jejunum |
4. Discussion
- To our knowledge, this report is the first of its kind in Saudi Arabia. It shows that the presence of lymphoma in this patient is most likely linked to undiagnosed celiac disease which was overlooked for a long time possibly because of atypical presentation or misdiagnosis. Besides nutritional deficiencies due to malabsorption, serious complications of CD include ulcerative jejunoileitis, osteomalacia, cavitating mesenteric lymph node syndrome (CMLNS) and an increased risk of malignancies, particularly small bowel lymphoma. [11] Several studies in non-Middle East populations have found a positive association between celiac disease and malignant lymphomas [12-14] especially the rare enteropathy-type T-cell lymphoma. However, earlier estimates of risk of non-Hodgkin lymphoma in celiac disease showed wide variations from no increased risk, a 3 to 6 fold risk, a 42-fold increase, or a 69-fold increased risk of death from non-Hodgkin lymphoma [13-18].In neighbouring countries Turkey and Iran, non-Hodgkin lymphomas are the most common CD-associated malignancies [19-20].Our patient was advised to have a gluten free diet and offered chemotherapy for his lymphoma.
5. Conclusions
- CD prevalence is underestimated, with little data available about its malignant complications especially in the Middle East. More efforts should be targeted to diagnose this disease at an early stage in order to prevent serious complications such as enteropathy type T-cell lymphoma, presence of unsuspected nutritional deficiencies, association with low birth weight infants in affected mothers, and other autoimmune diseases.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML