-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2014; 4(1): 14-18
doi:10.5923/j.ajmms.20140401.03
Stroke Etiology Varies with Age in Patients Younger than 50 Years: Assessment of Stroke Etiology and Classifications in Young Saudi Patients
Fawzi Babtain1, 2, Harsha Bhatia2, Ebtesam Al Shehri1, Basma Al Ghamdi1, Eman Al Amer1, Manal Al Jabri1, Mohanned Alhamrani1, Naif Ali1, Adel Alhazzani1, 2, Muthusamy Velmurugan2
1College of Medicine, Department of Intern medicine, King Khalid University, Abha, Saudi Arabia
2Division of Neurology, Aseer Central Hospital, Abha, Saudi Arabia
Correspondence to: Fawzi Babtain, College of Medicine, Department of Intern medicine, King Khalid University, Abha, Saudi Arabia.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
This study was undertaken to determine if stroke classifications and etiologies vary according to age in young Saudi patients with stroke. A retrospective analysis of 80 patients with ischemic stroke younger than 50 years was conducted, and risk factors and stroke classifications using TOAST (Trial of Org 10172 in Acute Stroke Treatment) were identified for all patients, and in those younger and older than 30 years of age. 52.4% of the patients had hypertension, 51 % had carotid stenosis of 50% or more, 40 % had diabetes, 35 % had a documented cardiac disease and 29% had hyperlipidemia. Hypertension, carotid disease and hyperlipidemia were significantly seen in patients older than 30 years (p <0.05). Presence of no identified risk factors was significantly seen in those aged 30 years and younger (p<0.05). Cardiac disease and diabetes were not associated with a particular age group. TOAST classification showed that 50% of the cases had stroke secondary to cardio-embolic and small vessel disease, 24% had cryptogenic stroke, 15% had a large vessel disease, and 11% had stroke of other determined etiologies. Large and small vessel disease were strictly seen in those older than 30 years (p< 0.05), while stroke of other determined etiology and cryptogenic stroke were mostly seen in those aged 30 years and younger (p< 0.05). Cardio-embolic stroke were seen among the entire group with no particular distribution. Therefore, there is an age specific distribution of the risk factors and classifications in young patient with stroke.
Keywords: TOAST classification, Stroke in young, Stroke aetiology
Cite this paper: Fawzi Babtain, Harsha Bhatia, Ebtesam Al Shehri, Basma Al Ghamdi, Eman Al Amer, Manal Al Jabri, Mohanned Alhamrani, Naif Ali, Adel Alhazzani, Muthusamy Velmurugan, Stroke Etiology Varies with Age in Patients Younger than 50 Years: Assessment of Stroke Etiology and Classifications in Young Saudi Patients, American Journal of Medicine and Medical Sciences, Vol. 4 No. 1, 2014, pp. 14-18. doi: 10.5923/j.ajmms.20140401.03.
Article Outline
1. Introduction
- Stroke is the most common neurological disease, and the second most common cause of death. It comes the sixth among the disease burden according to the World Health Organization (WHO).[1] Stroke in young contributes to around 5% of all stroke patients[2] and its incidence increases with age[3] . It is known that stroke etiology and risk factors in this young population are different from those identified in the older population[4], and these risks remain unknown in some of the young patients despite an extensive stroke work up[5]. Yet, the interest in stroke evaluation among the young increases with the availability of advanced diagnostic tools, especially for the uncommon etiologies. Therefore, the present study was carried out to assess stroke classifications and etiologies, evaluate the stroke risk factors in young patients with stroke, and to assess if these risk factors vary among the young patients.
2. Methods
- This is a one-year retrospective analysis of stroke in 80 patients of Saudi nationals aged between 16 and 50 years, who were evaluated at Aseer Central Hospital, Abha, Saudi Arabia from January 2010 to December 2010. The data obtained for this study is a part of the stroke registry available in Aseer Central Hospital for all patients evaluated during the study period; the data included patient’s file numbers, age, sex, diagnosis, and risk factors. The patients were selected from 421 patients registered in our stroke registry during the study period and fulfilled the inclusions criteria which include: a) ischemic stroke confirmed by the clinical history and neurological examination; and b) computerized topography (CT) or magnetic resonance imaging (MRI) of the brain to confirm the presence of ischemic changes. Patients with intracerebral hemorrhage, subarachnoind hemorrhage, subdural or epidural hematoma, cerebral vein thrombosis, and transient ischemic attacks (TIA), and patients with incomplete medical records or clinical data were excluded. All patients had electrocardiogram (ECG), echocardiogram, fasting lipid profile and fasting blood sugar, and blood pressure was monitored on admission and every 8 hours during the hospital stay. The LDL level of more than 100 mg/dL was used to determine hyperlipidemia. Patients with anterior circulation stroke or stroke with undetermined localization had carotid doppler, and suspected case of cardio-embolic stroke underwent a 24 holter monitor. Hypercoagulable work up for arterial thrombosis (including anti-cardiolipin antibodies, lupus anticoagulants) and immunological screening (including antinuclear antibodies, ANA, and anti-double stranded DNA) were performed in suspected cases of hypercoagulable state and vasculitis. Vascular imaging of the intracranial vessels using CT or MR angiography was performed in patients with posterior circulation stroke or suspected vasculitis. Stroke risk factors were determined for all the patients, and a neurologist reviewed the neuroimaging in order to classify the stroke type according to TOAST classifications[6]. Patients up to 50 years of age were included so our results would be comparable with previous studies[7]. Our hospital does not require ethical approval for retrospective studies. TOAST classification was determined for the whole group. To evaluate any age specific distribution of TOAST, the group was subdivided into those older and younger than 30 years of age.
2.1. Statistical Analysis
- Statistical analysis was performed using contingency tables and Fisher exact test or X2 test for categorical variables and Student t test for continuous variables. Significance was set at p < 0.05. Data analysis was performed using IBM SPSS Statistics for Macintosh, Version 20.0.0, Armonk, NY: IBM Corp.
3. Results
- Eighty patients fulfilled the inclusions criteria. There were 52 men (65%), with mean age of 37.4±10.6 years (mean ± SD) (range; 17-50). Hypertension was the most common identified risk factor, being seen in 42 patients (52.5%), and followed by carotid artery stenosis in 41 patients (51%). Diabetes was documented in 32 patients (40%), cardiac disease in 28 patients (35%), hyperlipidemia in 23 patients (29%), and smoking in only 12 patients (15%). Some of the patients had more than one identified risk factor. Other identified risk factors included dissection of an extracranial large artery (3 cases), vasculitis (2 cases), systemic lupus erythematosus (SLE) with antiphospholipid syndrome (2 cases), Neuro-Behcet (1 case), and sickle cell disease with moyamoya syndrome (1 case). Nineteen patients (24%) had no identified risk factors. Among the identified cardiac etiologies leading to stroke in 28 patients, dilated cardiomyopathy was documented in 9 patients (32%), ischemic heart disease in 7 patients (25%), atrial septal aneurysm (ASA) in 4 patients (14 %), valvular heart disease (VHD) in 4 patients (14%), rheumatic heart disease (RHD) in 2 patients (7%) and atrial fibrillation (AF) in 1 patient (4%). None of these risk factors had gender predominance.Anterior circulation was the most involved territory among our young patients with stroke, and was observed in 69 cases (86%), and it involved more than one artery in 15 cases (19%). On the other hand, the posterior circulation stroke was seen in 11 cases (14%). Both arterial distributions were seen more in men (57% and 82% respectively).
3.1. Stroke Classifications and Age
- Stroke was classified according to TOAST classification (Table 1). Small vessel disease and cardio-embolic stroke accounted for half of the stroke etiologies in our young Saudi patients with stroke (25% each). On the other hand, 12 patients (15%) had stroke secondary to a large vessel disease, and 9 patients (11%) had stroke with determined etiology. Only 19 patients (24%) had cryptogenic stroke.
|
3.2. Stroke Risk Factors and Age
- Further analysis of the risk factors according to age was performed. The patients were divided into two groups; 30 years and younger, and 31 to 50 years of age. Figure 2 shows the distribution of the stroke risk factors according to age. Hypertension, carotid artery stenosis and hyperlipidemia were significantly seen more in patients older than 30 years (p <0.05), while other identified risk factors were a significant finding in patients aged 30 years and younger. Similarly, presence of no identified risk factors was significantly observed in patients aged 30 years and younger (p <0.05). Diabetes and cardiac disease were seen among all ages with no particular age distribution.
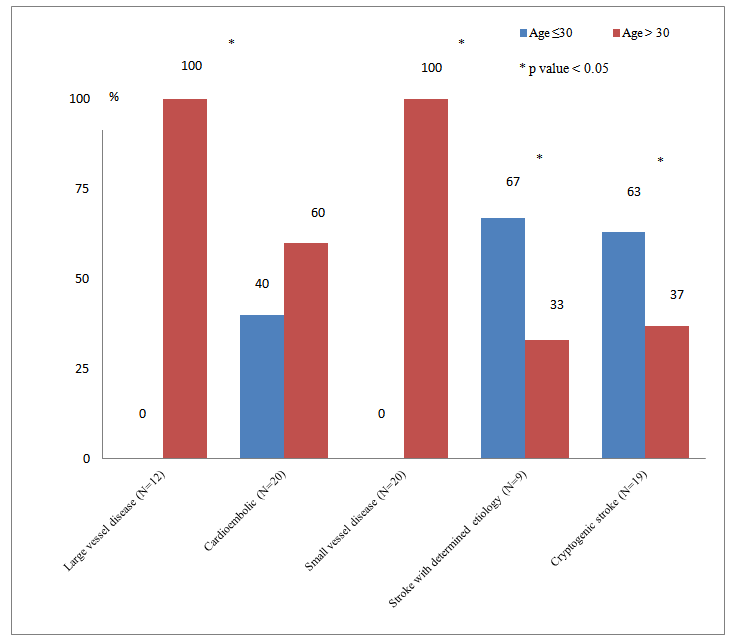 | Figure 1. TOAST stroke classifications according to age |
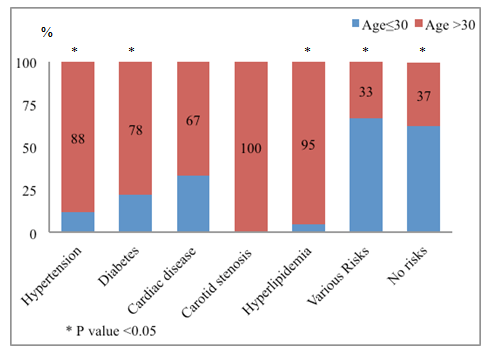 | Figure 2. distribution of risk factors according to age |
4. Discussion
- While a specific definition of “young stroke” is lacking, the vast majority of authors consider “stroke in young” to pertain to individuals under 50 years of age. To our knowledge, the present epidemiological study is the first that has evaluated risk factors for ischemic stroke in young adults in the southern part of Saudi Arabia. Despite the scarce stroke data from this region with the exception of few hospital-based reports, the data revealed a higher incidence of stroke in young than expected; however, the prevalence and distributions of stroke risk factors identified in our population were similar to those reported in the literature.[8,9]Hypertension remains the most frequently identified stroke risk factor in patients with stroke, particularly in the young population. Besides hypertension, other traditional risk factors such as diabetes, cardiac disease, history of smoking, and hyperlipidemia were also identified, and unusual etiologies, namely hypercoagulable state, vasculitis and none atherosclerotic arteriopathies, were determined in some cases lacking the traditional risk factors.[10-13] Risk factors such as hypertension and hyperlipidemia are common in young population with stroke in the developing countries[14,15], and were significantly seen in our patients older than 30 years of age, which lead to a significantly more small and large vessel disease stroke in this age group. These findings could be explained by the fact that the underlying pathogenesis driven by hypertension and hyperlipidemia will require a time to establish a significant atherosclerosis, and subsequently clinical symptoms and signs related to the involved organ.[16] It has been observed that the stroke risk factors in patients older than 40 years are similar to the older populations.[17] None of our patients who were 30 years and younger had a radiological evidence of carotid stenosis. Stroke related to small vessel disease was seen in one fourth of our young population, an incidence comparable to the previously published reports[12,18], yet it was more frequently encountered in the older population. Our findings would also validate the use of TOAST classification in younger population with stroke, which was questioned previously.[12] Despite the high incidence of strokes related to cardio-embolic phenomena, it was not particularly associated with a specific age group, since cardiac disease leading to stroke was seen across all ages in our study. Nine patients (11%) had stroke related to non-atherosclerotic vasculopathies such as arterial dissection, vasculitis or moyamoya disease; this observation is less than the previously reported in the literature.[19] Interestingly, this stroke class was significantly seen in patients younger than 30 years, probably because of more patients older than 30 years would have other common risk factors. This observation would suggest the need for careful assessment of these risks in the young patients with stroke, especially those younger than 30 years. Cryptogenic stroke was identified in 24% of our young patients with stroke, a finding almost similar to the literature.[19,20] The strong association of the above mentioned stroke types to patients younger than 30 years of age signifies the distribution of risk factors according to age, which revealed an age specific distribution of risk factors, and subsequently stroke classes. To our best knowledge, this is the first report on the presence of an age-specific stroke risk factors and classifications within the young population, something may aid to guide in the stroke investigation in this young age. Cardio-embolic stroke is a major stroke risk factor in young patients with stroke[21], and is one of the most identified stroke risks in the present study. This may be related to the higher incidence of hypertension, diabetes, and hyperlipidemia across all the groups, which increased the risk for ischemic heart disease, probably more in those older than 30 years. Yet, dilated cardiomyopathies of variable etiologies were the most identified cardiac disease in our population, which was associated with stroke in up to 15% in children requiring cardiac transplant.[22] On the other hand, ischemic heart disease (IHD) was reported in 1% of hospital stroke in one study[23], yet it appears to be observed in higher rates in our young population, most probably because of higher incidence of risk factors leading to IHD, and subsequently stroke. Finally, atrial fibrillation is an uncommon stroke etiology in the young population[24], a finding well represented in our study despite the presence of hypertension and IHD that are known to increase its risk. Atrial fibrillation is a well-known risk factor for stroke in the older population, and its incidence increases with age. [25,26]Our study has some limitations. Since this is retrospective study, further investigations of patients with cryptogenic stroke were not performed routinely at the time of the study, where checking homocystein level for instance, or the inflammatory markers such as CRP could identify stroke etiology in these young patients when no classic risk factors identified. Determining these factors could identify further treatable cases, and probably improve the outcome in these patients.
5. Conclusions
- Ischemic stroke in our patients younger than 50 years is commonly seen in practice, with higher than expected rates that could be related to sedentary life, as well as the high incidence of hypertension and diabetes known in our population, all of which might reflect the impact of lifestyle and dietary habits. Furthermore, identifying the variable risk factors within the young population, as reported in the present study, would guide clinicians in investigating these patients. Meanwhile, better understanding of stroke classifications and etiology will improve the diagnosis and management of these patients.
ACKNOWLEDGEMENTS
- We would like to thank Prof. Adel Bondok, Professor of Neuroscience for revising the manuscript.
Conflict of Interest and Funding
- Authors received no financial support from any industry to conduct this study, and no conflicts of interest in performing this study that might bias the interpretation of results.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML