-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2013; 3(5): 97-102
doi:10.5923/j.ajmms.20130305.01
The Self-reported Prevalence and Knowledge of Urinary Incontinence and Barriers to Health Care-Seeking in a Community Sample of Canadian Women
D. Wayne Taylor1, Michael Weir2, Jacqueline J. Cahill3, Diaa E. E. Rizk2
1DeGroote School of Business, McMaster University, and The Cameron Institute, Hamilton, L8S 4M4, Canada
2Department of Urology, Peterborough Regional Health Center, Peterborough, K9J 7C6, Ontario
3The Canadian Continence Foundation, Peterborough, K9J 2R8, Ontario
Correspondence to: D. Wayne Taylor, DeGroote School of Business, McMaster University, and The Cameron Institute, Hamilton, L8S 4M4, Canada.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
The study aimed to determine the prevalence and understanding of urinary incontinence (UI) in a community sample of Canadian women and identify barriers to health-care seeking. Women aged 20 or more were selected randomly from the community and interviewed about inappropriate urine loss within the previous 12 months, the meaning and causes of UI, and their demographics. Attitudes towards health care-seeking and average waiting intervals before medical encounter were also studied. With a response rate of 92%, 36.5% women admitted to having UI. Of this number, 76.5% considered themselves “incontinent” because of amount and/or frequency of leakage; only 55.8% sought medical advice, on average, 14 months post onset. Several reasons for not seeking help were identified. Only 46.2% of respondents interpreted “incontinence” as the inability to control urine; 19.4% defined incontinence as involuntary urine leakage. Exactly one-third of respondents did not know the causes of UI; 63.4% thought it was normal in old age, and 12.9% believed UI could not be cured or improved. Only 51.6% considered UI as any amount or frequency of uncontrolled urine loss. The study concluded that UI is prevalent, poorly-understood and under-reported in Canadian women because of inadequate public knowledge with consequent delay in management. This information should assist in formulating a public education strategy for UI and in planning the social and medical care of incontinent women.
Keywords: Knowledge, Prevalence, Urinary Incontinence, Women
Cite this paper: D. Wayne Taylor, Michael Weir, Jacqueline J. Cahill, Diaa E. E. Rizk, The Self-reported Prevalence and Knowledge of Urinary Incontinence and Barriers to Health Care-Seeking in a Community Sample of Canadian Women, American Journal of Medicine and Medical Sciences, Vol. 3 No. 5, 2013, pp. 97-102. doi: 10.5923/j.ajmms.20130305.01.
Article Outline
1. Introduction
- Urinary incontinence (UI) is an embarrassing and debilitating symptom that is becoming a major health concern for women of all ages with significant public health and economic consequences[1-8]. Female UI is more common with vaginal birth, advancing age and co-morbid medical conditions[4, 7, and 9]. Previous studies have commented on the increasing community prevalence of UI in women worldwide and the psychosocial consequences of having this disorder[1-9]. The role of patient advocacy groups in improving health care and services through community knowledge transfer and government lobbying has been recently appreciated[10]. Incontinence advocacy groups like The Canadian Continence Foundation (TCCF) strive to ensure that all urinary incontinent Canadian consumers have access to evidence-based medical therapy of UI, and that their quality of life is given serious consideration by health policy makers, because UI is still a stigmatized and taboo condition amongst Canadian women. As such, UI is often suffered in silence without seeking health care[3, 9, 11, and 12]. Epidemiological studies and qualitative data show that many individuals do not understand the meaning of the word “incontinence” and therefore the condition is often under-reported[4, 6, 13-15]. Previous patient surveys have also consistently indicated that it takes several years before incontinent woman report the symptoms to a health care provider and/or get referred to the appropriate specialist[3-5, 11]. The reasons were: thinking that the condition could not be treated, feeling embarrassed, and thinking that this is a “normal” part of ageing.Family physicians, who are the primary care providers for the majority of incontinent women in Canada, frequently report that they are not adequately trained to treat incontinent patients and therefore are reluctant to discuss or manage the condition during consultation, and in arranging subsequent care including timely specialist referral[16]. As yet, there is a paucity of accurate figures and recent studies pertaining to the perception, knowledge andhealth-care seeking behaviour of the Canadian female population with regard to UI[9, 12]. The “true” prevalence of this condition in the community is not known[9, 12].This community-based, epidemiological study is important for projecting the need for women’s health services as well as therapeutic intervention. With the continuing drive of patient groups, such as TCCF, to encourage access to incontinence treatment and patient education, it is also pertinent that physicians improve their understanding of women’s perceptions of the condition, identify the biomedical knowledge gaps in public information about UI, and recognize the potential barriers to care-seeking in incontinent women. The objectives of the study were to: 1- Determine the self-reported prevalence of UI in a randomly selected community sample of women including when women perceive this as a “problem”, i.e. quantity or frequency of urine loss, and what “qualifies” as significant or bothersome UI necessitating medical help. 2- Identify the meaning of the term “incontinence” in this group and assess their background knowledge about the causes and treatment outcomes for UI.3- Study the patient-specific reasons for delaying or not choosing to seek incontinence care.4- Measure the waiting interval before medical encounter and specialist referral of incontinent women, and evaluate the practice of family physicians regarding clinical triage.
2. Materials and Methods
- A cross-sectional, population-based survey was conducted on a random cohort of Canadian women aged 20 or more years living in the City of Peterborough, Ontario. In 2006 the population of Peterborough was 74,898. In 2008 the average household income for Peterborough was $60,700, over $20,000 below the provincial average for the 82 cities in Ontario, thus designating it as a “low income” municipality.The following women were excluded either because of the higher risk of developing UI or because UI is not related to obstetric or gynaecologic causes:a) Pregnant women or those who delivered less than 3 months previously.b) Women with neurological diseases known to cause UI such as previous spinal cord injuries, stroke, dementia, disseminated sclerosis and Parkinson’s disease.c) Women with previous major operations or malignant diseases of the urinary tract.d) Women who have permanent urinary stoma. In addition, women who could not communicate in English were also excluded. The study protocol was approved by the Research Ethics Board of the Peterborough Regional Health Centre. Sample size calculation indicated that a study of 101 subjects was adequate to achieve a high degree of precision (± 4%; 95% confidence) in estimating the true prevalence of UI in the general female population of Peterborough[17]. A priori assumption was that the expected prevalence in this group is 4%, similar to that reported in women from Ontario in the largest Canadian study about UI “The Canadian Community Health Survey and Data about UI”, with an anticipated 80% patient response rate[18]. The study population was identified through the telephone listings of Peterborough residents. Subjects were selected, using a simple random sampling technique, utilizing a random number generator, from households who had an eligible woman resident, and were contacted by telephone at home. Telephone interviews were conducted after 17.00h in order to increase participation. In some cases, an initial phone call was made and a further telephone appointment was set up at a mutually agreeable time in order to conduct the survey. Women who were not available were contacted a further two times and if still not available, were excluded and replaced by the subsequent woman in the list. Between March and June, 2011, 101 eligible women were recruited. After receiving information about the study, participation was voluntary and anonymous. The participant’s consent was implied if she agreed to be interviewed and 93 women (92%) agreed to participate in the study.Data were collected by one investigator[DEER] using a structured questionnaire. This consisted of 42 items that included a number of demographic, reproductive, medical and lifestyle variables (Table 1) with closed and open responses. Parity was the number of previous pregnancies > 28 weeks. Chronic constipation was considered as fewer than 3 bowel movements per week for at least 3 months. The survey definition of UI was any self-reported episode of involuntary urine loss within the previous 12 months; the screening inquiry included the concept of “current UI”, UI in the previous 12 months only[2, 3, 7, 11], followed by a series of more specific questions. The questionnaire included items from the psychometrically validated PELVIC FLOOR BOTHER (PFB) questionnaire[19] combined with items based on the responses to the voluntary on-line pilot study of TCCF about UI[20].The urinary component items of the PFB questionnaire are a survey instrument to detect the presence and type of symptom of UI and the degree of bother from UI. The patient-specific questions were generated from responses to the pilot study of TCCF, modified accordingly and categorized into 2 main themes to assess the women’s knowledge about UI and their attitude to care-seeking. All the questionnaire answers were kept anonymous and confidential. A copy of the questionnaire is available from the authors on request.Data was analyzed using Stata 11.06 and Microsoft Office Excel 2007. Differences between proportions were examined by Fisher’s exact test size. Measure of association between variables was assessed by correlation coefficient.Open-ended responses and qualitative data were analyzed using a content analysis approach whereby individual responses were analyzed and categorized into themes. For all analyses, a p value of < 0.05 was considered significant.
3. Results
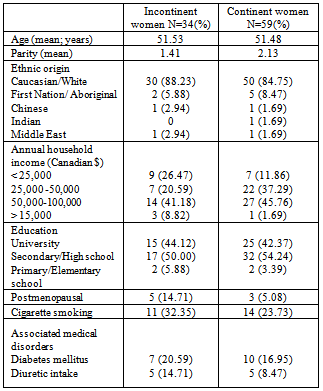
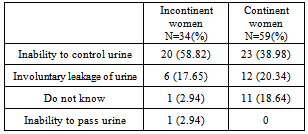
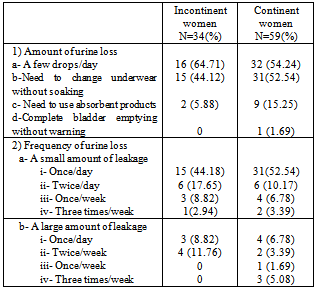
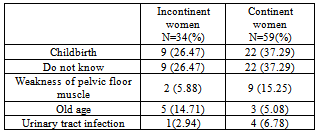
- A total of 93 women out of 101 enrolled subjects participated in the study giving a non-respondent rate of 8%. No further data were available on the 8 women who declined to be interviewed. Thirty four women (36.5%) were incontinent according to the survey definition of UI; 20 (58.8%) complained of stress UI and 14 (41.2%) of urge UI with 16 women (47%) having mixed symptoms (both stress and urge UI). Of the incontinent population, 23 (67.6 %) had mild UI and 11 (32.4 %) had severe UI. Only 19 (55.8%) of the 34 incontinent women had sought medical advice, the 11 women with severe UI and 8 women with mild UI. Table (1) gives the socio-demographic, reproductive and medical characteristics of study subjects. The study sample was representative of the general female population in Peterborough. The mean age of participants was 51.50 years and parity was 1.87. The majority of subjects were Caucasians, married, educated to the secondary school level with a medium annual household income, and non-smokers. Both incontinent and continent women were comparable in the various parameters measured.
|
|
|
|
4. Discussion
- This survey has produced information from a Canadian female community population perspective which can be added to the world literature on the epidemiology of UI. Results showed that almost one third of Canadian women of all ages suffer from UI similar to previous studies[9, 12, and 18]. This finding clearly explains the considerable cost to the health care system incurred by UI, estimated to be CND6 billion per annum in 2009[21]. The symptom of UI remains under-reported mainly because of the lack of women understanding or appreciating the morbidity of the condition with subsequent delay in seeking care from their primary care provider and/or further specialist advice. Comparison of results from various studies estimating the prevalence of female UI is limited by differences in the definition of UI, particularly its onset, severity, frequency and whether or not it poses a social or hygienic problem. Other factors are the ethnic group examined, the type of patient population whether community- or hospital-based, and the standards and methods of data collection[22]. Therefore, available results vary widely but comparable studies of Western women in the community belonging to a similar age spectrum have described prevalence rates between 4 and 60%[1-8, 23]. This study’s result was within this range, and the self-perceived incontinence rate was interestingly similar to the overall incontinence rate of 28.8% found in a recent multi-provincial community study of 518 Canadian women[12].A previous, family practice, clinic-based, Canadian study, however, reported a higher prevalence of UI in women (51%) in another town in Ontario[9]. The difference could be explained by the shorter time frame of one month over which UI was measured in this study with a likely higher recall of symptoms. Our prevalence rate is significantly higher than the 4% rate previously cited in the national Canadian Community Health Survey (CCHS) possibly because of the different manner of enquiring about UI[18]. Unlike the CCHS study, inquiry about UI in our study was based on the assumption that it would detect incontinence of any severity or frequency to be an important problem to the woman concerned to report, whether or not diagnosed by a health professional[3, 11,19, 22]. This definition of UI is similar to the most recent standardized terminology used for UI by the International Continence Society[24] and wascomprehensible to the target Canadian population in the previous TCCF survey[20]. Although pregnancy and vaginal birth is considered the major cause for having female UI, this factor does not totally explain the origin and progression of UI in all women[8]. UI has been observed in nulliparous women and the absence of the condition has been confirmed in many multiparous women, as seen here[9]. Besides obstetric causes, other important risk factors such as age, medical disorders like diabetes mellitus and chronic respiratory diseases, chronic constipation, and diuretic intake are known to be associated with the development of UI[2-4, 9, 12, and 25]. There was no significant association, however, with UI in the present study. A possible explanation could be the under-representation of women with other associated medical disorders in our sample.As observed in this study, perception of UI as a problem for which to seek care is directly related to having severe UI, urge UI and associated sexual dysfunction that grossly under-estimates the “true” community prevalence of female UI[12, 23]. Moreover, even the presence of severe symptoms is probably under-reported because most women are embarrassed to talk about UI and prefer to suffer in silence[6, 13-15, 21]. It is also possible that specific inquiry about the symptom of UI may yield a relatively lower rate of positive answers because of lack of understanding and/or difficulty with interpretation on the subjects’ part of this widely accepted question on interviewing[11,18]. In this study, therefore, a specific question was added about the meaning of the word “incontinence”. Only 76.5% of women understood the proper meaning of the term UI, even if they were incontinent, similar to other studies[6, 14]. Many respondents were also unsure about the definition, causes or treatment outcome of UI and yet aware of the adverse effects. This finding underscores the importance of promotion of public awareness about UI[5].Knowledge translation campaigns and community education programs about UI in Canada should thus focus on explaining the word “incontinence” clearly to women and on discussing the available treatment options for UI and their expected effectiveness. Women should also be informed about the risk factors for having UI and that any involuntary loss of urine irrespective of amount or frequency is abnormal. Raising awareness and channelling information about UI to the general public has a positive impact on care seeking and access to incontinence services[6, 13, and 14]. Canada’s general comparative affluence, well-developed women’s health care delivery infrastructure, near-universal coverage, and public-funding of physician and hospital services tend to balance the traditional barriers to UI care-seeking in women[15]. This explains the low number of incontinent women who did not seek care because of difficulty in accessing health services.A disappointing finding, however, was that some women in the study still believed that UI may either regress spontaneously or is normal at old age, and had low expectations about the results of treatment. The knowledge barrier to seeking help for UI emphasizes the responsibility of health care providers as key informants to correct women’s misconceptions about UI being normal or untreatable[6, 13,14,26]. The majority of the incontinent women sought help from a family physician but after a long interval of over a year, similar to previous Canadian studies [12]. Education and training of family physicians in the management of UI, and raising public awareness of other sources of medical help for UI are, therefore, recommended to improve timely patient access to appropriate incontinence care[5, 27]. Dedicated continence promotion clinics in a community care setting staffed by specialist continence providers may be an alternative means of achieving this objective, particularly if effort is made to make the clinic as user-friendly as possible to the clientele. Surveys are subject to sampling, detection and response biases. The inclusion of only English-speaking women in the study inevitably induced a selection bias against non-English speaking women in Canada. Results cannot be generalized to the entire female population of Canada since this is a city-based survey. The results of this survey, however, can be used as a pilot basis for a further nationwide study of English- as well as French-speaking and other minority language Canadian women. Our data collection technique of telephone interviews contained less detection bias of the community prevalence of UI than surveys based onface-to-face interviews, or self-completed mailed questionnaires, because a larger population of women could be sampled by this relatively inexpensive method, and because most incontinent women can report the symptom freely over the phone through indirect personal contact with an investigator. The anonymity allowed by private telephone participation further optimized freedom of choice and liberty in responses to questions particularly those involving sensitive or personal health topics such as bladder control or sexual activity. This interviewing technique also reduced response bias as a result of direct verbal communication and interaction with participants that provides more accurate information because subjects’ questions can be clarified immediately prior to answering[2,3,11,12]. Response bias was further minimized in our cohort because the interviewer approached women as an independent researcher and not as a service provider when respondents may be reluctant to criticize health care professionals. However, there was no further information to assess the characteristics ofnon-respondents. This could bias the results because motivated participants may differ from non-respondents. The questionnaire included a fixed-choice option about the ethnic origin of participants in an attempt to investigate the recognized role of ethnicity on women’s understanding and attitudes to UI[2, 3]. The small size of the ethnic subgroups precluded further statistical analysis in our study. Another limitation was that our survey did not include detailed qualitative analysis of responses. A further qualitative study may seek suggestions from interviewees about how best to manage UI, for example, what diagnostic and treatment strategies would they be prepared to accept in order to provide more patient-centred information about management of UI.If and when funding is secured for further research in this important area of women’s health, a larger and more nationally representative and stratified sample will be surveyed.
5. Conclusions
- In conclusion, our results support the findings of previous national studies that UI is a prevalent condition in Canadian women. The novel data provided by our study on the Canadian female consumer’s views regarding UI is expected to increase awareness and develop the knowledge base of different stakeholders involved in incontinence service provision in Canada. This should assist in formulating the public education strategy for UI and in planning the social and medical care of incontinent women. Society should be aware that UI is a disorder that needs medical attention. Women must be encouraged to report their problem and seek medical advice and treatment.
ACKNOWLEDGEMENTS
- The study was funded by a 2010 grant from the Astellas US Foundation to The Canadian Continence Foundation.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML