-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2013; 3(4): 91-95
doi:10.5923/j.ajmms.20130304.06
Effect of Feeding Type on Efficacy of Phototherapy in Neonatal Non-Haemolytic Hyperbilirubinaemia
Basil M. Hanoudi C. A. B. P
Department of Pediatrics, College of Medicine, University of Al-Mustansiriyah, Baghdad, Child Central Teaching Hospital, Baghdad, Iraq
Correspondence to: Basil M. Hanoudi C. A. B. P, Department of Pediatrics, College of Medicine, University of Al-Mustansiriyah, Baghdad, Child Central Teaching Hospital, Baghdad, Iraq.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Jaundice is observed during the 1st week of life in approximately (60%) of term infants and (80%) of preterm infants. Breast-fed neonates frequently develop severe jaundice which starts early and is frequently of long duration.A cross section study included 113 newbornsrequiring phototherapy for jaundice of consecutive admissions. Newborns requiring phototherapy for jaundice were admitted to the neonatal intensive care unit of Child΄sCentral Teaching Hospital/Baghdad, between 1st of November 2007 and 1st of July 2008. Newborns were divided into three groups according to type of feeding at the time of admission.Group one newborns were 42 breast-fed, group two newborn were 34 formulas fed andgroup three newborns were 37 mixed-fed. Weight lossat the start of phototherapy was significantly greater in groupone as compared with group two (P<0.001) and group three (P=0.004).Results revealed that the duration of exposure to phototherapy was not significantlydifferent in the three groups (P=0.06). The 24 hours rate of decrease in the bilirubin concentration in group three was significantly better than thatof group one (P=0.008) and group two (P=0.015). The overall rate ofdecrease in the bilirubin concentration during the durationof exposure to phototherapy in group one was significantly lessthan that of group two (P=0.006) and group three (P<0.005). The addition offormula-feedings for totally breast-fed infants, withoutsuspension of breast-feeding would be useful in enhance the efficacy ofphototherapy and reduce the exposure time.
Keywords: Phototherapy, Hyperbilirubinaemia, Breast Feeding
Cite this paper: Basil M. Hanoudi C. A. B. P, Effect of Feeding Type on Efficacy of Phototherapy in Neonatal Non-Haemolytic Hyperbilirubinaemia, American Journal of Medicine and Medical Sciences, Vol. 3 No. 4, 2013, pp. 91-95. doi: 10.5923/j.ajmms.20130304.06.
Article Outline
1. Introduction
- Jaundice is observed during the 1st week of life in approximately (60%) of term infants and (80%) of preterm infants[1].Neonatal hyperbilirubinemia is common and in most cases is a benign problem[2]. Increased enterohepatic bilirubin circulation occurs in infants who are exclusively breastfed and not feeding well, and who have low levels of intestinal bacteria preventing conversion of bilirubin into a non-reabsorbable form[3,4]. Untreated severe unconjugated hyperbilirubinemia is potentially neurotoxic at certain concentrations andconditions[5]. The study was conducted to evaluate the efficacy of phototherapyinnon-haemolytic hyperbilirubinemia ofbreast-fed infants, formula-fedinfants and infants receiving formula and breast-milk.
2. Materials and Method
2.1. Patients
- A cross sectional retrospective study of healthy full term newborns admitted to the neonatal intensive care unit of Child΄s Central Teaching Hospital / Baghdad, between 1st of November 2007 and 1st of July 2008. It included 140 full term newborns requiring phototherapy for jaundice of consecutive admissions were initially enrolled in the study.Criteria ofinclusion; absence of blood groupincompatibility (Rh or ABO), negative direct Coombs’ test, hematocrit (>45%), normal reticulocyte count and normal glucose – 6 - phosphate dehydrogenase activity.Newborns with blood group incompatibility, direct hyperbilirubinemia, excessive bruising orcephalohaematoma, infection or any type of congenital malformations were excluded from the study. The study group was divided into three groups according to type of feeding at the time of admission.Group one newborns were breast-fed, group two newborn were formula fed andgroup three newborns were mixed-fed (received additional bottle feeding of approximately 75ml /kg /day).Each type of feeding was started at birth and continued throughout the study period and was mothers in preference. The group one infants were initially fed frequently (15-60 minutes intervals); the frequency, however, varied with the enthusiasmof mothers averaged about 3 hours, aswas the case for group two and group three infants. The phototherapy was continuous except during feeding, providing nursing care and bathing.Phototherapy wasinitiated when the total serum bilirubin concentration was >12 mg/dl, (205.2 µmol/l) in the first 48 hours of life or >15 mg/dl, (256.5 µmol/l) on subsequent days. Capillary blood was sampled at the start of exposure and at12 hours intervals.Phototherapy was conventional type used, terminated when bilirubin level<10mg/dl (171.0 µmol/l) on two consecutive determinationsasdiurnal variation of bilirubin concentrations considered-and the duration of phototherapy was recorded.The post-phototherapy bilirubin concentration was monitored 12 hourly; the minimum period was 24 hours. If the rebound bilirubinconcentration exceeded thepre-phototherapy concentration, phototherapywas started again according to the same guidelines. The hematocrit values were determined at the start of phototherapy and 24 hours after cessation of exposure to phototherapy. The infantswere weighed at the start and end of phototherapy. Relationships between variables were assessed using Pearson’s correlation coefficient. Values are expressed as mean ± SD. P values (<0.05) were considered to indicate statistical significance. Informed consent from family was obtained.
3. Results
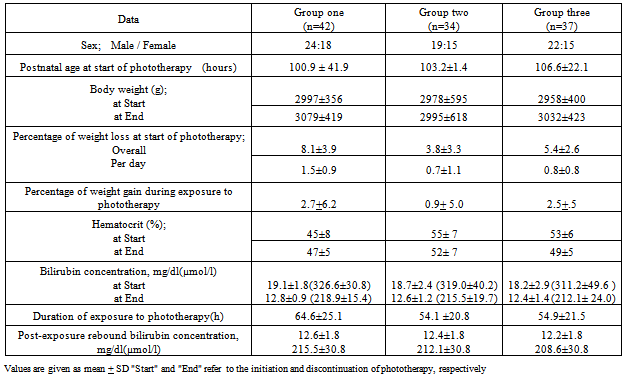
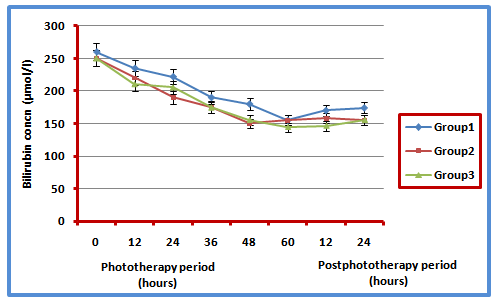
- The study included 140 full term newborns requiring phototherapy for non-haemolytic jaundice of consecutive admissions. The study group included 113 newborns enrolled in the study fulfilling the criteria. The male: female ratio of study group was 65:48. Group one, two and three newborns were 42 breast-fed, 34 formulas fed and37 mixed-fed respectively.The postnatal age at the start of exposure to phototherapy was comparable and not significant among the three groups (P=0.30), as seen in table 1.The body weight at start of phototherapy was not differ significantly in the three groups (p=0.10).Weight loss at the start of phototherapy was significantly greater in group one as compared with group two (P0.001) and group three (P=0.004).The weight loss was significantly different among the three groups, overall loss (P=0.02); loss/day (P=0.01); the loss was more in group one than in group two and three.Results revealed that the lowest weight gain was in group two, however, the differences were not significant between the three groups (P=0.10). Table 1 shows that the hematocrit values at the end of exposure were not differ significantly for all groups (P>0.05).The duration of exposure to phototherapy was not significantly different in the three groups (P=0.06); however, the duration of exposure of group one infants was 10 hours more than the other two groups (Figure1). The duration of exposure to phototherapy was significantly different in the groups one and three (P<0.001).The concentrationsof post-exposure rebound bilirubin were as follows: group one (12.6±1.8mg/dl); group two (12.4± 1.8mg/dl) and group three (12.2±1.8mg/dl). The differences in all groups were not significant during the first 24 hours (P>0.184) (figure 1).
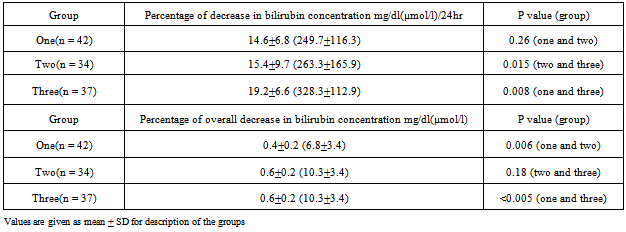
|
|
- Thedifference in rate of decrease of bilirubinconcentration in 24 hours of group oneand two was not significant (P=0.26), while rate of decrease in the bilirubin concentration in group three was insignificantly different and better than group two (P=0.015) and group one (P=0.008) (table 2).The overall rate of decrease in the bilirubin concentration during exposure to phototherapy in group one was significantly lowerthan that of group two (P=0.006) and group three (P<0.005) whereasthe overall rates of decreasein the bilirubin concentration were not significantly different between groups two and three (P=0.18) Table 2and figure 1.The duration of jaundice in group one was much more prolonged, in some casesextending beyond 1 month of age and no additional phototherapy forreboundhyperbilirubinemia was required. The jaundice in group two and group three infantsfaded much more rapidly than group one. It was no longer apparent 7-10 days after completion of exposure to phototherapy.
4. Discussion
- There are several ways in which breast-feeding could contribute to marked neonatal hyperbilirubinemia. The breast-feeding was highly related to the development of exaggerated jaundice. The most common occurrence of jaundice requiring phototherapy was in breast-feeding infants in whom no cause for the jaundice could be determined. Our study findings were most compatible with a theory of relative caloric deprivation as an explanation of the increased incidence of hyperbilirubinemia found in breast - fed newborns, Maisels[12]. Other likely contributing factors and facts were lower fluid intake, greater weight loss and increased enterohepatic circulation of bilirubin [4,6,7].In our study, results showed that the postnatal age at the start of exposure was not significantly different among the three groups (P=0.30). However, phototherapy remained highly effective in controlling the hyperbilirubinemia, but with significantly lower efficacy for group one as compared with the other two groups. These results are consistent with those reported by Tan (8) and Gulcanet al.[9].Weight loss at the start of phototherapy was significantly higherin group one as compared with group two (P<0.001) and group three (P=0.004). Breast-fed newborns lost more weight, and presumably received fewer fluid and calories in the first few days of life than formula-fed newborns. The weight loss was significantly different among the three groups, overall loss (P=0.02); loss/day (P=0.01) It has been found found that the weight loss was not significantly different among the three groups (P=1.0)Tan.[10,11]There is an inverse relationship between oral caloric intake and serum bilirubin concentration, particularly in newborns who weight <2000gr.[6,7,12]. The higher weight loss in group one newborns and slower response of hyperbilrubinemia to phototherapy can be explained by the reduced intake of calories and reduced passing motion that lead to increase in the enterohepatic circulation.A phototherapy study conducted by the National Institute of Child Health and Human Development revealed that newborns who were receiving <90 Cal/kg/day had significantly higher peak bilirubin concentrations than those fed >90 Cal/kg/day and showed that phototherapy was much less effective when caloric and fluid intakes were low[9,10].In our study; the duration of exposure to phototherapy was not significantly different in the three groups(P=0.06);however, the duration of exposure of group one infants was 10 hours more than that of theother two groups (figure 1). Tan (8) and Lazar et al.(13) found that breast-fed full term healthy newborns with non-hemolytic hyperbilirubinemia showed slower response to phototherapy and required a longer duration of treatment than newborns fed a mixed formula and breast-milk. Tan (8)found theduration of exposure to phototherapy was as follows: group one (38.6+12.61 hours) andgroup three (26.8+9.4 hours). The duration of exposure to phototherapy was significantly different in the two groups (P<0.001).The 24 hours rate of decrease in the bilirubin concentration in group three was significantly better than that of group one (P=0.008) and group two (P=0.015); the difference in rates of decrease for groups one and two was non-significant (P=0.26), also observed by Lazar et al. and John[13,14]. The overall rate of decrease in the bilirubin concentration during the duration of exposure to phototherapy in group one was significantly lower than that of group two (P=0.006) and group three (P<0.005); the rates for groups two and three were similar (P=0.18). Gartner and Gulcanet al. found that the overall rate of decrease in the bilirubin concentration during the duration of exposure to phototherapy in group one was significantly lower than that of group three (P=0.01)[4, 9]The post-exposure rebound bilirubin concentrations was comparable in all groups during the first 24 hours (P>0.184) with no significant difference. It was advised that newborns need not be detained in hospital to measure rebound bilirubin levels after phototherapy is completed and that significant rebound after discontinuation of phototherapy is rare Lazar et al and Yet mam et al[13,15].A study by Newman J and Newman TB have recommended that phototherapy may be discontinued in healthy, full term newborns once total serum bilirubin falls <14 - 15 mg/dl (239.4-256.5 µmol/1)[19,20].The overall rate of decrease in the bilirubin concentration during the duration of exposure to phototherapy in group one was significantly lower than that of group two (P=0.006) and group three (P<0.005); the rates for groups two and three were similar (P=0.18).Also overall rate of decrease in the bilirubin concentration during the duration of exposure to phototherapy were similar to findings noted by Tan, Gulcanet al, Brown et al and Tan.[8,9,17,18].Tan[8] found that the overall rate of decrease in the bilirubin concentration during the duration of exposure to phototherapy in group one was significantly lower than that of group three(P=0.01), but these patients would show significantly slower response to this treatment than group three newborns. This is similar to study of by Newman J and Newman TB[19,20]
5. Conclusions
- 1. Phototherapy was highly effective in reducing the bilirubin concentration in neonatal non–haemolytic hyperbilirubinemia.2. The response to phototherapy of breast-feeding infants was significantly slower than that of formula-feeding and mixed-feeding infants; this response was still of adequate efficacy.3. The addition of formula-feeding for breast-feeding infants without suspension of breast-feeding could be useful to enhance the efficacy of phototherapy and reduce the exposure time.
6. Recommendations
- 1. Breast-milk is strongly recommended as the preferred feeding patternin newborns with rare exceptions[21,22].2. Phototherapy is highly effective in reducing the bilirubin concentration in neonatal non-haemolytic hyperbilirubinemia.3. In Breast-feeding infants with severe jaundice that requires phototherapy, the addition of formula-feeding might enhance the response to phototherapy[23,24]. 4. In breast-feeding newborns with significant jaundice and especially with large weight losses; should alert the health care provider to increase the frequency of breast -feeding as the infant might not be breastfeeding well[25,26].
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML