-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2013; 3(2): 22-26
doi:10.5923/j.ajmms.20130302.02
Safety and Efficacy of Azithromycin in Uncomplicated Typhoid Fever in North Indian Population
Manish Chandey1, Rahul Mannan2, Gurinder Mohan1, Tejinder Singh Bhasin2
1Department of Medicine, SGRDIMSR, Amritsar-143001, India
2Department of Pathology, SGRDIMSR, Amritsar-143001, India
Correspondence to: Manish Chandey, Department of Medicine, SGRDIMSR, Amritsar-143001, India.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Enteric fever is a major public health problem in third world countries including India. In past, many antibiotics have been used in typhoid fever. For the last few years, multidrug resistant strains of salmonella typhi are being reported from all parts of the world including Indian subcontinent. The present study , carried out in the north India, was designed to evaluate the clinical efficacy and safety of azithromycin in uncomplicated typhoid fever cases. 100 adult proven cases of typhoid fever aged between 18 and 65 years, who did not took any antibiotic, were included in the study. All patients were given oral azithromycin 1 gm on day 1 followed by 500mg daily from day 2 to 7. Azithromycin therapy was well tolerated in most of the patients. Cure rate of 98% with mean fever clearance time of 3.66+/-0.91 days was achieved in our study .Side effects were not serious enough to withhold the treatment.Thus it is concluded that azithromycin is an effective and safe oral agent for treatment for typhoid fever.
Keywords: Typhoid, Azithromycin, India
Cite this paper: Manish Chandey, Rahul Mannan, Gurinder Mohan, Tejinder Singh Bhasin, Safety and Efficacy of Azithromycin in Uncomplicated Typhoid Fever in North Indian Population, American Journal of Medicine and Medical Sciences, Vol. 3 No. 2, 2013, pp. 22-26. doi: 10.5923/j.ajmms.20130302.02.
Article Outline
1. Introduction
- Typhoid fever (also known as enteric fever) is an acute systemic disease resulting from infection by a specific organism, Salmonella typhi. It is a major endemic public health problem in India due to suboptimal sanitary and hygiene practice. Its incidence in India has been reported to be as high as 7.6 per 1000 per year with an estimated 6-8 million cases occurring per year. Case fatality rate due to typhoid has varied between 1.1 and 2.5% in the last few years[1]. Intestinal haemorrhage and bowel perforation, two most feared complications were common causes of death in 12 to 32 percent of cases. The frequency of complications of typhoid fever has been reduced to 2% or less since the advent of effective chemotherapy[2].Antimicrobial therapy remains the cornerstone for treatment of typhoid fever. Various antibiotics including chloramphenicol, cotrimoxazole, amoxicillin and flouroquinolones have been used in typhoid fever with variable success rate. In India, fluoroquinolones are one of the most common oral agent used for typhoid fever but quinolones resistant strains of salmonella typhi are being reported[3,4]. Moreover, quinolones are contraindicated in pregnant and lactating women as well as in paediatric age group. Also, they are to be used with caution in combination with NSAIDs in patients with history of seizure disorder. There are also reports from the Indian subcontinent of isolates that are fully resistant to fluoroquinolones and the extended spectrum cephalosporins[5]. In recent years various studies have tried in different parts of the world to elaborate the role of azithromycin as an alternate oral agent in typhoid fever[6,7]. Crum NF also advocated Azithromycin as alternatives to fluoroquinolones in multidrug resistant enteric fever[8]. However there was lack of substantial data in Indian population especially in north indiaThe present study, carried out in the northern part of the country, was designed to evaluate the clinical efficacy, side effects and relapse rate of azithromycin treated typhoid fever cases in this part of the world.
2. Material and Methods
- 100 adult proven cases of typhoid fever of either sex aged between 18 and 65 years, visiting outpatient or admitted to medical ward of sri guru ram das institute of medical sciences and research,Amritsar,India, who did not took any antibiotic, were included in the study after obtaining a written consent from each patient. The serological and bacteriological criteria taken to prove the typhoid fever employed in the study were:--positive blood culture for typhoid/paratyphoid group of organisms and/or-When agglutination titre (Widal test) was 1/320 or more or-When agglutination titre was 1/160 and showed a rise subsequently along with clinical picture suggestive of enteric fever.
2.1. Exclusion Criteria
- - Patient having complicated typhoid fever (intestinal perforation, typhoid encephalopathy)- Patients, who are unable to swallow oral medicine- Patients having hypersensitivity to azithromycin.- Patient refusing consent.- Patients already on antibiotics.Before the start of therapy routine laboratory investigations like haemoglobin (Hb), total leucocyte count (TLC), differential leucocyte count (DLC), peripheral blood film (PBF) for malarial parasite, erythrocyte sedimentation rate (ESR), urine examination were done after detailed history taking, general physical examination and systemic examination. Screening chest X-ray test were done in all cases. Electrocardiography (ECG) and liver function tests were carried out as and when indicated.Widal slide agglutination test against O, H, A(H) and B(H) antigens was carried out in all cases, at the time of admission and was repeated afterwards in patients with +ve titre of 1:160. Blood culture for salmonella typhi and paratyphi was done in every case at the time of admission and repeated in cases in which fever did not respond in a week’s time after start of treatment.After sending the investigations, all patients were put on oral azithromycin. It was given in an oral dose of 1 gm on day 1 and 500 mg daily from day 2 to 7. A six hourly temperature chart was maintained in all cases.Supportive treatment including tablet paracetamol, intravenous transfusions of dextrose saline, 5% dextrose and blood were also employed in some cases as supportive measures as and when indicated. High grade fever was brought down by the aid of hydrotherapy and antipyretics. The patients were given semi-solids to liquid bland diet consisting of milk, eggs, curd, cheese, vegetable, meat soups, bread, khichri and fruit juices.The progress of the cases in the ward was recorded daily as per proforma with special reference to defervescence, general condition, bowel functions, chest signs, pulse, blood pressure and side effects of the drug were enquired for and noted. All cases were followed up weekly for a period of 4 weeks. All the cases came for follow up regularly and were examined for any sign/symptoms of relapse.
2.2. Effectiveness Parameter
- Patients were considered clinically cured when fever subsided within 7 days of antibiotic therapy and without any clinical relapse during 4 week follow up period. The following parameters were noted and tabulated-
2.2.1. Cure Rate
- Patient was considered clinically cured when fever settles within seven days of antibiotic therapy and without any clinical relapse during four week follow up period.
2.2.2. Fever Clearance Time
- The average period of defervescence of fever i.e. the average time taken from the onset of therapy to the time when fever touched to normal was recorded in all patients. The patient was considered afebrile, when the daily maximum temperature was <38°C for two days or longer.
2.2.3. Treatment Failure
- Patient was considered a treatment failure, if fever failed to settle within 7 days of treatment.
2.2.4. Clinical Relapse
- Patient was considered to have relapsed if he developed fever and other symptoms consistent with the enteric fever during four weeks follow up period.
2.2.5. Any Adverse drug Reaction
- Side effects were ascribed to the antibiotic therapy if it developed after the commencement of the treatment or within two days of completion of the antibiotic therapy. Antibiotic therapy was well tolerated in most of the patients.
3. Results
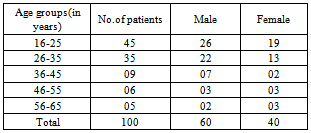
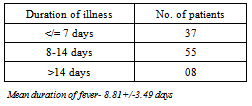
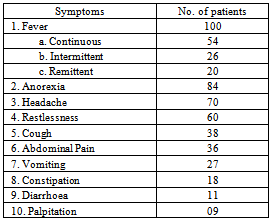
- In the present study, 100 patients of typhoid fever were included of which 60 were males and 40 were females in the range of 16-65 years with male: female ratio being 1.5:1. The maximum incidence was between the age group of 16-25 years (45%). The mean age of patients in this study was 29.41 +/- 11.93 years. [Table-1]
|
|
|
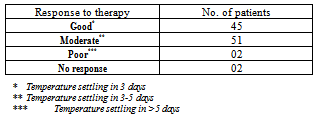
3.1. Clinical Cure
- 98 out of 100 patients were cured in this study with cure rate of 98%[Table-4].
3.2. Fever Clearance Time
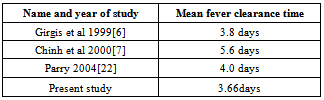
- The mean fever clearance time was 3.66+/-0.91 days in our study.
3.3. Treatment Failure
- Only 02 out of 100 (02%) patients failed to respond to antibiotic therapy in this study.
|
3.4. Relapse
- No relapse was recorded in the present study in a follow up period of 4 weeks.
3.5. Adverse Drug Effects
- Nausea and vomiting were most common side effects observed in 11 patients, while dizziness and vertigo were observed in nine patients. Abnormal liver function tests in the form of mild elevation of serum alkaline phosphatase developed in two patients.Side effects were not serious enough to withhold the treatment. No serious complication related to typhoid fever appeared during the treatment in any of the patients.
4. Discussion
- Typhoid fever is one of the commonest causes of systemic infections in India and is one of the common causes of travel associated illnesses[9]. Hospital-based studies and outbreak reports from India indicate that enteric fever is a major public health problem in this country, with Salmonella enterica serovar Typhi (S. typhi) the most common etiological agent but with an apparently increasing proportion of cases due to Salmonella paratyphi[10]. Typhoid fever carried a very high morbidity and mortality before the introduction of chloramphenicol. Chloramphenicol was introduced in 1948 as a specific bacteriostatic drug against salmonella group of organisms. Chloramphenicol remained the drug of choice for typhoid fever for more than 35 years after which resistant strains to chloramphenicol appeared[11]. Quinolones (Ciprofloxacin, Pefloxacin, Ofloxacin, Lomefloxacin, Sparfloxacin, Fleroxacin and Amifloxacin) were introduced as first line of therapy for the treatment of typhoid fever in mid eighties. However; widespread use of fluoroquinolones for typhoid fever were also followed by the emergence of S. typhi and S. paratyphi A isolates with elevated Minimum Inhibitory Concentrations (MIC) to ciprofloxacin and ofloxacin across Asia and in parts of Africa. These strains are associated with point mutations in the gyrA gene and occasionally the parC gene[12]. Typhoid fever caused by S. Typhi strains with an elevated MIC to ciprofloxacin and ofloxacin have been coupled with the failure of treatment with these antimicrobials and increased disease severity[13]. In a review done by Effa et al. comprising twenty-six studies, involving 3033 patients, concluded that the newer fluoroquinolone, gatifloxacin, remains effective in some regions where resistance to older fluoroquinolones has developed[14].Similar results were reported in a study conducted in Karach[15].Now the third generation cephalosporins are being used as first line agent for typhoid fever in many centres especially for paediatric age group. Ceftriaxone being the most frequently used 3rd generation cephalosporin for this purpose. But since it is an intravenous agent and a very costly drug, search for oral alternatives is on. There are also reports from the Indian subcontinent of isolates that are fully resistant to fluoroquinolones and the extended spectrum cephalosporins as well[16].The azalides are another class of antibiotics which have shown promise in the treatment of typhoid fever. Azithromycin, the first drug of this class, is a derivative of the basic macrolide nucleus with better activity than erythromycin against gram negative bacteria. In vitro, azithromycin has an MIC range of 4 to 16 ug/ml against S.typhi, suggesting that the drug has limited utility for the treatment of typhoid fever. However in murine typhoid model, azithromycin given once daily was highly effective in clearing the infection and this activity was attributable to the remarkable property of intracellular concentration of azithromycin in macrophages (>100 times the concentration in serum). Recent data on the use of Azithromycin in children indicate that it may be safely given as an alternative agent for the treatment of uncomplicated typhoid fever. Azithromycin has been used in recent past in multidrug resistant cases of typhoid fever . Various comparative studies have been conducted in different parts of world for MDR typhoid fever and have found efficacy of azithromycin to be comparable to flouroquinolones as well as cephalosporins [17,18].98 % clinical cure rate with no case of relapse observed in our study corroborates with similar cure rates between 91% to 100% achieved in previous studies. 100% cure rate was obtained by Girgis et al and Butler et al[6,19]. Cure rate of 91% was achieved by Frenck et al in 2000 and 94% by Frenck et al in 2004[20,21]. As noted earlier only 2 cases of treatment failure were noted in the present study pointing towards a good cure rate achieved by azithromycin in enteric fever.The observed mean fever clearance time of 3.66+/-0.91 days in our study was better than the known previous studies of fever clearance time. In other studies it has been found to be varying between 3.8 – 5.6 days. [ Table-5]
|
5. Conclusions
- In our study, high cure rate was achieved with Azithromycin with comparable mean fever clearance time and without any serious side effects. This led us to conclude that azithromycin is an effective oral agent for treatment for typhoid fever.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML