-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2013; 3(1): 1-9
doi:10.5923/j.ajmms.20130301.01
Interplay Between Quantifiable and Unquantifiable Safety Climate as Affected by Successful Systems Approach to Medication Safety Improvement:Primary Care Settings
Ranjit Singh 1, Diana Anderson 2, Elizabeth McLean-Plunkett 2, Dev Raheja 3, Gurdev Singh 4
1Associate Professor at Schools of Medicine and Management, Co-Director UB Patient Safety Research Center, UB School of Medicine, State University of New York at Buffalo, Member of WHO Expert Panel for Patient Safety in Primary Care.77 GoodellSt,Room 220R, Buffalo, NY 14203, USA
2Research AssociateUB Patient Safety Research Center, UB School of Medicine,77 Goodell St, Room 220R, Buffalo. NY 14203. USA
3Patient System Safety, 9811 Mallard Drive, Suite 213Laurel, MD 20708. USA
4Director UB Patient Safety Research Center, UB School of Medicine, Adjunct Professor UB Schools of Management and Medicine,State University of New York at Buffalo, Member of WHO Expert Panel for Patient Safety in Primary Care.77 Goodell St, Room 220R, Buffalo, NY 14203, USA
Correspondence to: Gurdev Singh , Director UB Patient Safety Research Center, UB School of Medicine, Adjunct Professor UB Schools of Management and Medicine,State University of New York at Buffalo, Member of WHO Expert Panel for Patient Safety in Primary Care.77 Goodell St, Room 220R, Buffalo, NY 14203, USA.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
The authors examine interrelation of safety attitude constructs measured with an Ambulatory Safety Attitudes Questionnaire(SAQ-A) and a successful intervention designed to reduce medication errors. This paper responds to WHO All Expert Working Group’s 2012 call to understand this interrelationship. Authors set out to measure safety attitude changes in relation to the changes in Adverse Drug Events using a cluster randomized trial in which 12 Upstate New York Practice-based Research Network practices were each randomized to one of 3 states(4 practices each):(1)Team resource management intervention based on FMEA approach;(2)Team resource management intervention with Practice Enhancement Assistants;(3) No intervention(comparison group). Combined pre- and post-intervention scores of the safety attitudes constructs were: (a)stress recognition: 62 vs 64.8, (b)perceptions of management:64.3 vs 61.5,(c)working conditions: 68.1 vs 63.9,(d) teamwork climate: 75.4 vs 72.9,(e) safety climate: 73.3 vs 75.2, and (f) job satisfaction: 78.4 vs 77.0. Despite anecdotal reports to the contrary, the efficacious TRM intervention appeared to have had no significant effects on measured safety attitudes.The authors describe limitations of the work and put forward a concept of context-sensitive culture of safety.
Keywords: Ambulatory, Attitude, Culture, Failure Modes, Medication, Primary Care, Safety
Cite this paper: Ranjit Singh , Diana Anderson , Elizabeth McLean-Plunkett , Dev Raheja , Gurdev Singh , Interplay Between Quantifiable and Unquantifiable Safety Climate as Affected by Successful Systems Approach to Medication Safety Improvement:Primary Care Settings, American Journal of Medicine and Medical Sciences, Vol. 3 No. 1, 2013, pp. 1-9. doi: 10.5923/j.ajmms.20130301.01.
Article Outline
1. Introduction
- The huge chasm that exists between the potential and the actual safety-based quality of care delivered by the health care industry is consistently wide across1,2 most of the world. The World Health Organization(WHO) has formed an ‘Alliance for Patient Safety’. According to WHO patient safety is a Basic Human Right.A most generally expressed and accepted view is that creation of culture of safety is a critical first step for healthcare organizations that aim to improve quality and safety.3-6 This approach has been embraced by the National Quality Forum.7 The Joint Commission for accreditation of healthcare organizations appropriately included an annual assessment of safety culture in its 2007 Patient Safety Goals. Agency for Health Research and Quality(AHRQ) has developed surveys for assessment of patient safety culture in outpatient and inpatient settings.It is important to point out that the WHO All Expert Working Group’s 2012 report8 calls for understanding of the relationship between safety culture and state of safety in any organization.With support of an AHRQ grant the authors set out to:1) examine the feasibility of objectively assessing the impact of a FMEA based Team Resource Management(TRM) intervention on reducing medication errors among geriatric patients in primary care settings, with and without Practice Enhancement Assistants(PEAs). At the heart of this TRM is a Safety Enhancement and Monitoring Instrument that is Patient Centred(SEMI-P).9-132) examine changes in six safety attitude constructs measured with an Ambulatory Safety Attitudes Questionnaire(SAQ-A).8,14-16The associated hypotheses were that: 1) implementing an intervention will reduce Adverse Drug Event(ADE) incidence and severity over the comparison group, 2) implementing TRM will result in measurable changes in safety culture, and 3) the Practice Enhancement Assistant(PEA) will further reduce ADEs and improve safety climate beyond the effect of TRM intervention alone.In this first section we present, very briefly, the TRM intervention and its effects on ADEs. Subsequent sections present detailed description and discussion of effects of this intervention on the safety attitudes.
1.1. SEMI-P Centered TRM
- The authors have developed a bottom up Team Resource Management(TRM) approach for not only monitoring safety hazards but also for improving patient safety in an office setting.10-13,17-19 This approach synergizes with the paradigm of complex adaptive systems and views each medical setting as a complex adaptive micro-system. The measurements that are used to identify and prioritize quality and safety problems must be trusted by the members of the system. The literature reflects scepticism regarding externally driven measures20-22 and top-down recommendations for improvements, suggesting that, in their current forms, they may not be trusted by many physicians, nurses and other staff as fair and valid measures. An alternative approach, TRM, that solicits and encourages involvement of all team members to identify and prioritize safety and quality problems has SEMI-P at its heart and is prospective.10,23 The science of observed systems is looped with that of observing systems in the development of this approach.5,24
1.2. Effects of TRM on ADEs
- Rate and severity of ADE’s and preventable ADE’s was measured using a Trigger Tool(TT)25 for the 12-month periods before and after the start of the intervention. It is useful to note that a TT is likely to uncover the largest number of adverse evenets.26 At baseline, among 1019 patients there were 341 ADE’s(33.5 per 100 patient-years), of which 39.3% were preventable. Paired T-tests using site-level rates showed that the rate of preventable ADE’s in the TRM intervention with PEA group was significantly lower after the intervention than before(11.0vs 15.9 per 100 patient-years, p=0.042). Preventable ADE’s most commonly occurred during prescribing and administration of medications.The most common triggers as well as the largest contributors to ADE’s and to preventable ADE’s were: medication discontinuation, unplanned hospitalization, and emergency department visits.Among preventable ADE’s•38% were deemed to have minimal or no clinical effect(e.g., abnormal lab with no symptoms)•30% were classified as “Severe”(resulting in either hospitalization, permanent disability or death)The conclusion drawn from this part of the study was that the TRM intervention(when enhanced by a PEA) appeared to affect a significant improvement in medication safety.
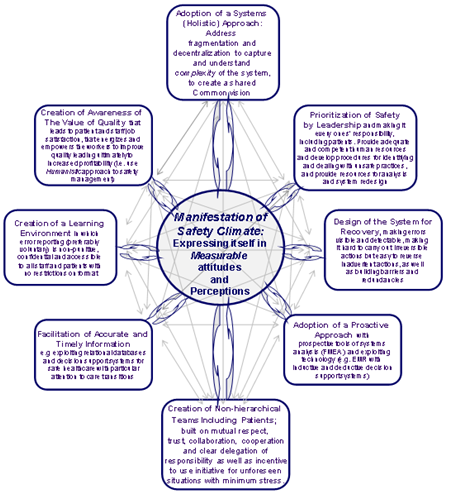
1.3. Rationale and Background to the Constructs Safety Culture, Climate and Quantifiable and Unquantifiable Attitudes
- Definitions of organizational and safety culture abound in the literature.27,28 These constructs aspire to help analytical reasoning and practical research. It should be acknowledged that the causes and effects of an organization’s safety culture are intertwined. A highly reliable organization ‘has’ a safety culture and ‘is’ a safety culture, wherein the objective of cultivating this culture is to continuously enhance safety, advisedly, with self-empowered and motivated teams.10 It is also helpful to acknowledge and treat each ambulatory practice(organization) as a unique and complex adaptive micro-system.19 In the paradigm of complex adaptive systems, a culture of safety not only functions as a conceptual model but also as a ‘central attractor’ bringing order in disorder(i.e. reliability where there was risk).17,27 It is interesting to note that a study by Quinn et al.29 showed that physicians from practices that were involved in the evaluation of QI activities had significantly less isolation, stress, and dissatisfaction. In broad terms, climate can be seen as the observable part of culture. Safety attitudes in turn are a subset of safety climate; they are the part of the climate that resides in individuals and may, therefore, be measurable via self-administered surveys. But it should be remembered that attitudes too are very impressionable and complexly dynamic. Figure 1 portrays the dynamic conceptual relationships between the different constructs.Figure 2 portrays a framework that attempts to clarify the contributors to safety culture and the relationship of culture to climate and attitudes. This figure shows eight factors that, in our view, contribute to a safety culture.14 Although the relative importance of these contributors(and potentially others not identified in this framework) are not well understood at this time, it is important to note that each of these contributors interacts with and influences every other contributor(see narrow arrows); they worksynergistically to create a culture of safety. This culture is complex and hyper-dimensional and is the result of complex interactions between multiple players and their beliefs, attitudes, and behaviours over time.
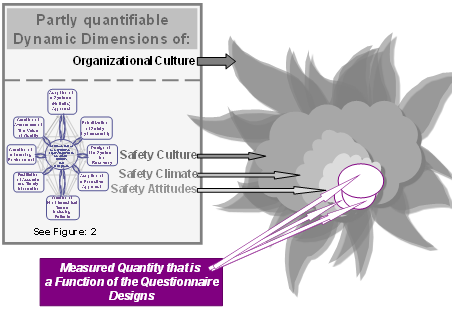 | Figure 1. Conceptual Dynamic Relationship between Various Constructs |
2. Objective
- The objective of the study presented in this paperwas to measure safety attitude changes in relation to the changes in ADEs by examining changes in the following safety attitude constructs as measured with a 30 item Safety Attitudes Questionnaire(SAQ-A):a)stress recognition d) teamwork climateb)perceptions of management e) safety climatec)working conditionsf) job satisfaction
3. Methods
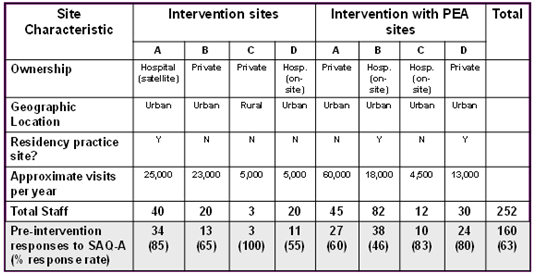
- Table 1 shows the characteristics of the sites studied. This was a cluster randomized trial in which 12 Upstate New York Practice-based Research Network practices were each randomized to one of 3 states(4 practices each):(1) Team resource management intervention;(2) Team resource management intervention with PEA;(3) No intervention (comparison group).All staff at the intervention sites were invited and encouraged to participate in TRM and respond to SAQ. The intervention period was 12 months.The study protocolwas approved by the Social and Behavioural Sciences Institutional Review Board.
|
3.1. Implementation
- The SAQ-A was administered voluntarily and anonymously to all eligible staff at 8 primary care offices within the Upstate New York Practice-Based Research Network. To be eligible, staff had to have worked at the office(full- or part-time) for at least one month prior to survey administration. As shown in Table 1 the characteristics of the practices ranged from a rural solo practice to an urban academic residency practice site. The main part of the survey consisted of a series of statements that respondents rate according to a 5-point Likert scale(1 = disagree strongly, 2 = disagree slightly, 3 = neutral, 4 = agree slightly, and 5 = agree strongly). Respondents could also indicate that an item was ‘Not Applicable.’ The survey took approximately 10-15 minutes to complete. Most surveys were distributed in person at brief informational meetings accompanied by a concise explanation of the purpose of the survey, instructions for completion, and assurances of anonymity. For those employees unable to attend the informational session, materials were left with brief written instructions. To help maintain anonymity and confidentiality, participants were instructed to refrain from placing any identifying information on the survey; a secure drop-box was provided for completed questionnaires. Surveys returned within two weeks were included in analysis.
3.2. Analysis
- In keeping with the analytic technique of the originators of the SAQ, calculation of safety attitudes for each of the six safety factorswas performed by converting results from categorical to continuous variables as follows: Strongly disagree=0, Disagree=25, Neutral=50, Agree=75, and Strongly Agree=100. Some items were reverse scored so that a higher score always represents a more positive attitude. For each respondent, a mean score of ≥ 75 for the items in a particular factor denotes a “positive safety attitude” for that factor. Survey data were analyzed using SPSS, version 14.0(SPSS Inc., Chicago, IL).
4. Results
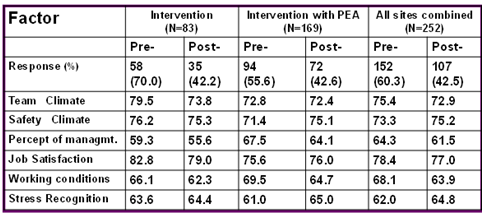
- Table 2 shows the 30 item questionnaire response rates and mean scores on the six attitude subscales at the start and after 12 months of TRM intervention. Comparison of post versus pre data by ANOVA showed no significant differences with or without PEA despite anecdotal reports from multiple sites of improvement in attitudes as measured by SAQ-A.
|
5. Discussion
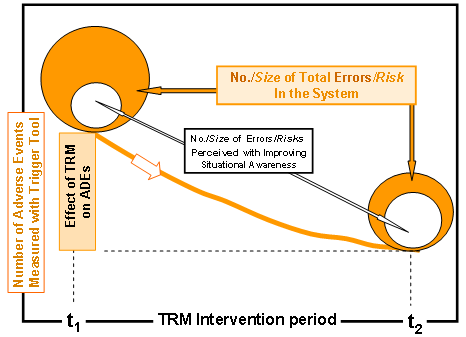
- The theoretical framework described in Figure 2 includes several contributors to safety IT. Some of these contributors can be mapped to measurable attitudes, many of which are covered by the SAQ and SAQ-A. For example, ‘Creation of a Learning Environment’ maps very closely to the SAQ’s Safety Climate scale, ‘Creation of Non-hierarchical Teams’ corresponds to Teamwork Climate, Job Satisfaction, and Stress Recognition in the SAQ, and ‘Prioritization of Safety by Leadership’ is an area that is well addressed via the Perceptions of Management and Working Conditions scales. The framework reveals some areas that could be addressed further, such as ‘Design of the System for Recovery’ and ‘Adoption of a Proactive Approach’ that are not explicitly covered by the SAQ. It should also be recalled that all these 8 contributors manifest in complex multidimensional ways, some of which are either not measurable or require methods of assessment other than self-administered surveys. In an effort to explain absence of direct correlation between reduction of ADEs due to TRM intervention and no significant change in measured safety attitudes, we have visualized threshold effects of TRM intervention, combined with concurrent administration of SAQ-A, on the dynamic interplays between total state of safety, perceived state of safety, the various constructs of culture/climate/attitudes, and the ADEs. Figure 3 portrays the conceptual interplay, over a 12 month intervention period(t1 to t2), between the beneficial effect of TRM on ADEs and:(1) changes in total number of possible errors or total risks, and(2) changes in perceived number of errors or total risks. These relative changes are assumed to be due to improved situational awareness due to the formative effects of TRM and SAQ-A and the normative/summative effects of TRM. It is helpful to note that a number of studieshave shown that increase in error reporting can accompany overall safety improvements in a setting. A 2009 Report by AHRQ41 found that “hospitals with improvements over time in non-punitive response to error had slight increases in event reporting.”
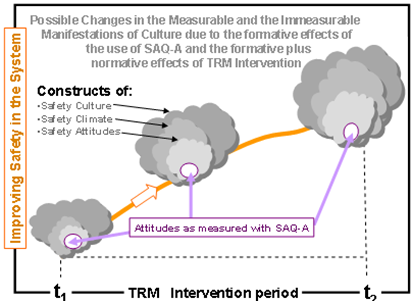 | Figure 4. Interplays between the improvement in medication safety and the constructs of safety culture, climate, and the measured attitudes |
6. Conclusions
- 1. At baseline SAQ-A revealed significant differences in safety attitudes between sites, attesting to the uniqueness of each setting.2. Five of the six subscales had reasonable internal consistency-reliability in primary care offices but some performed poorly with some subgroups. Further work is needed to evaluate and refine the instrument for these settings.3. Combined pre- and post-intervention scores of the safety attitudes constructs were: (a)stress recognition: 62 vs 64.8, (b)perceptions of management:64.3 vs 61.5, (c)working conditions: 68.1 vs 63.9, (d) teamwork climate: 75.4 vs 72.9, (e) safety climate: 73.3 vs 75.2, and (f) job satisfaction: 78.4 vs 77.0. Despite anecdotal reports to the contrary, the efficacious TRM intervention appeared to have had no significant effects on safety attitudes as measured by SAQ-A.4. Measurement of safety culture and climate in healthcare is still a relatively immature stage of development and there is need to further develop and construct theoretical models that are sensitive to the nature of healthcare environments.5. The concept of context-sensitive culture of safetyis,therefore,worthy of further development.6. It may be worth considering use of the recently developed AHRQ 12-dimensioned “Medical Office Survey on Patient Safety Culture” in future studies.7. Our work responds to WHO All Expert Working Group’s 2012 call to understand this interrelationship between safety culture and a successful intervention designed to improve safety.
6.1. Limitations
- •Small number of sites•Modest response rates(esp. post-intervention)•Lack of a control group•Confounding factors •Changes in management, staff turnover, etc.•Limitation of the measurement tool•Some aspects of safety climate not covered•Some issues not amenable to this approach•SAQ-A is a formative tool; confounding the “before and after” comparisons, e.g., people’s threshold for agreement may change.
ACKNOWLEDGEMENTS
- Authors are grateful for AHRQ Grant:1R21HS014867-01A1; Improving Geriatric Drug Safety in Underserved Practices.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML