-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2012; 2(5): 89-95
doi: 10.5923/j.ajmms.20120205.01
Quality of Life after Cardiac Rehabilitation for Patients with Heart Failure: 18 months follow-up
Elias F. Porto 1, Claudia Kümpel 1, José R. Leite 2, Aline A. Andrade 1, Natália C. Oliveira 3, 4, Leslie A. Portes 1, 3, 4
1Physical Therapy Department, Universitary Clinic, Adventist Univesity of São Paulo (UNASP), Brazil
2Clinicas Hospital from University of São Paulo Medical School, Brazil
3Exercise Physiology Laboratory (LAFEX-UNASP), São Paulo, Brazil
4Physical Education Department, Adventist University of São Paulo (UNASP), Brazil
Correspondence to: Leslie A. Portes , Physical Therapy Department, Universitary Clinic, Adventist Univesity of São Paulo (UNASP), Brazil.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
The aim of this study was to evaluate the effects of a supervised cardiac rehabilitation (CR) program on long-term quality of life (QoL) of patients with heart failure (HF).Methods: A sample of 21 HF patients, previously sedentary, NYHA II, was randomly divided into two groups: the CR group (N = 13) and the control group (CG = 8). The CR consisted of sessions of 120 minutes/day, 3 times/week,for 60 days. CR group performed their activities under supervision at a rehabilitation clinic, and CG received standard care and was instructed to exercise at home. All patients underwent a maximal symptom-limited test at the beginning and after 30 and 60 days of CR. QoL was monitored after 60-days, 6, 12 and 18 months of CR. Results:Two-way ANOVA for repeated measures, followed by Tukey’s test for statistical analysis showed significantimprovement in peak VO2 at 30 and 60-days of CR (p<0.05). QoL improved after 60-days of CR and remained improved throughout the 18following months in the supervised CR group. The use of hospital emergency services became less frequent (p=0.023) and there was a trend for better survival after 18 months of follow-up (p=0.092).Conclusion: CR was effective upon cardiopulmonary and QoL aspects.
Keywords: Heart Failure, Cardiac Rehabilitation, Functional Capacity, Quality of life, Survival
Article Outline
1. Introduction
- Heart Failure (HF) is, in most of the cases, a status due to the evolution of a number of illnesses, such as arterial hypertension or high blood pressure, coronary heart disease (CHD), acute myocardial infarction (AMI), valvediseases and cardiac arrhythmic illnesses[1,2]. The main HF symptoms are dyspnea, physical activity intolerance and quality of life reduction[2,3]. HF represents the main cause for hospital admission in individuals aging 65 and beyond. It is a fact that HF prevalence is increasing, and among the factors that might be contributing to this situation we highlightthe increase in life expectancy of the general population and greater effectiveness of new drugs[4]. However, despite the advent of new drugs, mortality and morbidity indexes are still high in this type of affection[1,2]. Cardiac rehabilitation (CR) has become mandatory in HF patients. Objectives of CR include mortality and morbidityreduction, quality of life improvement and cos reduction[5-13]. Several studies have already demonstrated the efficacy of exercise - based CR programs[7-11], but a meta - analysis of randomized controlled trials[12] has concluded that quality of life improves to similar levels in patients receiving CR and standard care.The aim of the present study was to evaluate the effectiveness of asupervised CR program in the quality of life of HF subjects, as compared to standard care. Success indicators were based on cardiorespiratory capacity analysis, functional capacity, quality of life, survival and/or mortality.
2. Methods
- The present study was based on a longitudinal prospective design composed by two phases: 1st-supervised CR or non-supervised CR (control) for 60 days; and 2nd- 18 months follow-up after CR. All procedures in the study were in conformation with resolution 196/96 of the Brazilian Health Council(http://conselho.saude.gov.br/resolucoes/1996/Reso196.doc) and the declaration of Helsinki[14], and were approved by the local University ethics committee (protocol number: 004/2005).
2.1. Patients
- After discharge from hospital, 28 male patients volunteered to participate in the study. They were randomly distributed into two groups: CR (n = 16) and CG(n = 12). Random distribution was performed as follows: for each participant that enrolled the study, researchers drew out a number from a box (1 or 2), and this consequently led to different group sizes.
2.2. Selection Criteria
- At the beginning of the study, we excluded from our sample subjects in whom the following incidents had occurred less than three months ago: myocardial infarction, ischemic myocardial manifestation,unstable angina anduncontrolled high blood pressure. We also excluded subjects who were physicallyactive before the cardiovascular event, the ones who were physically impaired due to brain vascular disease,orthopedic or rheumatologic limitations, and individuals with lack of availability to participate. After being adequately informed about all the procedures in the study, all subjects signed aninformed written consent. Twenty-one out of 28 patients concluded the CR program, 3 patients were excluded from CR and 4 from the CG. Patients were excluded because of cardiac arrhythmia (n = 2), because they did not take personal medication adequately (n = 2) one of themreferring sporadicangina pectoris, and 3 were excluded because of lack of availability to participate in the study. Final group numbers were 13 subjects in CR and 8 in CG. All 21 patients had New York Heart Association functional classification II (NYHA II)[15]. These individuals had clinic and hemodynamic stability according to the “American Heart Association”[13,15]and had not been hospitalized 6 months previously to the beginning of the study. All of them were instructed not to suspend medication intake during the study period, except by medical prescription.
2.3. Cardiopulmonary Evaluation
- Patients underwent cardiopulmonary tests in 3 distinguished moments: one week before initiating participation, 30 days and 60 days after the beginning of the study. Metabolic measures were obtained by means of K4b2 Cosmed®gas analyzer, model CO9052-02-99 (Rome, Italy).Throughout the tests,electrocardiographic trace (ECG) and peripheral oxygen saturation(SpO2) were constantly monitored; and arterial blood pressure was measuredevery 3 minutes. Dyspnea sensation was also verified every minute using Borg scale[16,17]and ventilation and metabolic variables were acquired breath by breath. All tests were carried out on a treadmill protocol according to maximum test symptom limited[17]. Treadmill speed was chosen for each patient and was maintained unaltered until the end of the test. During the first three minutes of the test the treadmill inclination was zero and from the fourth minute onwards the treadmill inclination increased by 1% every minute until the end of the test[16,17]. The duration of incremental test should be between 8 and 12 minutes. When the test lasted less than 8 or more than 12 minutes, a new test was performed the next day. The speed of the treadmill was based on the evaluator’s experience.
2.4. Training Protocol
- CR and CG patients were accompanied by a professional team during the study period. CR performed approximately 20 minutes of upper and lower limbs calisthenic exercises. After that, patients walked for 30 minutes on the treadmill, with inclination being adjusted at moment zero and maintained until the end ofthe training session. Regarding speed, the first three and last five minutes were set at 1.6 km/h for warm up and cool down, respectively. The intermediate 22 minutes were effectively dedicated to training with customized load. Heart rate was continuously monitored during training by a Polar® heart rate wrist monitor. SpO2, breath rate and dyspnea sensation were also observed. In case of SpO2≤ 88%, enough oxygen through nasal catheter or Venturi mask was given to the patient to maintain SpO2≥ 92%. CR program period was 60 days, 3 times a week, 120 minutes/session, divided into10 minutes of stretching exercises, 20 minutes of calisthenic exercises, 3 minutes of warm-up in treadmill, 22 minutes of treadmill exercise as described above, 5 minutes of cool down, 20 minutes of stretchingexercises and the last 30 minutes were dedicated to rest before being dismissed to go home. Treadmill training load was individualized,based on initial cardiopulmonary test. Exercise intensity was set to maintain HR between 60% and 70% of the maximum obtained in the test.Throughout the training, due to the individual’s physical capacity improvement, perceived by decrease indyspnea and a better well-being sensation, thepercentage of the training load was increased up to 80% maximum HR limit.Patients of CG received standard care: orientation regarding benefits promoted by physical activities and the necessity and importance that all individuals performed the proposed activities regularly. Subjects received instructions to exercise3 times/week, 120 minutes/sessionduring 60 days. Patients should walk for30 minutes in a rhythm that was enough to keep their HR between 60% and 70% of maximum. Besides that, patients received instructions on how to perform warm upand back to rest activities. To do so, all patients received a Polar® heart rate monitor and received instructions regarding HR intensity and monitoring. Every CG patient was informed about how to complete calisthenic exercises. All patients were required to complete a diary log with the number of daily training hours, and to take notes of possible unexpected events during the walking sessions.Once a week, patients of both groups attended educational lessons about themes such as tobacco, alcoholism, high blood pressure, diabetes mellitus and proper use of medicine. Both groups were giventhe schedules in advance for all of the lectures.One day before each class all patients received phone calls reminding them of the rehabilitation center visit.
2.5. Quality of Life and Symptoms Evaluation
- Symptoms and quality of life were evaluated by using the Minnesota Living with Heart Failure Questionnaire (MLwHFQ)[18]applied at the beginning, after 60 days, 6 months, 12 months and 18 months of follow-up. The MLwHFQcontains 21 questions, each one with 6 alternatives to choose from: no, very little, little, more or less, much and very much; with “no” corresponding to zero and “very much” matching5. Finally, the number of hospital admissions, emergency room attendances and mortality were evaluated monthly.
3. Statistical Analysis
- Results are described as mean ± standard deviation. Initially, groups were compared by the non-parametric Mann-Whitney test. The excluded patients’ data was compared to the ones of those who completed the study by the Wilcoxon test. Two-way ANOVA for repeated measures was adopted, followed by Tukey’s test for comparisons between CR and CG, considering the following factors: exercise training program (CR versus CG) and time (beginning, 30 days, 60 days, 6, 12 and 18 months follow-up). Mortality was evaluated according to the Kaplan-Meier method[5]. Analyses were made by SigmaStat3.5 (www.Systat.com). In all cases, statistically different results were taken into account if p < 0.05.
4. Results
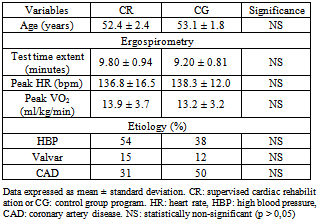
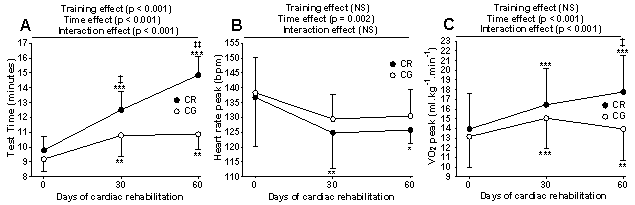
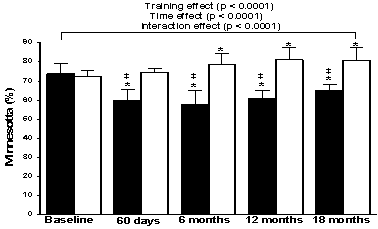
- Data from the 21 patients who completed the intervention protocol did not differ statistically from the 7 patients who were excluded from the study (data not presented). TABLE 1 shows both study groups results before CR. No statistically significant differences were found between CR andCG regarding age, maximum testtime length, peak heart rate (peak HR), peak VO2 and most frequent cardiac insufficiency aetiologies (high arterial blood pressure, valvedisease and acute myocardial infarction). Ninety-two percent of CR patients performed all sessions proposed. Although all patients in the control group received phone calls and encouragement to accomplish the physical activities proposed, only 16% performedthe activities as recommended, 35% performed them partially and 49% did not perform the activities as recommended.FIGURE 1A illustrates results relative to maximum amount of time on treadmill test for the two study groups. CR and CG patients were compared initially at 30 and 60 days of their respective programs. Statistically significant influences were observed regarding the program (CR versus CG) and the interaction (program plus period of time) in relation to time length of maximum test. The influence of time (beginning versus 30 versus 60 days) was observed in CR group (beginning < 30 days < 60days, p < 0.001) and inCG (beginning < 30 days = 60 days, p < 0.004). FIGURE 1B illustrates results relative to peak heart rate (peak HR) for both study groups. Statistically significant differences regarding time were observed only in CR group (beginning > 30 days = 60 days, p < 0.027). Values obtained fromCG (beginning = 30 days = 60 days, p > 0.05) were not significantly influenced by the amount of time required for the test to be performed, and in the same way there were no significant differences between CR and CG in each moment throughout the programs. FIGURE 1C illustrates peak VO2 results for both study groups. Statistically significant influences of time were observed in both groups: CR: beginning< 30 days < 60 days (p < 0.001); CG: beginning < 30 days > 60 days (p ≤ 0.008). When comparing groups it was noticed that at 60 days CR peak VO2values were significantly higher than CG (p = 0.027). Additionally, rehabilitation programs did not result in patients’ functional classification change.
|
5. Discussion
- The supervised CR program proposed in this study was effective and efficient, as seen by the high patient adherence in the proposed sessions (92%), by the success in all of the proposed activities, cardiopulmonary improvement, symptoms reduction and quality of life improvement. On the other hand,control patients,which received standard care,justshowed improvement in the first 30 days in peak VO2 and maximum test time length, and at 60 days in physical capacity, probably because of the low adherence to standard care verified in this group (16%).
5.1. Supervised Program Effects
- In general, supervised CR programs are successful in increasing physical fitness, cardiovascular performance, quality of life and reducing mortality[5-13,19-21,22-24].However, there are indications that only 11% to 30% of those who need CR have access to specialized centers[6,22,23,25].Taking these facts into consideration, there has been an increase in the number of programs, whether supervised or not. The effectiveness of these programs has been well documented, revealing broad benefits[19,23,26-28],although other studies have failed to observe positive effects, especially those regarding quality of life[29].In the present study, patients with HF in both groups demonstrated improvement in cardiorespiratory fitness and in functional capacity during the 60 intervention days, as verified by other authors[19-21,23,26-28].Nevertheless, only the supervised CR group showed quality of life improvement along the 60 CR days. As in other studies[30,31],quality of life benefits in CG patients were very discrete, likely because of low program adherence to standard care recommendations (16%), negatively influencing the results in this group.Some reasons may be highlighted for the benefits observed in CR program: motivation on behalf of the supervised program patients for attending a CR sector (department), specialized professional supervision, encouragement offered by the therapists during sessions, quality of service offered and social bonding with other patients in CR sessions. The differences verified when comparing both programs draw attention to the importance of the quality of the program offered, CR program adherence and adequate patient support[7,8,10,23,26,30,31].
5.2. Cardiorespiratory Effects
- Traditionally, maximum oxygen consumption (VO2 max) is a determiner for individuals’ physical and functional capacity. It is known that adequately planed intensity, time length and frequency of physical activities are the onlyeffective ways to improve VO2 max. This phenomenon is related to better cardiovascular and respiratory performance, higher muscular blood flow and greater number of mitochondria involved in aerobic metabolism[11,12,20].Studies indicate a 10% to 50% increase in VO2 max after CR program execution [5,6,11,21,30].Our results are similar to the ones cited - 18% peak VO2 max improvement in CR and 15% in control patients - indicating the effectiveness of our program.
5.3. Quality of Life
- During the 60 days of the program, none of the patients had any cardiac episode, nor needed medication change. On the routine medical appointments, in general, patients referred better well-being sensation due to CR. These results are in consonance withthe benefits verified in cardiorespiratory and functional capacity, and on the quality of life evaluation categories (in CR), as foreseen by other authors[31].Throughout the 18 months follow-up period,quality of life category improvement was only verified in CR. It is very likely that cardiorespiratory and functional capacity improvements in consequence of regular physical activity practice produced better physical performance scores for daily life activities execution and subjective health perception. These results are consistent with other studies[6,7,10,26-28,32]and emphasize the importance of having exercise training programs for quality of life improvement in HF patients. Nevertheless, there are evidences that contradict these arguments. Wijkstra[33],for example, did not find significant correlation when comparing physiologic data and quality of life in patients submitted to rehabilitation, although they observed parallel improvement in those patients. In Pell’s review[29],the author did not find significant rehabilitation program benefits on patients’ quality of life. This matter is still under debate.
5.4. Hospital Admission and Mortality
- Broad evidences endorse that CR is responsible for significant mortality reduction from all causes,from cardiovascular diseases, re-infarction and re-hospitalization[1,2,5,6,7,10,21,29,31].These reductions are related to the functional and cardiorespiratory improvements, risk factors reduction and lifestyle improvement. In the present study, hospital admittance and death indexeswere lower in the supervised exercise training group, although these differences did not reach statistical significance. Merely the emergency service frequency use in CR group was significantly lower than CG at the end of 18 months follow-up. This perceptible contrast with the studies mentioned above may be caused by the small sample, as demonstrated by others[29].Nonetheless, hospitalization reduction as well as emergency services can favorably affect costs in HF treatment, emphasizing CR treatment[2,5,6,7,10,23,24].These findings bring about at least two new questions: 1st- Which aspects are necessary to increase adherence to unsupervised CR programs? 2nd- Which strategies should be adopted to extend the benefits found in short term programs?
5.5. Limitations
- The present study has a few limitations. First, the fact of only having male subjects limits the conclusions drawn from the study. Secondly, the reduced number of patients in each group and the fact that they were sent by a single medical service,also limitsthe extent of our conclusions.
6. Conclusions
- The results of the present study allow us to conclude that a well-designedsupervised cardiac rehabilitation program is efficient and effective for heart failure patients. Cardiorespiratory fitness, functional capacity and quality of life improvementshave occurred.Reduction in the need of emergency treatment and increase in survival in these patients were also observed, both duringthe treatment program, and also in the 18 months follow-up period. These data are related to patient adherence and to the intrinsic benefits of supervised cardiac program rehabilitation.However, further research is still necessary to investigate ways to increase adherence to unsupervised CR programs, as most patients do not have access to specialized centers.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML