-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2011; 1(1): 23-27
doi: 10.5923/j.ajmms.20110101.04
The Impact of Incubators on Noise Transmission Produced by High-Frequency Oscillatory Ventilator Inside the Neonatal Intensive Care Unit
H. Salama , A. Azzam , S. A. Omar , K. Abdulhadi
Women’s Hospital, Department of pediatrics, Hamad Medical Corporation, BO box 3050
Correspondence to: H. Salama , Women’s Hospital, Department of pediatrics, Hamad Medical Corporation, BO box 3050.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Use of HFOV is a common practice inside the neonatal intensive care unit (NICU). There is a concern regarding the level of noise produced by HFOV inside the NICU. Objective: To evaluate and define the noise intensity produced by the high-frequency, oscillatory ventilator sensormedics (HFOV) and the impact of the incubator on the transmission of noise in different places inside the NICU. Methods: Using a noise analyzer, the noise produced by the HFOV sensormedics was measured in two setups: inside a quiet room, and inside the NICU during working hours. Measurements were repeated 2 times: first, inside and outside the tested incubator, second, inside and outside the next incubator. No human newborns were involved in the study; instead, a mannequin was used to simulate a newborn. The noise analyzer was placed next to mannequin mouth while inside the incubator and midway between the mannequin and the ventilator while measurements were taken outside the incubator. Each measurement was recorded against different HFOV ▲P and different frequency settings. Each measurement set lasted five minutes, where the highest and lowest readings were recorded every minute, and the average value of noise intensity was calculated.
Keywords: Noise, NICU, HFOV, Incubator
Cite this paper: H. Salama , A. Azzam , S. A. Omar , K. Abdulhadi , "The Impact of Incubators on Noise Transmission Produced by High-Frequency Oscillatory Ventilator Inside the Neonatal Intensive Care Unit", American Journal of Medicine and Medical Sciences, Vol. 1 No. 1, 2011, pp. 23-27. doi: 10.5923/j.ajmms.20110101.04.
Article Outline
1. Introduction
- HFOV sensormedics 3100 is a legendary respirator and it formulates the vast majority of the evidence-based medicine addressing HFOV in newborn infants over the last 20 years. Despite the efficiency of this respirator in ventilating the lung it is clear to those physicians came across working with this machine that it produce significant noise that can be easily recognized when approach the intensive care room. Noise is an unattractive and unfavorable sound. Sound is a vibration in a medium, which is usually air. The loudness of sound is measured in decibels (dB). Most of our knowledge about the damage to people from noise comes from studies of people with occupational exposure to sound. The standard for a workplace is to disallow more than eight hours of exposure to 90dB, four hours to 95dB, two hours to 100dB, and no exposure allowed to continuous noise above 115dB or impulse noise above 140dB. For the protection of the public health, the US Environmental Protection Agency has proposed a DNL (Day Night average sound Level) of 55dB during working hours, and 45dB during sleeping hours inneighborhoods, and 45dB in daytime, and 35dB at night time in hospitals (1).Noise may damage auditory functions for fetuses and newborns. Additionally, many pregnant women are exposed to noise in the workplace (2,3,4), causing the American Academy of Pediatrics to issue a statement in 1997 which reviewed accumulated evidence that updated the affects of noise on pregnant women, since the previous report was published in 1974. This new report addressed the concern that fetuses and newborns exposed to excessive noise may suffer noise-induced hearing loss and other health effects (5, 6). In one study, Surenthiran et al demonstrated that the proximity of the post-nasal space to the inner ear is enough to allow noise to be transmitted, and may cause cochlear damage, and therefore hearing loss in infants receiving the higher flow rates CPAP (7). Furthermore, Berens et al addressed concerns about the level of the noise produced by HFOV equipment inside pediatric intensive care units (8). While using HFOV is common practice inside a NICU, and despite the high noise levels produced by the HFOV machine itself (9), there is little information available on the magnitude of the noise levels produced by the HFOV within different NICU setups.
2. The Objective
- To describe the noise level produced by the HFOV sensormedics™ machine inside the neonatal intensive care environment and the effects of the incubator on reducing or augmenting the noise produced.
3. Methods
- This is a non-clinical observational trial, conducted in February 2010, and lasted one month inside the neonatal intensive care unit of Women's Hospital, Hamad Medical Corporation in the State of Qatar. The intensive care unit consists of 28 intensive cots, located inside two large halls which are connected by a 3-meter-wide, imaginary door. The rest of the unit is composed of three separate, large halls that constituted intermediate care.
4. Patients
- There were no human subjects involved in this trial. The measurements were conducted in one of the large halls, and no special arrangements for noise were taken during measurements inside the NICU. While special attention was taken inside the quiet room to limit the noise level during recording, the noise intensity and the test was performed after working hours.
5. Equipments
- T HFOV Sensormedics 3100A Yorba, Linda CaliforniaTM. Incubators: Ohmeda Omnibed GiraffeTM double walled. Noise analyzer: Monarch™ sound level meter.The noise analyzer measured the noise intensity (loudness) at two different locations. Location (1) is inside one of the NICU large halls during the weekday (9–12am). Location (2) is inside a quiet room that was formerly the respiratory therapy equipment room when the test was conducted after working hours. Noise measurements: Figure 1A. Quiet Room: three sets of measurements were taken before and during the HFOV:1. Measurement 1: Inside the incubator. A microphone was placed at the nearest point to the mouth of mannequin.2. Measurement 2: Immediately outside the incubator adjacent to the HFOV 3. Measurement 3: Inside the neighboring incubator (2.5-meter distance).B. Daytime NICU: three sets of measurements were taken before and during the HFOV was in operation: 1. Measurement 1: Inside the incubator. The microphone will be placed at the nearest point to the mouth of mannequin (Picture 3-a).2. Measurement 2: Immediately outside the incubator, adjacent to the HFOV.3. Measurement 3: Inside the neighboring incubators (2.5-meter distance).C. HFOV Settings: The measurements were completed at different frequencies and amplitudes, with the highest amplitude (delta ▲P) at 50, and the lowest frequency was 7.D. Noise Analyzer: The analyzer measured both loudness (dB) and frequency of noise level.E. Two persons were included in the measurements. One person was assigned to record the noise level and adjust the HFOV settings. The other person was assigned to observe and record the noise level using the noise analyzer.F. Each Measurement lasted five minutes, and recorded the highest and lowest readings at one minute intervals.G. The mean noise level was considered after five minutes of observation.
6. Results
- Inside the tested incubator: The base line noise level before test start was 50dB and 45dB inside the tested incubator in both NICU and quite room respectively. The mean noise level recorded inside the NICU and the quiet room was 84(±5) dB and 78dB (±2) respectively. These levels were recorded inside the tested incubator, with HFOV settings at a frequency of 7Hz and ▲P of 50. The noise records were progressively reduced as HFOV ▲P decreased to reach to the lowest records (78dB inside NICU and 70dB inside quite room), at ▲P of 20 and a frequency of 15 inside the NICU and inside the quiet room, respectively (Table 1) and graph 2Outside the tested incubator: The mean measured noise level was 67(±2) dB in the quiet room, and 77dB (±5) inside the NICU during a normal working day. Neighbor incubator: The mean records inside the incubator were 56dB in a quiet room, and 63dB inside the NICU. The mean records outside the incubator were (63dB (+-2) in a quiet room, and 63dB (±4) inside the NICU) (Tables 1, Figure 2&3).
7. Conclusions
- The NICU is a place where humans and technology come together to produce a unique and sometimes unbearable level of noise that can cause a significant level of discomfort. Noise has been a major concern among neonatal environmentalists, who are concerned about the outcome of noise intensity in sick, newborn infants. One of the new advanced technologies introduced to neonatal practice is the HFOV of different types. In this observational, in-vitro study, we demonstrated that the noise produced by a popular HFOV machine (sensormedics) was considerably high enough to cause major concern (86dB) inside the NICU.Only two papers address noise produced by HFOV, and both were conducted in a non-NICU setup. In this observation, we tried to document detailed information about the noise level at different settings.
 | Figure 1. Measuring method of the noise. |
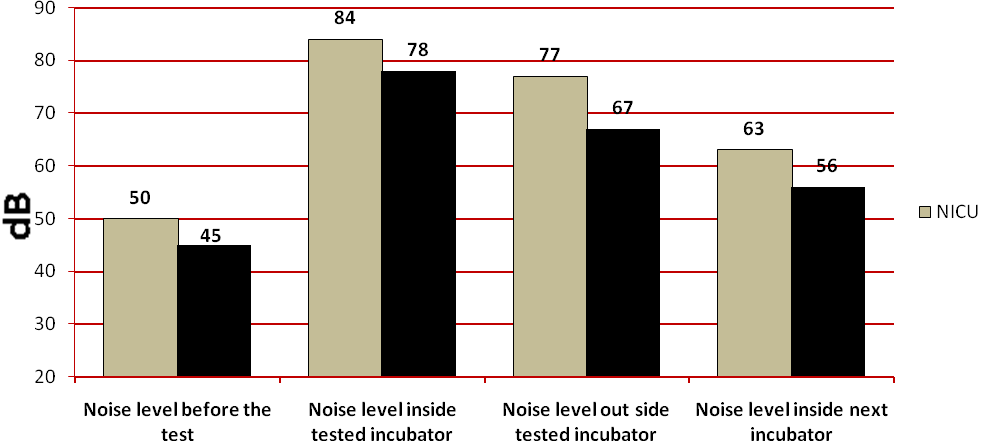 | Figure 2. Comparing highest recorded noise level before the test and during the test. |
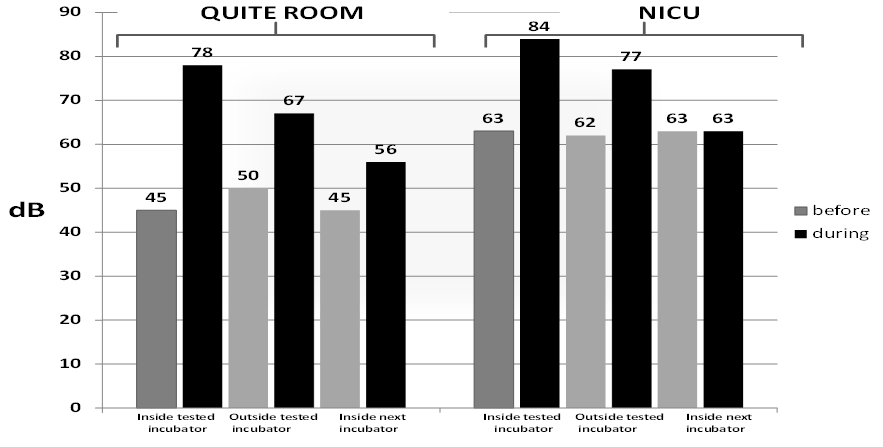 | Figure 3. Overall highest recorded noise level in different locations before and during HFOV. |
References
| [1] | Environmental Protection Agency, Office of Noise Abatement and Control. Information on levels of environmental noise requisite to protect Public Health and welfare With an Adequate Margin of Safety (Report No. 5509-74-004). Washington, DC: Government Printing Office; 1974 |
| [2] | Kam PC, Kam AC, Thompson JF. Noise pollution in the anaesthetic and intensive care environment. Anaesthesia. 1994; 49:982–986 |
| [3] | Rudolph L, Forest CS. Female reproductive toxicology. In: LaDou J, ed. Occupational Medicine. Norwalk CT: Appleton & Lange; 1990:275–287 |
| [4] | Paul Med. Occupational and Environmental Reproductive Hazards. A Guide for Clinicians. Baltimore. Williams & Wilkins; 1993: xviii |
| [5] | Noise: A hazard for the fetus and newborn committee on environmental health. American academy of pediatrics. Pediatrics vol. 100 No. 4 October 1997, pp. 724–727 |
| [6] | American academy of pediatrics, committee on environmental hazards noise pollution: neonatal aspects. Pediatrics. 1974; 54:476–479 |
| [7] | Surenthiran S S, Wilbraham K, May J, Chant T, Emmerson A J B, Newton V E. Noise levels within the ear and post-nasal space in neonates in intensive care. Archives of Disease in Childhood – Fetal- Neonata Edition 2003;88: F315-F318; doi:10.1136/fn.88.4.F315 |
| [8] | Berens R J. Noise in the pediatric intensive care unit. Journal of intensive care medicine vol 14 Issue 4, Pages 118–129 |
| [9] | Hoehn T, Busch A, Krause M. F. Comparison of noise levels caused by four different neonatal high-frequency ventilators. Intensive Care Med (2000) 26: 84±87 |
| [10] | Gray L, Philbin MK. Measuring sound in hospital nurseries. J of Perinatology, Dec 2000 (8 Pt 2), S100-4 |
| [11] | Brandon DH, Ryan DJ , Barnes AH. Effect of Environmental Changes on Noise in the NICU. Advances in Neonatal Care, Volume 8 Number 5, supplement: October 2008 Pages S5–S10 |
| [12] | Byers J, Lowman L., Waugh R Neonatal intensive care unit sound levels environment, and infant response, Neonatal Intensive Care 18 (2005), pp. 48–53 |
| [13] | Kellam B, Bhatia J. Sound spectral analysis in the neonatal intensive care unit: Measuring high frequency sound, Journal of Pediatric Nursing 23 (2008), pp. 317–323 |
| [14] | Bamiou FE, Luxon L.M. Aetiology and clinical presentations of auditory processing disorders—a review, Archives of Disease in Childhood 85 (2001), pp. 361–365 |
| [15] | Hosono S, Imura S, Akiyama K, Ttakigawa I, Shezeki S, Takeda H. Effect of vibration on auditory organ systems in low-birth weight infants treated with high-frequency oscillatory ventilation: 5 year outcome. Pediatrics International (2001) 43, 16–19 |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML