-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2025; 14(2): 15-17
doi:10.5923/j.ajdv.20251402.01
Received: Jan. 17, 2025; Accepted: Feb. 9, 2025; Published: Feb. 12, 2025

Solitary Plaque Rupioid Psoriasis with Nail Pitting: A Report of an Unusual Presentation of a Rare Variant of Psoriasis
Hala Elbedri Edris1, Mahdi Shamad2, Majed Al Dayhum1, Abrar Bin Abbas1, Salaheldin Ahmed Alfadni1
1Department of Dermatology and Venereology, Armed forces Hospitals-Southern region (AFHSR), Saudi Arabia
2College of Medicine, University of Bahri, Sudan
Correspondence to: Mahdi Shamad, College of Medicine, University of Bahri, Sudan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Psoriasis is a common chronic inflammatory skin condition presented with a variety of clinical manifestations and different variants. Herein, we report a solitary plaque rupioid psoriasis with nail pitting. This report highlights in details about this rare variant of psoriasis.
Keywords: Psoriasis, Rupioid, Nail pitting, Psoriasis variant, Papulosquamous
Cite this paper: Hala Elbedri Edris, Mahdi Shamad, Majed Al Dayhum, Abrar Bin Abbas, Salaheldin Ahmed Alfadni, Solitary Plaque Rupioid Psoriasis with Nail Pitting: A Report of an Unusual Presentation of a Rare Variant of Psoriasis, American Journal of Dermatology and Venereology, Vol. 14 No. 2, 2025, pp. 15-17. doi: 10.5923/j.ajdv.20251402.01.
1. Introduction
- Psoriasis is a common chronic inflammatory skin condition presented with a variety of clinical manifestations [1]. Based on morphologic characteristics, psoriasis can be divided into a number of variants, including chronic plaque, guttate, erythrodermic, and pustular. The plaque type represents the predominantvariant. Less common variants of psoriasis include rupioid, ostraceous, inverse, elephantine, and HIV-associated [2].Rupioid psoriasis is a rare variant that presents with cone-shaped, limpetlike lesions [3]. The origin of the word rupioid comes from the Greek word rhupos, which means dirt or filth, and is used to define well-demarcated lesions with thick, yellow, dirty-appearing, adherent crusts similar to oyster shells with a surrounding erythematous rim [4].Diagnosis of rupioid psoriasis can be established with a skin biopsy, which reveals characteristic histopathologic features of psoriasis.Rupioid psoriasis is commonly treated with a combination of topical and systemic therapy with reported good outcomes, such as methotrexate and cyclosporine [5].
2. The Case Report
- A 32-year-old male with an unremarkable medical history presented to the dermatology outpatient clinic with a 20 years duration of an asymptomatic left leg lesion. The lesion's size remained constant during this time, and there was no accompanying joint pain or swelling. The patient applied potent topical steroids many times as prescribed at private clinics with no response. There was a documented positive family history of psoriasis. Physical examination revealed a well-defined, oval, thick, hyperkeratotic, a sharply demarcated, and scaly single plaque with erythematous base over the lateral aspect of the left lower leg (Figure 1 and 2). His finger nails showed small, about the size of a pinhead, irregular depressions (pitting) (Figure 3). Other parts of the body were free. Laboratory tests, including syphilis and HIV serology, were unremarkable. A provisional diagnosis of rupioid psoriasis was made based on the clinical picture and unresponsiveness to topical corticosteroids. Histopathology of a punch skin biopsy from the lesion showed regular (psoriasiform) epidermal hyperplasia; alternating zones of and hypergranulosis, confluent parakeratosis with neutrophils collection; thinning of suprapapillary plates with dilated and tortuous vessels in dermal papillae; a perivascular, predominantly lymphocytic infiltrate in the upper and mid-dermis (Figure 4). These features are consistent with rupioid psoriasis.
 | Figure 1. The left lower leg showing a well-defined, thick, hyperkeratotic, scaly with erythematous base single plaque |
 | Figure 2. The left lower leg lesion after using of emollient |
 | Figure 3. Deep irregular pitting over finger nails |
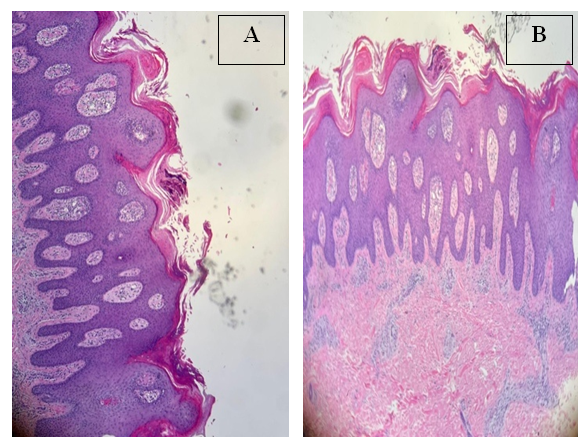 | Figure 4. A& B: Histopathology features consistent with rupioid psoriasis (details in the text) |
3. Discussion
- Psoriasis is a chronic inflammatory skin condition t can present with a range of clinical symptoms and signs. Chronic plaque psoriasis, the most common subtype of psoriasis, is characterized by well-demarcated, erythematous plaques with overlying coarse scale [1].Major subtypes of psoriasis include guttate psoriasis, pustular psoriasis, and erythrodermic psoriasis. Guttate psoriasis is typically presents as the acute onset of multiple small, inflammatory plaques. Pustular psoriasis may present as an acute, subacute, or chronic pustular eruption. Erythrodermic psoriasis exhibits cutaneous erythema and scale involving most or all of the body surface area. There are some less common subtypes of psoriasis that include rupioid, inverse, elephantine, and HIV associated [2].The terms "rupioid" and "ostraceous" refers to well-defined, round‑shaped, hyperkeratotic plaques with thick scales that resemble limpet or oyster shells, respectively [1]. Rupioid psoriasis was first documented in 1948 and is still a rare and documented form of the condition [6].Rupia is based on the Greek word rhupos, which means dirt or filth. Clinically, rupioid manifestations have also been seen in a number of illnesses, such as disseminated histoplasmosis [7], reactive arthritis [8], secondary syphilis [9], keratotic scabies [10], and including rupioid psoriasis. Rupioid or malignant syphilis refers to the stage in which papulopustules of pustular syphilis undergo central necrosis due to endarteritis obliterans and intravascular thrombosis [4]. Rupioid manifestations in Reactive arthritis may have a similar appearance to rupioid psoriasis but may be distinguished by a geographic relief map configuration with coalescing, keratotic and desquamating lesions, as well as associated urethritis, arthritis, and conjunctivitis [8].Patients with thick plaque (rupioid psoriasis) are more likely to be male with a higher incidence of nail disease as evident in our patient (a male patient with typical lesionand nail pitting), and psoriatic arthritis as well as a greater body surface area affected than patients with thin plaquepsoriasis, which are not evident in our patient [11,12].Drug history is important in patients with rupioid forms of psoriasis as its flares have been associated with the intake of some medication such corticosteroids, non-steroidal anti-inflammatory drugs, lithium carbonate, β-blockers,and hydroxychloroquine [13].A skin biopsy is diagnostic for rupioid psoriasis which displays typical histopathological features of psoriasis as demonstrated in the present case.Laboratory analysis should be performed to rule out other causes of rupioid lesions.Our patient’s lab showed negative serology for syphilis and HIV. Based on the clinical feature, histopathology, and laboratory results and diagnosis of rupioid psoriasis was confirmed.Hyperkeratotic lesions of psoriasis are generally resistant to topical therapy because of poor penetration of applied agents, which explained the unresponsiveness to topical corticosteroids in our case [14].
4. Conclusions
- This case demonstrates the importance of integrating clinical, histopathological, and familial data to diagnose rare and atypical presentations of psoriasis, such as rupioid psoriasis. It also highlights the need for awareness of this variant among clinicians to ensure timely and accurate diagnosis.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML