-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2025; 14(1): 10-13
doi:10.5923/j.ajdv.20251401.03
Received: Jan. 16, 2025; Accepted: Feb. 7, 2025; Published: Feb. 10, 2025

Characteristics of Mixed Vitiligo
Mahdi M. A. Shamad1, Mohammed T. M. Siddig2, Yousif Tibin M. Nour1
1College of Medicine, University of Bahri, Sudan
2Khartoum Dermatology and Venereology Teaching Hospital, Khartoum, Sudan
Correspondence to: Mahdi M. A. Shamad, College of Medicine, University of Bahri, Sudan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

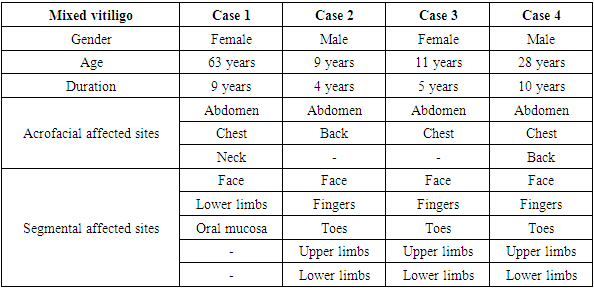
Mixed vitiligo (MV) is a rare and clinically subtype of vitiligo characterized by the the concomitant appearance of segmental and non-segmental vitiligo. While non-segmental vitiligo (NSV) usually manifests as bilateral, symmetrical patches and segmental vitiligo (SV) as unilateral, localized depigmentation, mixed vitiligo contains characteristics of both, creating difficulties for diagnosis and treatment. Mixed vitiligo is relatively uncommon, and according to studies, its occurrence among vitiligo patients is quite low. It frequently presents first as segmental vitiligo, which is followed by the emergence of non-segmental lesions. Risk factor for occurrence of mixed vitiligo is the presence of leukotrichia and halo nevi present at the onset of SV. This paper aims to study the characteristics of mixed vitiligo and identify its characteristics. This descriptive, cross-sectional study was carried out between September 2022 and March 2023. All vitiligo patients who consented to participate in the study were included. The study population consisted of 45 patients with various forms of vitiligo who came to the study area during the study period. Clinical examination was performed on each individual, and the results were documented using a specifically created questionnaire. A total of 45 vitiligo patients were included in this study. Mixed vitiligo was identified in 4 patients that formed 8.9% of the study population. Other subtypes include non-segmental vitiligo in 32 patients (71.1%) and segmental vitiligo in 9 patients forming 20% of the study sample. Mixed vitiligo patients were 2 males and 2 females. The four cases of mixed vitiligo demonstrated a consistent pattern of segmental vitiligo affecting the trunk (chest, abdomen, and back) and acrofacial vitiligo involving the face, fingers, toes, and limbs. The non-segmental component of mixed vitiligo is supported by the fact that all of the patients had bilateral lesions. In conclusion, the study's findings about the bilateral distribution, mucosal involvement, and possible systemic symptoms underscore the complexity of mixed vitiligo and its impact on patients. These results advance our knowledge of mixed vitiligo and highlight the need for more study to enhance patient outcomes, diagnosis, and treatment.
Keywords: Mixed vitiligo, Segmental vitiligo, Non-segmental vitiligo, Vitiligo
Cite this paper: Mahdi M. A. Shamad, Mohammed T. M. Siddig, Yousif Tibin M. Nour, Characteristics of Mixed Vitiligo, American Journal of Dermatology and Venereology, Vol. 14 No. 1, 2025, pp. 10-13. doi: 10.5923/j.ajdv.20251401.03.
1. Introduction
- Mixed vitiligo (MV) is a rare and clinically subtype of vitiligo characterized by the simultaneous presence of segmental and non-segmental vitiligo. It represents a unique and understudied subtype of vitiligo, with distinct clinical and pathogenic features. While non-segmental vitiligo (NSV) usually manifests as bilateral, symmetrical patches and segmental vitiligo (SV) as unilateral, localized depigmentation, mixed vitiligo contains characteristics of both, creating difficulties for diagnosis and treatment. Mixed vitiligo is relatively uncommon, and according to studies, its occurrence among vitiligo patients is quite low [1]. It frequently presents first as segmental vitiligo, which is followed by the emergence of non-segmental lesions. Risk factor for occurrence of mixed vitiligo is the presence of leukotrichia and halo nevi present at the onset of SV [2]. Younger people are frequently affected by the illness, with a significant proportion of cases reported in pediatric populations [1].Although the pathogenesis of mixed vitiligo is poorly understood a combination of immunological, neurological, and genetic factors are believed to be involved. Non-segmental vitiligo is linked to oxidative stress and autoimmune dysregulation, whereas segmental vitiligo is frequently linked to somatic mosaicism and neurological processes [3]. Although additional researches are required to clarify these mechanisms, the coexistence of both forms in mixed vitiligo raises the possibility of an overlap in pathogenic pathways. Clinical examination is the primary method used to diagnose mixed vitiligo; histopathology and dermoscopy are used as supplementary methods. Mixed vitiligo was identified as a separate subtype by the 2011 Vitiligo Global Issues Consensus Conference, which emphasized the significance of identifying its distinctive clinical characteristics [4]. A customized strategy that addresses the disease's widespread and localized aspects is needed to treat mixed vitiligo. Systemic treatments include oral corticosteroids and Janus kinase (JAK) inhibitors may be necessary for non-segmental involvement, but topical corticosteroids, calcineurin inhibitors, and phototherapy are frequently utilized for segmental lesions [5]. The possibility of combination therapies, such as phototherapy and surgical procedures, in attaining depigmentation in mixed vitiligo was highlighted in a review by Rodrigues et al. [6]. This paper aims to identify the characteristics and the clinical spectrum of mixed vitiligo.
2. Methodology
- This descriptive, cross-sectional study was carried out between September 2022 and March 2023 at the Phototherapy Centre of the Khartoum Dermatology and Venereology Teaching Hospital in Sudan. All vitiligo patients who consented to participate in the study were included. The study population consisted of 45 patients with various forms of vitiligo who came to the study area during the study period. Following ethical clearance from the appropriate authorities, participants signed informed consent was obtained, and privacy of data collection was taken into consideration. Clinical examination was performed on each individual, and the results were documented using a specifically created questionnaire. Data were taken from patients who visited the phototherapy center, including demographic and clinical information.The collected data were analyzed by Statistical Packages for Social Sciences (SPSS) 23.0 software with Chi-square test, as appropriate P<0.05 was considering statistically significant (Confidence Interval: CI 95%).
3. Results
- A total of 45 vitiligo patients were included in this study (Figure 1). Mixed vitiligo, characterized by the concomitant appearance of segmental and non-segmental vitiligo was identified in 4 patients that formed 8.9% of the study population. Other subtypes include non-segmental vitiligo in 32 patients (71.1%) and segmental vitiligo in 9 patients forming 20% of the study sample. Mixed vitiligo patients were 2 males and 2 females. Details of the cases are in table 1.
|
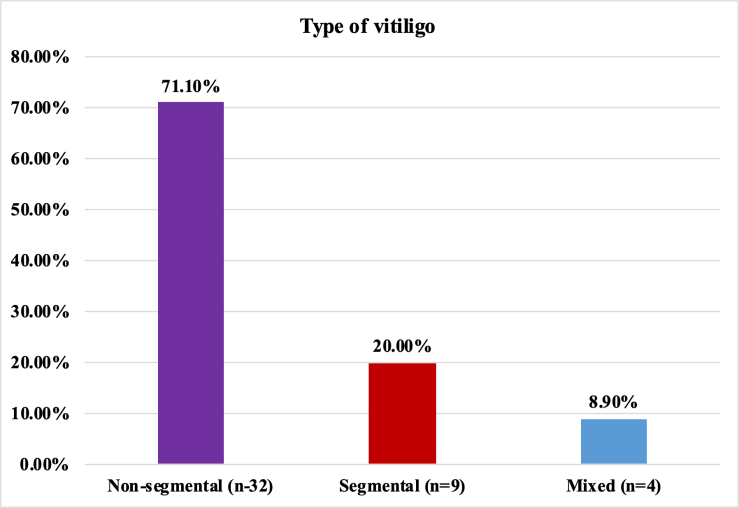 | Figure 1. Types of vitiligo in the study population |
4. Discussion
- The results of the research provide substantial illumination on the clinical manifestation of mixed vitiligo, a less frequent but nonetheless important subtype of the vitiligo. Despite being less common than non-segmental vitiligo, mixed vitiligo presents particular therapeutic difficulties since it combines segmental and non-segmental characteristics. Compared to non-segmental vitiligo (71.1%) and segmental vitiligo (20%), mixed vitiligo, which is defined as the dual presentation of segmental and non-segmental vitiligo, was seen in 8.9% of the current study group. This result is consistent with earlier research that describes mixed vitiligo as an uncommon subtype of vitiligo [1,4]. Mixed vitiligo combines the extensive distribution of non-segmental vitiligo with the localised, unilateral pattern of segmental vitiligo, in contrast to non-segmental vitiligo, which usually manifests as symmetrical, bilateral lesions. This dual presentation of mixed vitiligo makes diagnosis and management difficult, as treatment strategies need to address both the disease's systemic and localized components.Mixed vitiligo raises questions about the conventional division of vitiligo into discrete subtypes and raises the possibility of a continuum between segmental and non-segmental forms. In mixed vitiligo, the coexistence of both forms may indicate common or overlapping pathogenic mechanisms, including hereditary susceptibility, neurological abnormalities, or autoimmune dysregulation [5]. The underlying pathophysiology of mixed vitiligo and its connection to other kinds require further investigation [6].Clinically, an accurate evaluation of the distribution and course of lesions is necessary to diagnose mixed vitiligo. Because mixed vitiligo has a bilateral and widespread nature, this non-segmental component may require systemic therapies like immunosuppressants or phototherapy, while the segmental component may benefit from localized treatments [7]. Systemic symptoms including joint pain and mucosal involvement emphasize the necessity of a thorough approach to patient management, which may require interdisciplinary cooperation when needed.The systemic symptoms observed in mixed vitiligo patients, such as mucosal involvement and joint pain, align with the growing recognition of vitiligo as a condition with potential systemic manifestations.Mucosal involvement in vitiligo is often associated with more extensive or active disease. It may also indicate a broader autoimmune process, as mucosal surfaces are rich in immune cells and are common sites for autoimmune activity. Studies have shown that mucosal vitiligo is more frequently observed in patients with non-segmental vitiligo, which is considered a systemic autoimmune condition with poor prognostic implication [8]. The presence of mucosal involvement in mixed vitiligo could suggest a similar autoimmune mechanism, linking it to systemic immune dysregulation. One patient with mixed vitiligo reported joint pain and swelling, which are not typical features of vitiligo but may indicate an associated systemic condition. Vitiligo has been associated with other autoimmune diseases, including thyroid disorders, alopecia areata, and rheumatoid arthritis. The presence of joint symptoms in a patient with mixed vitiligo may reflect an underlying systemic autoimmune process. For example, a study by Gill et al. found that patients with vitiligo have a higher prevalence of autoimmune comorbidities, including joint-related conditions [9].
5. Conclusions
- In conclusion, mixed vitiligo is a rare but clinically significant subtype of vitiligo that is characterized by the coexistence of both segmental and non-segmental features. The study's findings about the bilateral distribution, mucosal involvement, and possible systemic symptoms underscore the complexity of mixed vitiligo and its impact on patients. These results advance our knowledge of mixed vitiligo and highlight the need for more study to enhance patient outcomes, diagnosis, and treatment.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML