Zahraa Hayder Al-Hamamy
Dermatology Department, AL-Kindy College of Medicine, University of Baghdad, Baghdad, Iraq
Correspondence to: Zahraa Hayder Al-Hamamy , Dermatology Department, AL-Kindy College of Medicine, University of Baghdad, Baghdad, Iraq.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Background: Biopsy is an important diagnostic tool in dermatology. It reflects the number and types of patient’s diseases attending a dermatological clinic and the care level. Clinicopathological correlation is an important step in establishing the final diagnosis. Patients and methods: The study is a retrospective record based observational study. It was carried out at the dermatology center / al- Kindy Teaching Hospital. Patients were divided into 2 groups: Group 1: Patients consulting the center from the first of August 2019 to the first of February 2020 (before COVID-19) Group 2: Patients consulting the center from the first of August 2021 to the first of February 2022 (after COVID-19). The data were collected from the records of the outpatient department and from the histopathological laboratory reports, the histopathological diagnosis was compared with first, second and third differential diagnoses. Results: A total of 204 patients were included in the study, 81 males (39.7%) and 123 females (60.2%). The mean age was 40.99 years and SD +/-19.44; in group one the total number was 124 patients; 46 (37.1%) males and 78 (62.9%) females. In group 2 the total number was 80 patients; 35(43.75%) males and 45(56.25%) females. The trunk was most common site of biopsy in the two groups. Neoplasms were most frequent diagnosis in the two groups, in group one they were followed by interface dermatitis and infective diseases while in group 2 neoplasms were followed by infective diseases and vascular proliferations. Concordance between clinical and histological diagnoses in this study were roughly the same in pre COVID-19 (69.25%) and in the post COVID-19 (70%). Conclusion: The number of cases was higher in pre COVID-19 period. In the pre COVID-19 period benign tumors were more common, while in post COVID-19 malignant neoplasm (BCC) were more common. The consistency between clinical and histological diagnoses before and after COVID-19 was found to be roughly the same.
Keywords:
COVID-19, Skin biopsy
Cite this paper: Zahraa Hayder Al-Hamamy , Clinicopathological Correlation in Pre and Post COVID-19 Period in the Diagnosis of Skin Diseases, a Retrospective Comparative Study, American Journal of Dermatology and Venereology, Vol. 11 No. 1, 2022, pp. 16-20. doi: 10.5923/j.ajdv.20221101.03.
1. Introduction
Biopsy is an important diagnostic tool in dermatology. [1] Incisional biopsy is indicated in suspicious cases to establish the diagnosis. [2]. Also, all excised material must be subjected to histological examination [3,4,5]. Biopsy reflects the number and types of diseases of patients attending a dermatological clinic. [3,5] It also reflects the level of care in that given clinic. [5] Clinicopathological correlation is an important step in establishing the final diagnosis. [6] Usually, clinicians propose a number of differential diagnoses to the pathologist to help in interpreting the specimen. [6,7]
2. Patients and Methods
The study is a retrospective record based observational study. It was carried out at the dermatology center /Al- Kindy Teaching Hospital, and included patients consulting during specified periods before and after the COVID-19 19 pandemic. Patients were divided into 2 groups:Group 1: Patients consulting the center from the first of August 2019 to the first of February 2020 (before COVID-19).Group 2: Patients consulting the center from the first of August 2021 to the first of February 2022 (after COVID-19). Ethical approval was granted by the scientific committee of Al-Kindy College of Medicine.All Patients attended the clinic during the specified periods who underwent a skin biopsy were included in the study. The data were collected from the records of the outpatient department and from the histopathological laboratory reports. The following information were recorded; patients age, gender and site of biopsy. The first three provisional diagnoses written by the dermatologist were recorded and histopathological diagnoses were also recorded.A comparison regarding the number, age and gender of patients in group 1 and 2 were carried out. The histopathological diagnosis was compared with first, second and third differential diagnoses.Values were expressed as percentages, mean and standard deviation.
3. Results
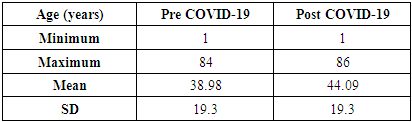
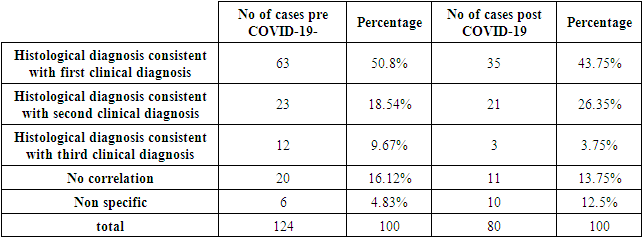
A total of 204 patients were included in the study, 81 males (39.7%) and 123 females (60.2%). The mean age was 40.99 years and SD +/-19.44.Patients were divided into two groupsGroup 1: Patients before COVID-19 pandemic. The total number was 124 patients; 46 (37.1%) males and 78 (62.9%) females. The mean age was 38.98 years and SD +/-19.3. (Table 1)Table 1. Mean and standard deviation of age in years of patients in pre and post COVID-19 period
 |
| |
|
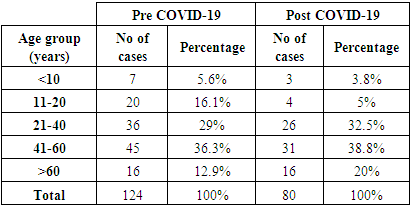
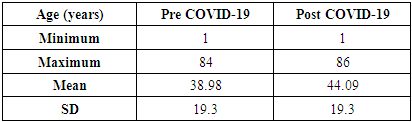
Group 2: patients after COVID-19 19 pandemic. The total number was 80; 35(43.75%) males and 45(56.25%) females. The mean age was 44.09 years and SD +/- 19.3 (Table 1). The most frequent age group in the two periods was between 41and 60 years. (Table 2)Table 2. Different age groups in years distribution in pre and post COVID-19 period groups Site of biopsy
 |
| |
|
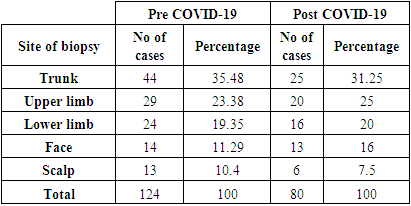
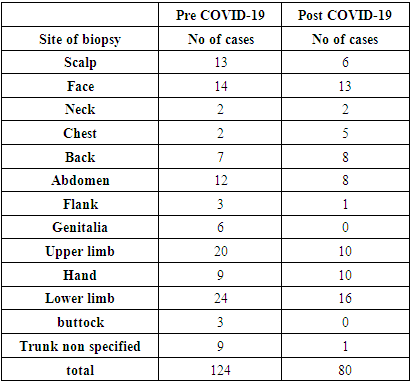
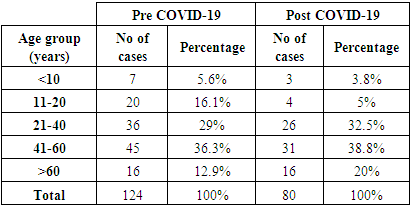
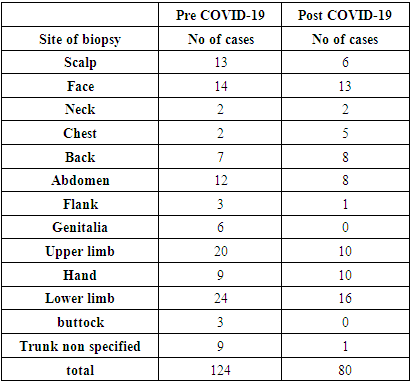
The site of biopsy is shown in (Tables 3,4). The trunk was most common site of biopsy. (Table 3)Table 3. Site of biopsy distribution in the two groups
 |
| |
|
Table 4. Site of biopsy distribution in details in the two period groups
 |
| |
|
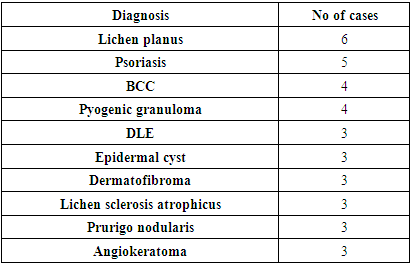
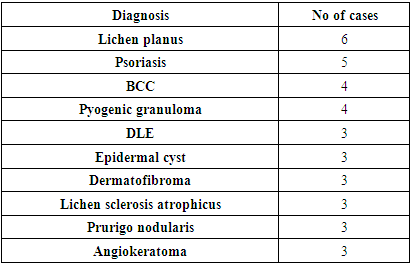
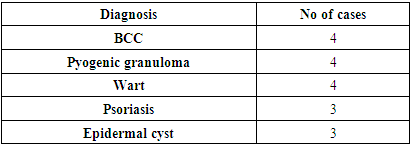
The most frequent specific histological diagnosis in pre COVID-19 period was lichen planus followed by psoriasis then basal cell carcinoma (Table 5), although neoplasms as a category were more frequent. After COVID-19 the most frequent diagnosis was basal cell carcinoma, pyogenic granuloma and wart followed by psoriasis. (Table 6)Table 5. The most frequent histopathological diagnoses in group 1 (pre COVID-19)
 |
| |
|
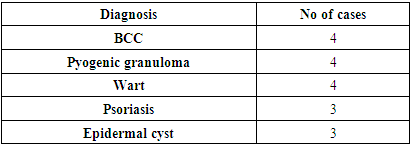
Table 6. The most frequent histopathological diagnoses in group 2 (post COVID-19)
 |
| |
|
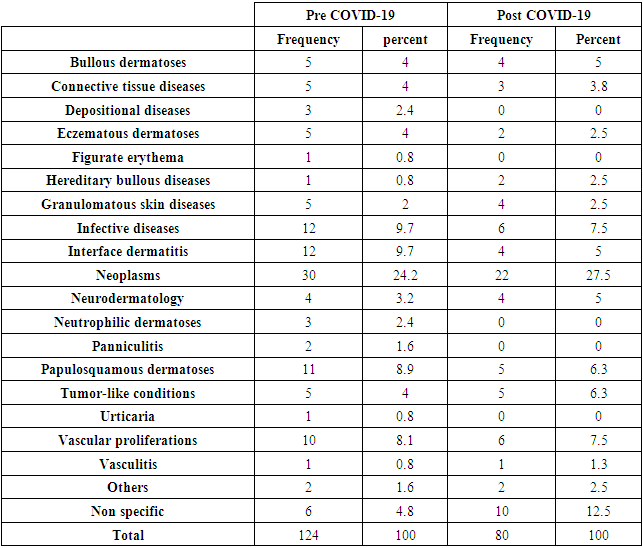
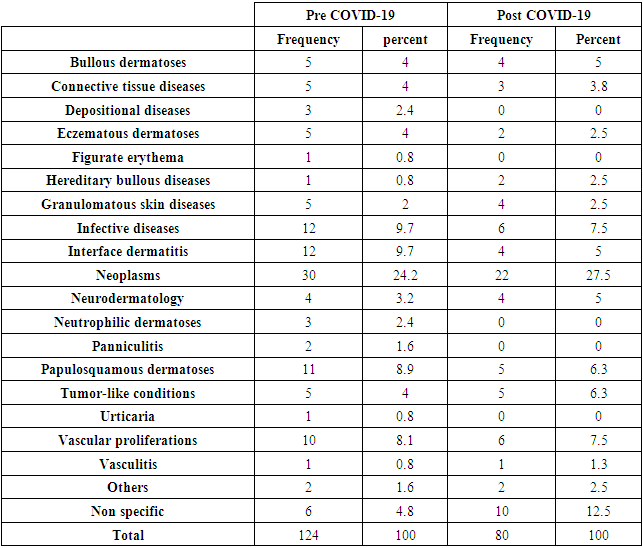
The pathological diagnosis was classified according to etiology and is shown in (Table 7). Neoplasms were most frequent diagnosis in both groups, in group1 they were followed by interface dermatitis and infective diseases while in group 2 neoplasms were followed by infective diseases and vascular proliferations. (Table 7)Table 7. Prevalence of different skin diseases in the two groups (according to etiological classification)
 |
| |
|
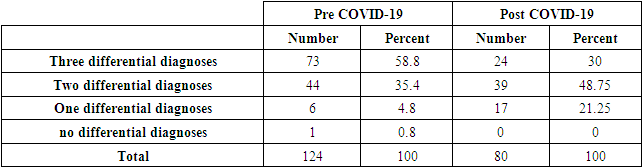
Regarding Number of neoplasms in pre COVID-19 period; there were 30 cases (24.2% from total). In post COVID-19 period there were 22 neoplasms (27.5% from total). Benign neoplasms in pre COVID-19 period were more frequent than malignant (17 cases, 56.6%). This included 4 nevi, 3 dermatofibromas, 2 seborrheic keratoses, and one leiomyoma, Lipoma, cutaneous horn, Hidradenoma, Syringoma, Pilomatrixoma, clear cell Acanthoma and digital fibroma. While there were 13 malignant neoplasms (43.33% of neoplasms) which included 4 cases of basal cell carcinoma, 2 mycosis fungoides, 2 Kaposi sarcomas, 2 skin metastases and one case for each of keratoacanthoma, squamous cell carcinoma and actinic keratosis. In the post COVID-19 period benign neoplasms were 8 cases (36.36%) which was included 2 nevi, one case for each of dermatofibroma, seborrheic keratosis, fibrokeratoma, leiomyoma, blue nevus, omphalomesenteric duct polyp.There were malignant 14 neoplasms (63.63% of neoplasms) which included 4 cases of basal cell carcinoma, 2 cases for each of keratoacanthoma, mycosis fungoides, secondary metastasis and one case of each of Bowen’s disease, actinic keratosis, verrucous carcinoma and Carcinoma Erysipeloides.The number of differential diagnoses illustrated by dermatologist were shown in (Table 8).Table 8. Number of differential diagnoses illustrated by dermatologist
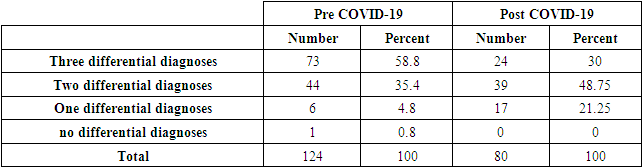 |
| |
|
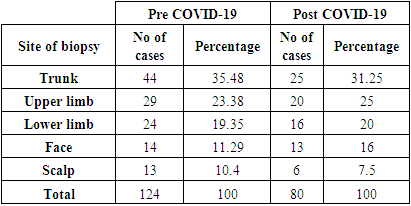
On comparing clinical diagnosis with histological diagnosis in group 1, the histological diagnoses conformed with the first, second and third clinical diagnoses in (50.8%), (18.45%) and (9.67%) respectively. While there was no correlation between clinical and histological diagnoses in (16.12%) of cases and 4.83% of cases the histopathological diagnosis was non-specific. (Table 9)Table 9. Correlation between clinical and histological diagnoses in the two groups
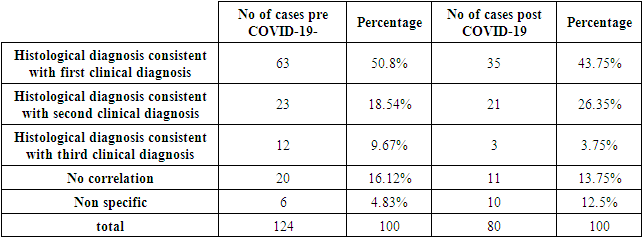 |
| |
|
In group 2 the histological diagnoses conformed with the first, second and third clinical diagnoses in (43.75%), (26.25%) and (3.75%) respectively. While there was no correlation between clinical and histological diagnoses in (13.75%) of cases and in 12.5% of cases the histopathological diagnosis was non-specific. (Table 9)
4. Discussion
COVID-19 pandemic started in early 2020 and swept the globe. It had a profound effect on the health and life of people in all countries. [8]In Iraq there was a period of complete lockdown of two months. Many hospitals were restricted to COVID-19 patients. After the period of lockdown life started to be back again and the number of patients consulting the dermatology clinic starts to rise. [9]In the present study a comparison was made for patients attending al-Kindy dermatological center before and after COVID-19 regarding the number, gender and age. Also, a comparison regarding the diseases were performed to know whether COVID-19 had effects on diseases subjected to biopsy. The number of cases was higher in pre COVID-19 period; this is expected because a smaller number of patients are consulting the clinic in post COVID-19 era.In both groups female numbers were higher. The most common age group was 41-60 years in both groups and the most common site of biopsy was the trunk, this is may be due to the preference of dermatologists to take a biopsy from cosmetically less important areas.Neoplasms constituted 24% of cases in pre COVID-19 period and 27% in post COVID-19 period. However, in the pre COVID-19 period benign tumors were more common while in post COVID-19 malignant neoplasm (BCC)were more common, this can be explained by the fact that people in post COVID-19 period consult for only important reasons.In the pre COVID-19 period rashes such as lichen planus and psoriasis were biopsied, while in post COVID-19 period most such rashes were not biopsied. Non-specific diagnosis counts less in pre COVID-19 period 4.8%, while in the post COVID-19 period it was 12.5%.The consistency between clinical and histological diagnoses before and after COVID-19 was roughly the same. In pre COVID-19 (50.8%) were consistent with first and (18.45%) with second, together they constitute 69.25%.In post COVID-19 (43.75%) was consistent with first and (26.25%) with the second clinical diagnosis, together they are 70%.While No correlation was found between clinical and histological diagnoses in 16% in pre COVID-19 period and 13.7% in post COVID-19 period. On comparing the results of the present study with previous similar studies [10,11,12], the mean age at the present study was 40.9 years which is higher than the study by Al-Saif et al (2019) (36.9 years) [11] and similar to Al-Hamammy et al (2019) study (41.6 years). [10]In the present study females were more commonly had biopsies (60.29%). This is similar to the study by Al-Saif et al (58.1%) [11] and different from the study by Al-Hamammy where males (60%) outnumbered females (40%). [10]Regarding the site of biopsy, the trunk was the most common site of biopsy 35.48% in group 1 and 31.25% in group 2 while in the study by Al-Saif the lower limbs were the most frequent site (29.1%). [11]In the study by Akanksha et al the upper limbs were the most frequent sites [12] and in Al-Hamammy study there were equal percentages for head &neck, trunk& genitalia biopsies. [10]The most common diagnoses in the present study were neoplasms which constituted 24% of cases in pre COVID-19 period and 27% in post COVID-19 period similar to Al-Hamammy et al (2019) study in which neoplasms constituted 46.36% [10] while Al-Saif study the most frequent diagnoses were papulosquamous and eczematous dermatoses (26.2%). [11]Regarding the concordance between clinical and histological diagnoses in this study they were roughly the same in pre COVID-19 (69.25%) and in the post COVID-19 (70%). While the study by Al-Saif et al (2019) the overall concordance was 75.9% (partial concordance 47.6%, full concordance 28.3%) [11], Akanksha et al (2020) showed the overall concordance 61.01%. The percentage of cases found to have definitive pathological-clinical concordance was 45.67% and 15.34% had a descriptive pathological diagnosis consistent with the clinical diagnosis. [12]In Al-Hamammy et al (2019) study showed that there was a consistency between provisional clinical diagnoses and histopathological report in 19 biopsies (17%), 75 biopsies (68%) were consistent with other differential diagnoses and 16 biopsies (15%) were inconsistent. [10]
References
| [1] | Balasubramanian P, Chandrashekar L, Thappa DM, Jaisankar TJ, Malathi M, Ganesh RN, Singh N. A retrospective audit of skin biopsies done in a tertiary care center in India. Int J Dermatol. 2015, 54: 939-943. 10.1111/ijd.12718. |
| [2] | Farmer ER: Why a skin biopsy? Arch Dermatol. 2000, 136:779-780. 10.1001/archderm.136.6.779. |
| [3] | Llamas-Velasco M, Paredes BE. Basic concepts in skin biopsy. Part I. Actas Dermosifiliogr 2012; 103: 12-2. |
| [4] | Korfitis C, Gregoriou S, Antoniou C, Katsambas AD, Rigopoulos D. Skin biopsy in the context of dermatological diagnosis: a retrospective cohort study. Dermatol Res Pract 2014; 2014: 734906. |
| [5] | Werner B: Skin biopsy and its histopathologic analysis: Why? What for? How? Part I. An Bras Dermatol. 2009, 84: 391-395. 10.1590/s0365-0596200900040001. |
| [6] | Sa DK, Kumar P. Clinicopathological consistency in diagnosis of skin disorders: a retrospective study of 371 histopathology reports. ??JPAD 2016; 26: 96-8. |
| [7] | Rajaratnam R, Smith AG, Biswas A, Stephens M. The value of skin biopsy in inflammatory dermatoses. Am J Dermatopathol 2009; 31: 350-3. |
| [8] | Bhargava S, McKeever C, Kroumpouzos G. Impact of COVID-19 pandemic on dermatology practices: Results of a web-based, global survey. Internat J Women’s Dermatol 2021; 7: 217–223. |
| [9] | Al-Hamamy HR, Jawad ZK. A Case Report of Papulo-pustular Rosacea-Like Reaction after the Second Dose of Pfizer Vaccine. Iraqi Postgrad Med J 2022; 21, 127-130. |
| [10] | Al-Hamammy HR, Al-Alsadawi A, Al-Samarraee RI. Clinicopathological Consistency in the Diagnosis of Skin Disorders in Patients Attending Dermatology Centre\ Medical City Teaching Hospital. Iraqi Postgrad Med J 2019; 18: 218-226. |
| [11] | Al-Saif FM, Binsufayan SA, Alhussain AH, Alkaff TM, Alshaikh HM, Aldosari MS, Binsufayan SA, AlTaleb RM, Alotaibi HM, Alshahwanab MA. Clinicopathological concordance in the diagnosis of skin diseases: a retrospective analysis of 5000 histopathology reports. Ann Saudi.Med 2019; 39(6): 388-394. DOI:10.5144/0256-4947.2019.388. |
| [12] | Akanksha M, Fouzia S, Sharma S, Pooja G, Geeti K, RameshV. Clinicopathological Concordance in 2216 Cases of Skin Biopsy over One Year: An Indian Experience. Cureus 2020; 12: e7752. DOI 10.7759/cureus.7752. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML