Sarah M. H. Hussein1, Hayder R. Al-Hamamy2
1Dermatology Center, Medical City Teaching Hospital
2Chairman of Scientific Council of Dermatology and Venereology Iraqi Board for Medical Specialization
Correspondence to: Hayder R. Al-Hamamy, Chairman of Scientific Council of Dermatology and Venereology Iraqi Board for Medical Specialization.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Background: Cutaneous lymphoma can be primary, starting in the skin and may have an extracutaneous manifestations during their courses, or secondary extending from other organs, most commonly a spread from extracutaneous non-Hodgkin’s lymphoma. The primary cutaneous lymphoma can be either T cell or B cell lymphoma. Differences in the incidence and clinical features of different types of lymphoma in different geographic locations are noted. Objectives: To describe the clinical and histopathological features of different types of lymphoma involving the skin. Patients and Methods: The study is a retrospective, descriptive, study. A file review of patients diagnosed with cutaneous lymphoma was performed and the diagnosis was based on the clinical, histopathological grounds supported by immunohistochemical studies when needed. All patients who consulted the Center of Dermatology and Venereology at Baghdad Medical City over 9 year period from June 2012 to May 2021 were included. Results: The total number of patients with cutaneous lymphoma was 120 which included 90% primary cutaneous T-cell lymphoma, 4.2% primary cutaneous B-cell lymphoma, and 5.8% secondary lymphoma. The male to female ratio was 1.2:1. Age at diagnosis of primary cutaneous T-cell lymphoma was 44.3±16.4 years and the duration was 8.7±10.9 years while primary cutaneous B-cell lymphoma was 67.4±12 years and the duration was 11.6±20 months, and secondary lymphoma was 58.4±18.6 years and the duration was 4.7±4.5 months. The clinical distribution of primary cutaneous T-cell lymphoma was mainly on the trunk and proximal lower extremities (91.6%), while primary cutaneous B-cell lymphoma was mainly on the head (60%) and secondary lymphoma was on the trunk (85.7%). In patients with mycosis fungoides, the most common morphological pattern was the early patches and plaques with most patients in stage 1A or 1B. The atypical lymphocytes showed CD3 and CD4 expression in nearly all specimens examined by immunohistochemistry. Conclusions: Mycosis fungoides was the most common diagnosis, followed by secondary non-Hodgkin lymphoma and primary cutaneous B-cell lymphoma, the mean age at diagnosis was 44 years in primary cutaneous T-cell lymphoma, 67 years in primary cutaneous B-cell lymphoma, and 58 years in secondary cutaneous lymphoma. The majority of mucosis fungoides patients were in the early stages.
Keywords:
Primary cutaneous T-cell lymphoma, Primary cutaneous B-cell lymphoma, Mycosis fungoides, Epidemiology
Cite this paper: Sarah M. H. Hussein, Hayder R. Al-Hamamy, Cutaneous Lymphoma, Clinical and Histopathological Study, American Journal of Dermatology and Venereology, Vol. 11 No. 1, 2022, pp. 1-6. doi: 10.5923/j.ajdv.20221101.01.
1. Introduction
Primary cutaneous lymphomas represent a heterogeneous group of lymphatic neoplasia starting in the skin and may have an extracutaneous manifestations during their courses. They can be either Primary cutaneous T cell lymphoma (PCTCL) or Primary cutaneous B cell lymphoma (PCBCL). While secondary cutaneous lymphoma is most commonly a spread from extracutaneous non-Hodgkin’s lymphoma. Primary cutaneous lymphoma exhibits distinct clinical, histological, immunophenotypic, and genetic features. Moreover it differs in prognosis and treatment from systemic lymphomas with similar histological features [1]. There is paucity in literature regarding secondary lymphoma of the skin [2]. Differences in the incidence and clinical features of different types of lymphoma in different geographic locations are noted [1].
2. Aim of the Study
To describe the clinical and histopathological features of different types of lymphoma involving the skin.
3. Patients and Methods
The study is a retrospective descriptive study. A file review of patients diagnosed with cutaneous lymphoma was performed including all patients seen in the Center of Dermatology, Medical City Teaching Hospital over a 9 year period from the beginning of June 2012 to the end of May 2021. The ethical approval was given by the Scientific Council of Dermatology and Venereology-Iraqi Board for Medical Specializations. Detailed history including age, gender, onset, duration, and evolution of the disease and the associated symptoms, past medical history, drug, and social history were reviewed. Clinical morphology and distribution of the skin lesions, general examination including lymph nodes examination were noted. The results of the histopathological examination were recorded and some slides were reviewed, as well as the results of immunohistochemistry in some cases.In patients with MF, TNM staging was noted, all patients underwent a complete physical examination, complete blood cell count with examination for Sezary cells, chest X-ray, and CT scan of the chest and abdomen. The diagnosis was based on clinical and histopathological studies supported by immunohistochemical examination when needed. The collected data were organized, tabulated, and statistically analyzed and values were expressed as a number, percentage, mean with or without SD.
4. Results
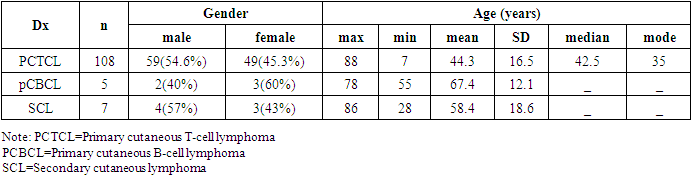
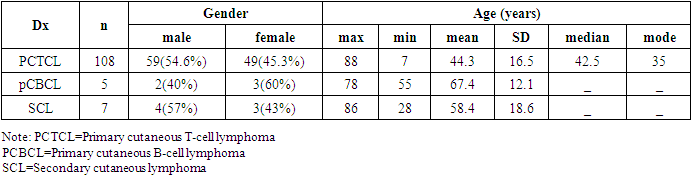
A total of 120 cases of CL were studied including 108 (90%) with PCTCL, 5 (4.2%) with PCBCL and 7 (5.8%) secondary cutaneous lymphoma. Of PCTCL; 106 had MF (98% of PCTCL), one patient had primary cutaneous anaplastic large cell lymphoma (PCALCL) and one patient had extranodal NK-T-cell lymphoma. The age and the gender characteristics are presented in table 1. In general the male to female ratio was 1.2:1.Table (1). Age (years) and gender characteristics and of cutaneous lymphoma
 |
| |
|
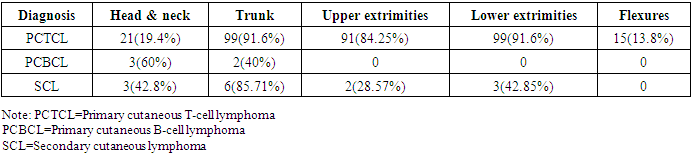
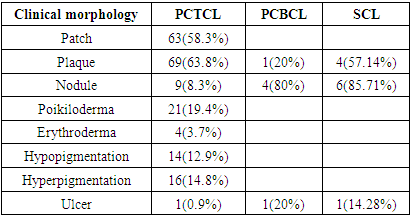
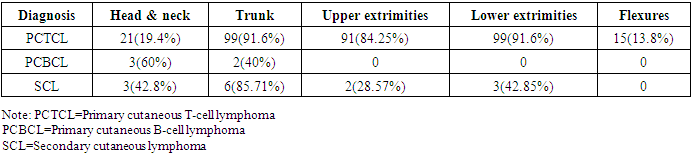
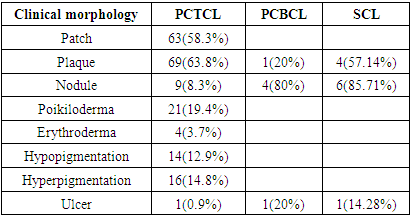
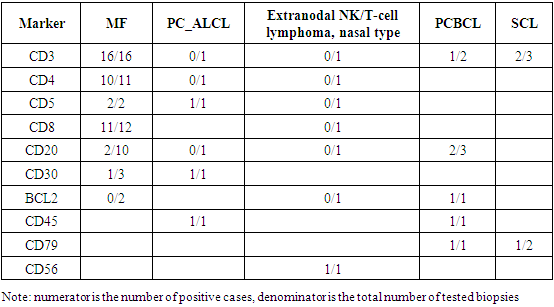
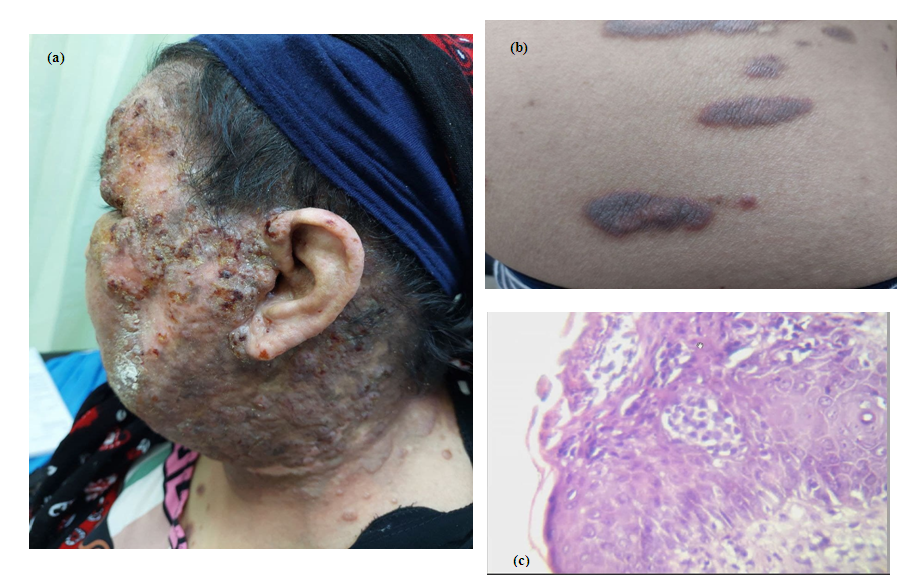
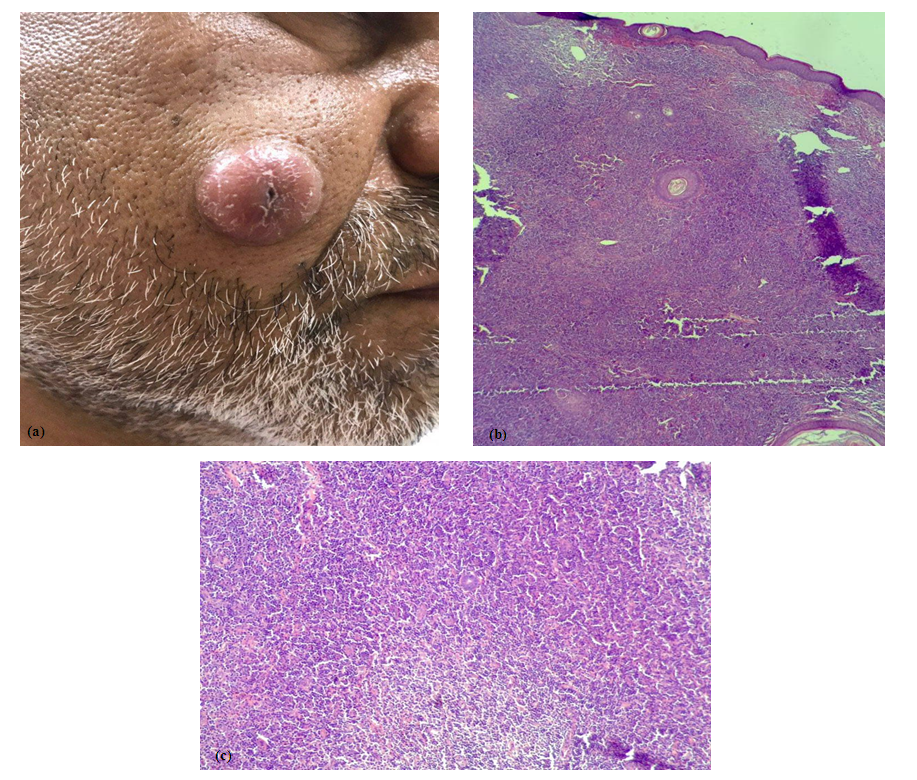
The age at diagnosis of PCTCL was 44.3±16.4 years and the duration was 8.7±10.9 years while PCBCL was 67.4±12 years and the duration was 11.6±20 months, and secondary lymphoma was 58.4±18.6 years and the duration was 4.7±4.5 months. The clinical distribution of PCTCL was mainly on the trunk and proximal lower extremities (91.6%), while PCBCL was mainly on the head (60%) and secondary lymphoma was on the trunk (85.7%) (table 2). Itching was more frequent in PCTCL (57.4%), less common in SCL (28.5%) and almost non of the patients with PCBCL had itching. The most common clinical morphology in PCTCL was patch and plaque while in PCBCL and SCL it was mainly nodules, plaques and ulcerations (table 3) (figure 1-3).Table (2). Clinical distribution of cutaneous lymphoma
 |
| |
|
Table (3). Clinical morphology of cutaneous lymphoma
 |
| |
|
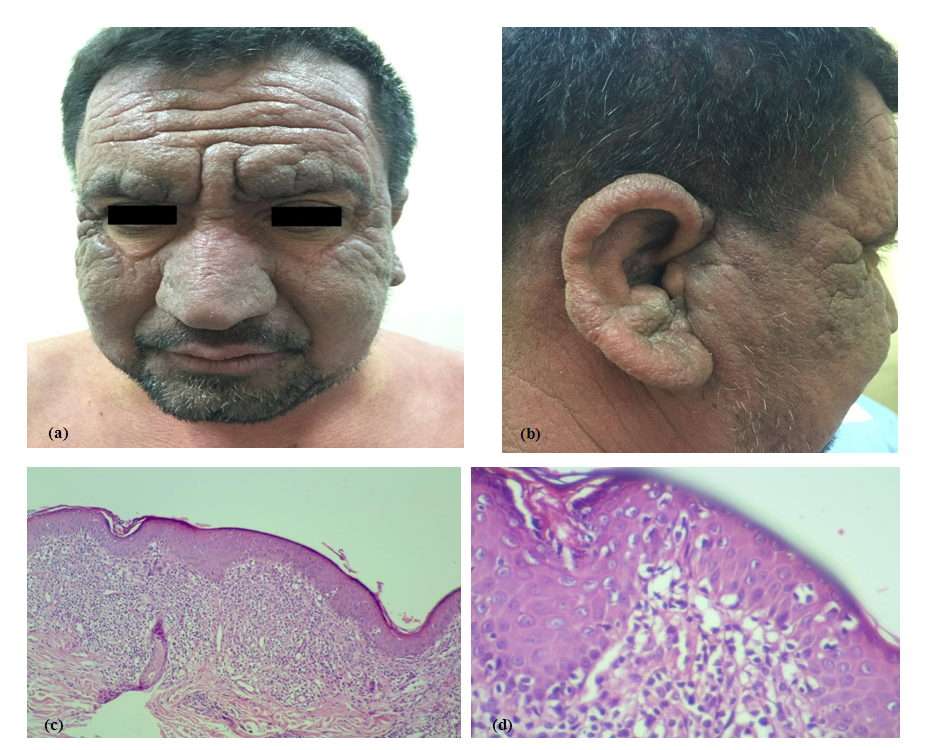
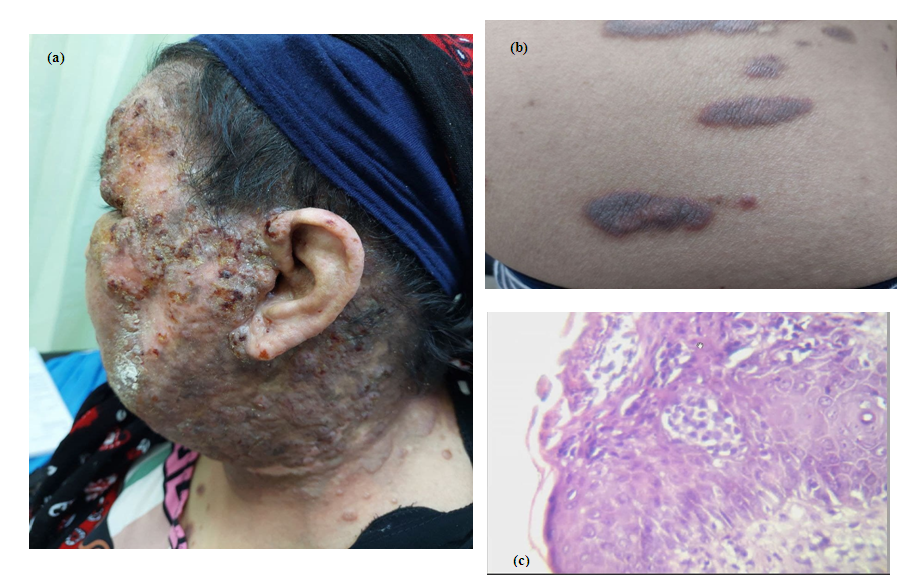
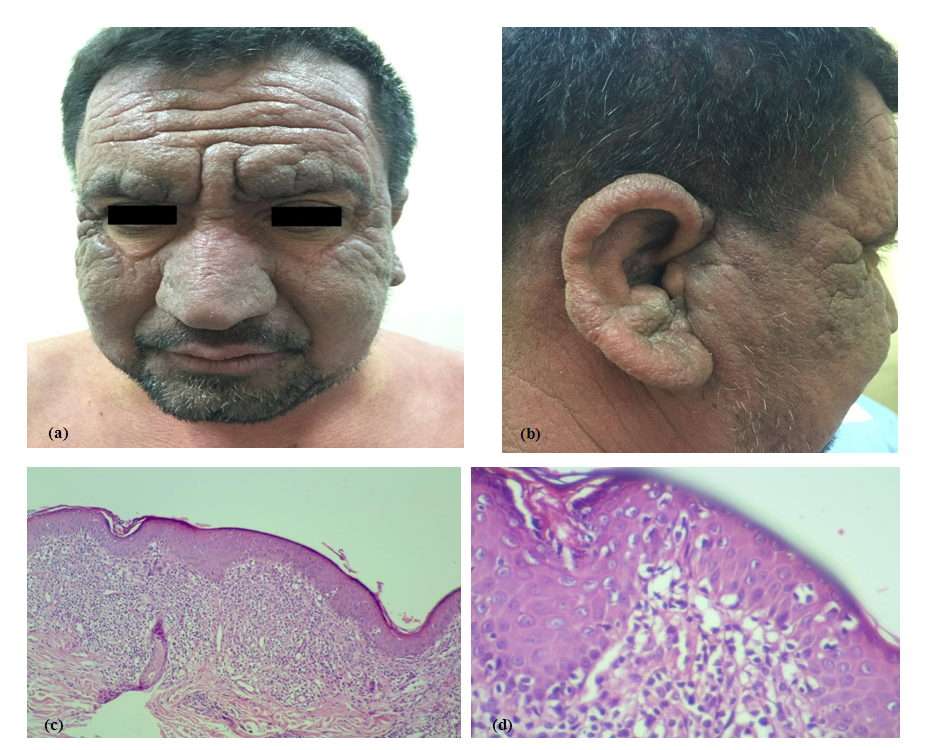 | Figure 1. Mycosis fungoides in a 45 year old male. (a) Leonine face, (b) Infiltrating lesions involving the ears, (c) Lichenoid infiltration of atypical lymphocytes (H&E stain x40), (d) Pautrier microabscess (H&E stain x400) |
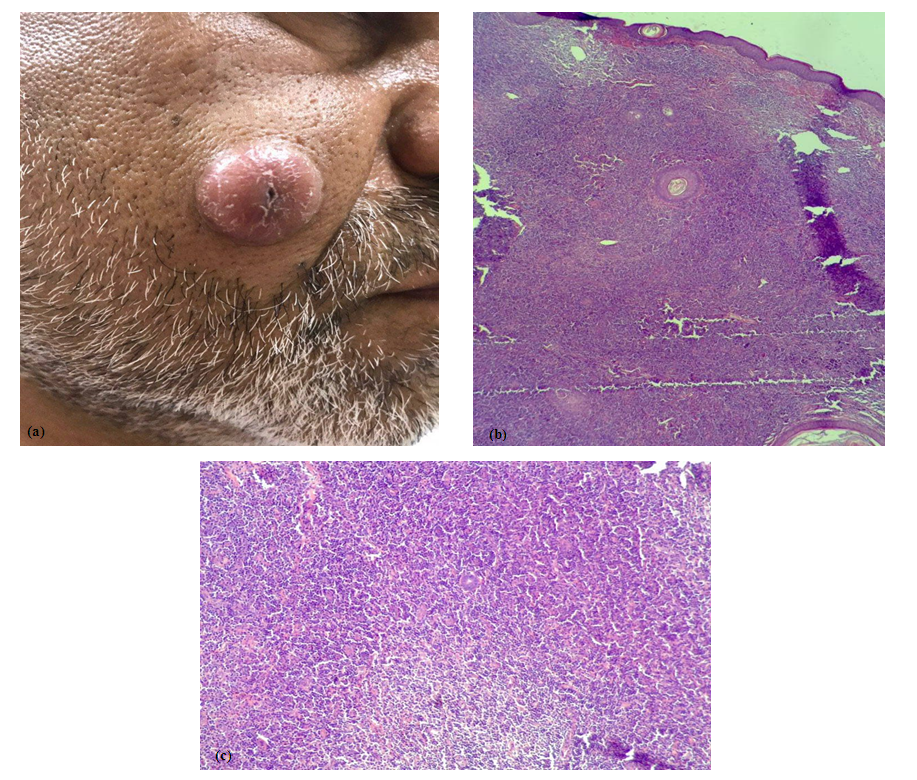
 | Figure 2. (a, b) Mycosis fungoides in a 35 year old female, tumor stage. (c) Heavy dermal infiltration of atypical lymphocytes and Pautriar microabscess. (H&E stain x400) |
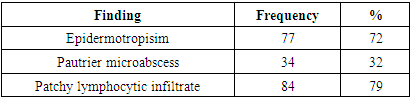
 | Figure 3. (a) Primary cutaneous B-cell lymphoma in 55-year-old male; (b) H&E stain x40 shows heavy dermal infiltrate; (c) H&E stain x400 shows the cellular morphology |
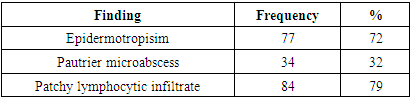
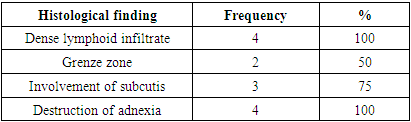
The histopathological characteristics of MF are shown in table 4, epidermotropism was the most common finding in MF while in the patient with EN-NKTCL there was atypical lymphoid and mixed inflammatory infiltration destructing the nasal mucosa and the cartilage. Histopathology of patient with PCALCL demonstrated massive expansion of the dermis with dense diffuse large atypical lymphocytic infiltration with high mitotic figure. Dense lymphoid infiltrate was the most common finding in PCBCL and SCL (table 5, 6).Table (4). Histopathological characteristics of mycosis fungoides
 |
| |
|
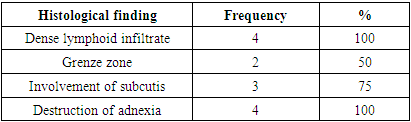
Table (5). Histopathological characteristics of four cases of PCBCL
 |
| |
|
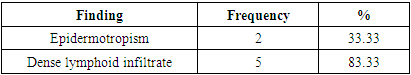
Table (6). Histopathological characteristics of six cases of SCL
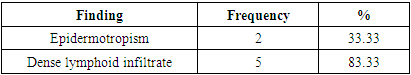 |
| |
|
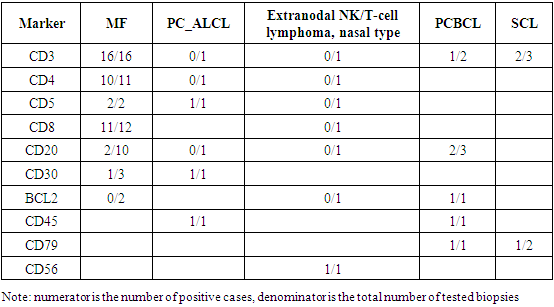
Immunohistochemistry was performed to some biopsies and showing that in MF all were CD3 positive, CD4 was positive in 10/11 and CD8 was positive in 11/12, other results are shown in Table 7.Table (7). Immunohistochemistry of some of selected biopsies
 |
| |
|
5. Discussion
Cutaneous lymphomas are a heterogeneous group of extranodal non-Hodgkin lymphomas representing nearly 20% of all extranodal non-Hodgkin lymphoma [3].Cutaneous lymphomas affect predominantly middle-aged and elderly people, different types of lymphoma are associated with certain age distribution, in the present study the mean age at diagnosis was highest in PCBCL with a mean of 67.4 years followed by secondary cutaneous lymphoma with a mean of 58.4 years and then CTCL with a mean of 44.3 years [1].In the present study, there was a slight male predominance with a male to female ratio of 1.2:1 which was consistent with global male predominance in all types of cutaneous lymphoma [4].In the present study, the most prevalent cutaneous lymphoma was PCTCL (90%) and mycosis fungoides was the most common type (98% of PTCL), with only one case of CD30 positive primary cutaneous anaplastic large cell lymphoma and one case of extranodal NK-T cell lymphoma, nasal type.In the Western world, CTCL constitute approximately 75%-80% of all primary cutaneous lymphomas, MF is the most common type and accounts for 60% of CTCL and almost 50% of all primary cutaneous lymphomas [5].Regarding MF in the present study, about 2.8% of cases were younger than 18 years at the time of diagnosis, the prevalence of childhood MF among different studies ranged from 2.7% to 16.6%, so the finding was compatible with other reports [6]. Regarding clinical morphology of cutaneous lymphoma, cases of MF were mostly patches and plaques reflecting an early-stage disease, most of the patients were at stage 1A or 1B which is similar to other studies conducted in the middle east and Europe [7] while studies from the USA demonstrated later stages at time diagnosis [3]. Nodular stage MF represented an uncommon finding and was found only in 8% of the patients. other variants include poikiloderma (19.26%), hypopigmented MF (12.8%), and erythroderma in 3.66% which are comparable with previous studies in the neighboring countries [6,7]. The diversity in clinical morphology of early MF makes the diagnosis of this disease a challenge to dermatologists.Hyperpigmented MF is an uncommon, clinical variant of MF, with a predilection for dark-skinned people. Sharquie et al 2020 [8] described the clinicopathological features of 12 patients with hyperpigmented MF. In the present study, there were 16 patients with hyperpigmentation that were associated with melanin incontinence on histopathology.In the present study, we reported a case of extranodal NK-T cell lymphoma in an 18 year old female presented with progressive ulcerated and necrotic mucocutaneous lesions. Of the rare cases, primary cutaneous anaplastic large cell lymphoma was diagnosed in a 36-year-old male with nodular and ulcerated skin lesions located in the dorsum of the foot. These findings are similar to the reported cases in the literature [9,10].Regarding histopathology of MF, the most common finding in the present study was epidermotropism and patchy lymphocytic infiltrate, while lichenoid infiltrates were present in 21.5%, with variable degree of hyperkeratosis and atrophy, liquefactive degeneration of the basal layer, and melanin incontinence in most cases. fibrosis was rare, present in only 1.8% of cases, also granulomatous reaction in only one case. These findings were comparable to other studies with the exception of fibrosis which was less common than previous studies [11,12].Concerning immunohistochemistry, the characteristic feature of MF is the expression of CD4, the marker of T-helper cells. Common MF immunophenotype is CD3 positive, CD4 positive, CD8 negative, and CD7 negative. In the present study, 16 cases were examined for CD3 and they were all positive, 12 cases were examined for CD8, and 10 were positive. Some studies suggest that the presence of CD8 positive lymphocytes in MF is associated with nonaggressive biological course [13].Regarding PCBCL in the present study patients presented with nodules and plaques which is the usual presentation of the disease [14].On histopathology, all cases showed dense diffuse atypical lymphocytic infiltrate with involvement of subcutis and adnexal destruction, one case was of primary diffuse large B cell lymphoma which was regarded as aggressive type unlike other indolent types of PCBCL. According to WHO classification, PCBCL constitutes 25% of all cutaneous lymphoma and was classified according to the stage of maturation of lymphocytes [15].The clinical characteristics of secondary cutaneous lymphoma remain poorly understood due to the small number of published studies and relatively small sample size. Consequently, while the epidemiology, relative frequency, clinical manifestations of primary cutaneous lymphoma are well understood, this is not true for secondary cutaneous lymphoma [2].In the present study patients with secondary cutaneous lymphoma were diagnosed with non-Hodgkin lymphoma months to a few years before the appearance of secondary cutaneous lesions. Three cases had DLBCL and 2 cases had non-Hodgkin lymphoma T-cell type while the remaining 2 cases were non-Hodgkin lymphoma unspecified. The trunk was mainly involved in most cases while the scalp was involved in three cases. Lee et al 2015 [2] found that T-/NK-cell lineage lymphoma most commonly affected the extremities while B-cell lineage lymphoma most commonly affected the trunk. In the present study the most common clinical manifestations of secondary cutaneous lymphoma were nodules followed by the plaques and one case had ulceration, Lee et al 2015 [2] found that nodules were the most common manifestation in both T-/NK-cell lineage and B-cell lineage SCL, extranodal NK/T-cell lymphoma commonly presented as cellulitis-like swollen or ulcerated patches.In secondary cutaneous lymphoma most of our cases on the histopathological examination showed dense diffuse atypical lymphocytic infiltrate destructing the adnexa and extending deep to the panniculus with a single filing arrangement of the tumor cells and Grenz zone in some biopsies. Other studies [16] revealed that skin involvement is relatively common in both B and T-cell NHLs. The histopathological characteristics were relevant to the primary type of lymphoma.
References
| [1] | Kempf W, Zimmermann AK, Mitteldorf C. Cutaneous lymphomas—An update 2019. Hematol Oncol [Internet]. 2019 [cited 2021 May 25]; 37(S1): 43–7. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/hon.2584. |
| [2] | Lee WJ, Won KH, Won CH, Chang SE, Choi JH, Moon KC, et al. Secondary cutaneous lymphoma: comparative clinical features and survival outcome analysis of 106 cases according to lymphoma cell lineage. Br J Dermatol. 2015 Jul; 173(1): 134–45. |
| [3] | Bradford P, Devesa S, Anderson W, Toro J. Cutaneous lymphoma incidence patterns in the United States: a population-based study of 3884 cases. Blood. 2009 Mar 1; 113: 5064–73. |
| [4] | Olsen EA. Evaluation, Diagnosis, and Staging of Cutaneous Lymphoma. Dermatol Clin. 2015 Oct; 33(4): 643–54. |
| [5] | Burg G, Kempf W, Cozzio A, Feit J, Willemze R, S Jaffe E, et al. WHO/EORTC classification of cutaneous lymphomas 2005: histological and molecular aspects. J Cutan Pathol. 2005 Nov; 32(10): 647–74. |
| [6] | Fatemi Naeini F, Abtahi-Naeini B, Sadeghiyan H, Nilforoushzadeh MA, Najafian J, Pourazizi M. Mycosis fungoides in Iranian population: an epidemiological and clinicopathological study. J Skin Cancer. 2015; 2015: 306543. |
| [7] | Alsaleh QA, Nanda A, Al-Ajmi H, Al-Sabah H, Elkashlan M, Al-Shemmari S, et al. Clinicoepidemiological features of mycosis fungoides in Kuwait, 1991-2006. Int J Dermatol. 2010 Dec; 49(12): 1393–8. |
| [8] | Sharquie K, Al-Jaralla F, Al-Saadawi A. Hyperpigmented lichenoid mycosis fungoides as a new variant: clinical and histopathological evaluation. Our Dermatol Online. 2020 Nov 3; 11: e168.1-e168.5. |
| [9] | Kempf W, Kerl K, Mitteldorf C. Cutaneous CD30-positive T-cell lymphoproliferative disorders-clinical and histopathologic features, differential diagnosis, and treatment. Semin Cutan Med Surg. 2018 Mar; 37(1): 24–9. |
| [10] | Li S, Feng X, Li T, Zhang S, Zuo Z, Lin P, et al. Extranodal NK/T-cell lymphoma, nasal type: a report of 73 cases at MD Anderson Cancer Center. Am J Surg Pathol. 2013 Jan; 37(1): 14–23. |
| [11] | Al-Hamamy HR, Sharquie KE, Noaimi AA, Abdulwahhab WS. Mycosis Fungoides in Iraqi Patients—Clinical, Histopathological and Immunohistochemical Study. J Cosmet Dermatol Sci Appl [Internet]. 2015 Mar 20 [cited 2021 Nov 19]; 5(2): 116–24. Available from: http://www.scirp.org/Journal/Paperabs.aspx?paperid=57128. |
| [12] | Mufti S. Morphological pattern of mycosis fungoides 2013. 2013 Oct 25; 7: 133–41. |
| [13] | Jj C, Ra C, R W, Ts K. Sezary syndrome and mycosis fungoides arise from distinct T-cell subsets: a biologic rationale for their distinct clinical behaviors. Blood [Internet]. 2010 May 18 [cited 2021 May 27]; 116(5): 767–71. Available from: https://europepmc.org/article/MED/20484084. |
| [14] | Kempf W, Kazakov DV, Mitteldorf C. Cutaneous lymphomas: an update. Part 2: B-cell lymphomas and related conditions. Am J Dermatopathol. 2014 Mar; 36(3): 197–208; quiz 209–10. |
| [15] | The 2018 update of the WHO-EORTC classification for primary cutaneous lymphomas | Blood | American Society of Hematology [Internet]. [cited 2021 May 1]. Available from: http://985.so/b8ree. |
| [16] | Khurana A, Al-Juhaishi T, Shafer D. Secondary Skin Involvement in Non-Hodgkin’s Lymphoma Does Not Impact Outcomes: SEER Database Analysis. Blood [Internet]. 2018 Nov 29 [cited 2021 Nov 23]; 132: 2895. Available from: https://www.sciencedirect.com/science/article/pii/S000649711938944X. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML