-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2021; 10(3): 31-43
doi:10.5923/j.ajdv.20211003.01
Received: Nov. 9, 2021; Accepted: Dec. 7, 2021; Published: Dec. 29, 2021

Management of Pruritus in Indian Settings: An Expert Opinion
Kiran Godse1, Prabhakar M. Sangolli2, Abhishek De3, Nidhi Sharma4, Mukesh Girdhar5, Krupa Shankar6, Bela Shah7, Sushil Tahiliani8, Vijay Zawar9, Roheet Rathod10, Rahul Rathod10
1D.Y. Patil University School of Medicine, Shree Skin Centre and Pathology Laboratory, Navi Mumbai, India
2Department of Dermatology, East Point College of Medical Sciences and Research Centre, Bangalore, India
3Department of Dermatology, Calcutta National Medical College, Kolkata, India
4Medanta Hospital, Gurugram, Gurgaon, India
5Department of Dermatology, Max Superspecialty Hospital, Patparganj, New Delhi, India
6Mallige Hospital, Bangalore, India
7Department of Dermatology, Venereology and leprology, B.J Medical College and Civil Hospital, Ahmedabad, India
8Hinduja Hospital and MRC, Nail Society of India, Mumbai, India
9Skin Diseases Center, Nashik, India
10Dr. Reddy Laboratories, Hyderabad, India
Correspondence to: Roheet Rathod, Dr. Reddy Laboratories, Hyderabad, India.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Pruritus is a very frequently seen cutaneous symptom in current dermatological practice. It exerts a significant impact on overall quality of life of a person. The current consensus article aims at describing clinical views of expert dermatologists, regarding various aspects of pruritus including classification, pathophysiology, diagnosis, along with appropriate management. A literature search was performed using databases Pubmed and Google Scholar. Relevant articles were identified using keywords like ‘pruritus’, ‘antihistamine’ and ‘itch’. After screening, 46 relevant articles were identified and included in the document. Effective diagnosis of pruritus includes a comprehensive patient history and physical examination for determining whether pruritus is due to a dermatologic disorder or an underlying systemic disease. This could be followed by basic investigations and subsequent suitable therapy approaches. General care measures are essential for every patient with pruritus. Various topical therapies used for pruritus include local anaesthetics, pramoxine, capsaicin, calcineurin inhibitors, menthol, camphor, zinc, doxepin, corticosteroids and palmitoyl-ethanol-amine. With respect to systemic therapies, oral antihistamines (e.g. hydroxyzine) are generally the first line of treatment for pruritus. The other systemic therapies include gabapentin and pregabalin, tricyclic antidepressants, doxepin, mirtazapine, naltrexone, cyclosporine and ultraviolet (UV) phototherapy. The current manuscript provides a collation of evidence-based literature and clinical insights of the expert dermatologists.
Keywords: Pruritus, Antihistamine, Itch, Hydroxyzine
Cite this paper: Kiran Godse, Prabhakar M. Sangolli, Abhishek De, Nidhi Sharma, Mukesh Girdhar, Krupa Shankar, Bela Shah, Sushil Tahiliani, Vijay Zawar, Roheet Rathod, Rahul Rathod, Management of Pruritus in Indian Settings: An Expert Opinion, American Journal of Dermatology and Venereology, Vol. 10 No. 3, 2021, pp. 31-43. doi: 10.5923/j.ajdv.20211003.01.
Article Outline
1. Introduction
- Pruritus has been reported as the most common clinical symptom in dermatology. [1] It still continues to be a difficult condition to diagnose and manage. Visible skin lesions are not observed in all cases, and pruritus could be a dermatologic manifestation of any systemic disease. It most frequently results from xerosis, eczema or cutaneous infections like tinea. However, systemic differential diagnosis extends as far as cirrhosis, hematologic disorders, infection, drug reactions, and malignancy. [2] It is frequently ignored, and has the potential to drastically compromise quality of life by causing several problems related to sleep, anxiety or attention. [1,2]Histamine is the primary mediator of pruritus in various disorders. [3] However, pruritus is transmitted along both histaminergic and non-histaminergic pathways with a multifaceted interplay between keratinocytes, immune cells and cutaneous neurons. It is crucial to take a detailed patient history, perform a focused physical examination, form structured differential diagnosis and perform suitable investigations. Treatment involves several therapies like antihistamines to aid in alleviating this distressing symptom. [4] The current article aims at providing an evidence-based overview and expert opinion on effective diagnosis and management of pruritus in routine in-clinic patient care in India.
2. Definition of Pruritus
- In literature, pruritus is described as an unpleasant feeling that causes a desire to scratch. This in turn, negatively affects psychological and physical aspects of life. [5] Pruritus significantly impacts quality of life (QoL), which subsequently results in several problems related to sleep, attention, anxiety, and sexual and social function. [1] It is the most frequently seen symptom of skin diseases, sometimes trivial or less and sometimes intolerable. Pruritus might exist continuously or occur intermittently. The site of occurrence could be local or generalized. [5]
2.1. Consensus Opinion
- The panel described pruritus as an unpleasant sensation of the skin that elicits the desire to scratch. They also added that it affects the quality of life of an individual.
3. Prevalence of Pruritus
- The prevalence of acute and chronic pruritus in general population is 8.4% and 13.5% respectively. The lifetime prevalence of chronic pruritus in general populations is 22%. This implies that more than 1 in 5 people experience chronic pruritus once in their life. [6] An increase in prevalence of chronic pruritus is associated with advancing age. A proportion of 60% of elderly population aged ≥65 years is affected by moderate-to-severe pruritus. [1]In Indian settings, pruritus is an important symptom seen along with superficial dermatophytosis. Verma et al. reported that majority of patients with superficial dermatophytosis experienced pruritus, with 89.9% complaining of pruritus limited to skin lesions. Severe and very severe itch was reported by 74.7% of patients.7 However, there is insufficient data regarding prevalence of pruritus in India. [1]
3.1. Consensus Opinion
- According to the panel experts, prevalence of pruritus might be higher in Indian settings; however, there is a lack of published evidence. Also, pruritus is a common complaint in elderly patients. In the last few years, a rise in dermatophytosis has been reported to be a major cause of pruritus in Indian clinical practice.
4. Classification of Pruritus
- In simple terms, pruritus can be classified as acute (≤6 weeks) or chronic (>6 weeks) forms as per duration. [8] Pruritus covers a wide range of clinical complaints including dermatologic, neurologic, systemic, and psychiatric diseases. In majority of cases, origin of pruritus is in the skin or/and nervous system. According to the peripheral and central nervous systemic mechanisms, pruritus could be divided into various categories. [5]Pruritoceptive or dermatologic pruritus could be caused due to dermatological disorders like dermatophytosis, xerosis, scabies, urticaria, reactions to insect bite and dermatoses such as atopic dermatitis and psoriasis. [1,2] It is transmitted by slow, unmyelinated group C nerve fibres and A delta fibres. In dermatologic pruritus, keratinocytes interact with pruritogens like histamines and many others. Systemic pruritus occurs from non-cutaneous organ systems with a central nervous system transmission and no peripheral nerve input. [2] The causes include: [5,8]• Metabolic and endocrine diseases like chronic renal insufficiency, liver diseases, hyperparathyroidism, hyperthyroidism, iron deficiency etc.• Diabetic pruritus (may be associated with primary problems of skin like xerosis or secondary problems like candidiasis and xerosis cutis, small fibre neuropathy (SFN) in diabetic individuals).• Infective diseases like acquired immune deficiency syndrome (AIDS) and parasitosis.• Haematological disorders like polycythaemia vera, myelodysplastic syndrome, lymphoma etc.• Neurological disorders like multiple sclerosis and brain tumours, etc.Neuropathic pruritus involves pathological alterations in the afferent pathway of sensory nerve fibres. The coverage is limited to a certain point. For instance, postherpetic neuralgia is frequently accompanied by itching. [5] Furthermore, psychogenic pruritus results from disorders of the mind like obsessive-compulsive disorder, depression, anxiety, somatic symptom disorders, psychosis and substance use. [2] Lastly, mixed pruritus occurs owing to multiple factors and is mediated by two or more mechanisms. For instance, atopic dermatitis (AD) involves skin derived itching and neurogenic pruritus. [5]
4.1. Consensus Opinion
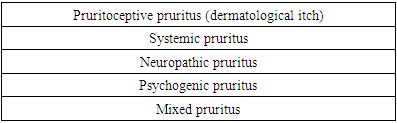
- The clinical classification suggested by panel experts is listed in Table 1.
|
5. Pathophysiological and Neurobiological Aspects of Pruritus
- Pruritus starts in the epidermis and dermo-epidermal junction, and involves a complex interplay between activated unmyelinated C nerve fibers, immune cells and keratinocytes. Numerous pruritogens including proteases, cytokines, prostaglandins, neuropeptides, nerve growth factor and histamine are released. Various pruritic receptors including protease-activated receptors and ion channel receptors are also activated. [4]
5.1. Initiation of Itch
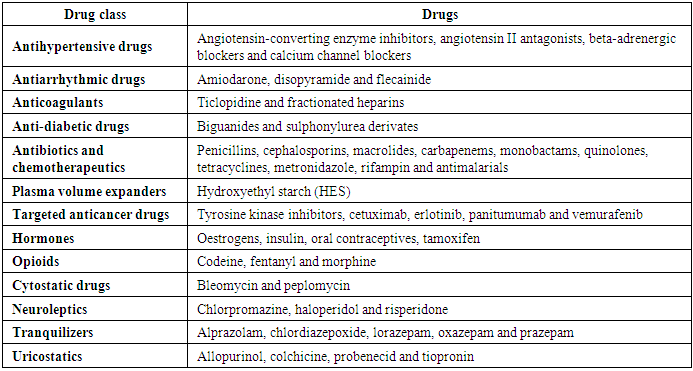
- Allergens, pruritogens and irritants contact the skin in acute and chronic pruritus. Branching terminal fibers of afferent neurons sense these substances and reach the epidermis. The sensory neurons are histaminergic or non-histaminergic. Neural activity enables recruitment of immune cells like mast cells and CD4+ T cells. These cells release mediators that activate cognate receptors on sensory neurons, which in turn release neuropeptides contributing to the ‘itch-scratch cycle’. Messages are transmitted from peripheral afferents to their cell bodies in the dorsal root or trigeminal ganglia. This is followed by synapsing with second order neurons in the spinal cord. Lastly, thalamus aids in interpretation of messages encoding pruritus (Figure 1). [9]
 | Figure 1. Initiation of itch (Adapted from Cevikbas F et al. Physiol Rev. 2020;100(3): 945-982) |
5.2. Concept of Neuronal Sensitization
- Chronic itch is commonly accompanied by allokinesis and hyperkinesis, which are likely caused by ‘neural sensitization.’ This denotes changes in sensitivity of itch-processing neurons. Numerous factors acting at targets in the skin, spinal cord, or brain could induce neural sensitization (Figure 2). [11]
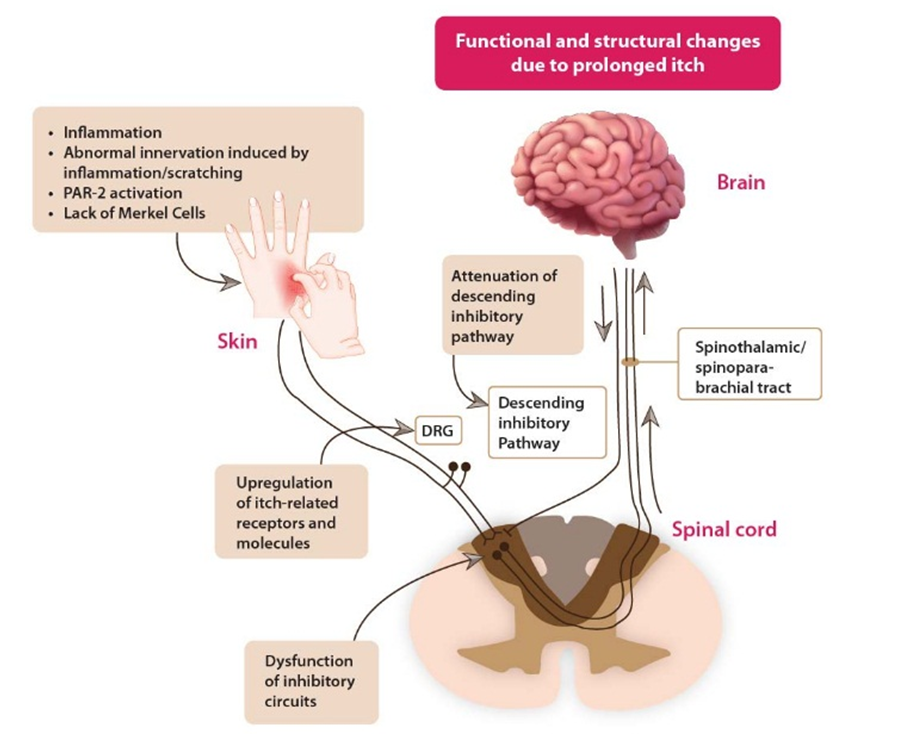 | Figure 2. Neural sensitivity to pruritus. DRG, dorsal root ganglion; PAR: Protease-activated receptor. (Adapted from Yosipovitch G et al. J Allergy Clin Immunol. 2018; 142(5): 1375-1390) |
5.3. Neurobiological Aspects of Pruritus
- Pruritus is encoded by genetically distinct neurons both in the peripheral nervous system (PNS) and central nervous system (CNS) to elicit a characteristic behavioural response namely, scratching. [12] Presently, theories like “selectivity” and “labeled-line” describe how itch is transmitted to the brain. [13] The “selectivity” theory hypothesizes that most fibers respond only to painful stimuli, while some respond to both pain and itch stimuli. The greater population of pain-related C-fibers imposes an inhibitory influence on the smaller population of itch-sensitive C-fibers. Itch is only perceived when the itch transmitting C-fibers are selectively activated. If a stimulus activates itch and pain both, C-fiber neurons transmitting the pain signal will mask the itch input. When the pain pathway is activated, it inhibits any itch sensation from the dual-modal pathway. [14] The “labeled-line” theory supports presence of afferent fibers exclusively responsive to pruritogenic stimuli. [13] There is evidence for spinal neurons that particularly transmit itch signals. [14]
5.4. Consensus Opinion
- The panel experts agreed that pruritus involves a release of pruritogens. Pathophysiology of acute and chronic pruritus differs from each other. An itch could occur owing to various underlying mechanisms. It is transmitted to the cortex through a subset of polymodal fibers that are more selective toward pruritogens.
6. Most Common Etiological Factors Associated with Pruritus
6.1. Dermatological Disorders
- While approaching a patient with pruritus, one must first consider various causative skin disorders. Xerosis is a cause of significant pruritus. In atopic dermatitis, involved regions are quite pruritic. Papules might appear with variable degrees of lichenification dependent upon the amount of scratching. [15] Moreover, pruritus is the most frequent presenting symptom in individuals with disorders caused by ectoparasites like scabies or pediculosis. [16] In the Indian context, dermatophytosis is an important aetiology of acute pruritus. [7] Various other dermatological conditions causing pruritus include dermatitis herpetiformis, urticaria, psoriasis, lichen planus, contact dermatitis, insect bites, sunburns, polymorphous light eruption, pityriasis rosea and many more. [15]
6.2. Systemic Diseases
- Among all systemic diseases causing pruritus, chronic kidney disease is possibly the most common underlying pathology. Uremic pruritus is a frequent complication in terminal renal disease patients. Pruritus affects 50–90% individuals undergoing peritoneal dialysis or hemodialysis. [17] Diabetes mellitus could be associated with pruritus which is mostly localized. It is more likely to occur in diabetic patients who have dry skin or diabetic neuropathy. [18] Hepatic cholestasis is another causative factor of pruritus in many diseases. Almost all patients with primary biliary cirrhosis exhibit pruritus. [15] Endocrine disorders like thyrotoxicosis and hypothyroidism also cause pruritus. [17] Additionally, pruritus could also be drug-induced. Drugs like chloroquine, opioids, antihypertensive drugs and others could induce pruritus.19 Similarly, pruritus is a common dermatological adverse event across different categories of targeted anticancer therapies like tyrosine kinase inhibitors. [20]
6.3. Hematopoietic Disorders
- Various hematopoietic diseases have been associated with pruritus. Patients with polycythaemia vera commonly have pruritus that is aggravated by hot baths. Almost 50% patients with Hodgkin’s disease might have pruritus. Multiple myeloma, mastocytosis, and iron-deficiency anaemia may also present with pruritus. [15]
6.4. Neuropathic Causes
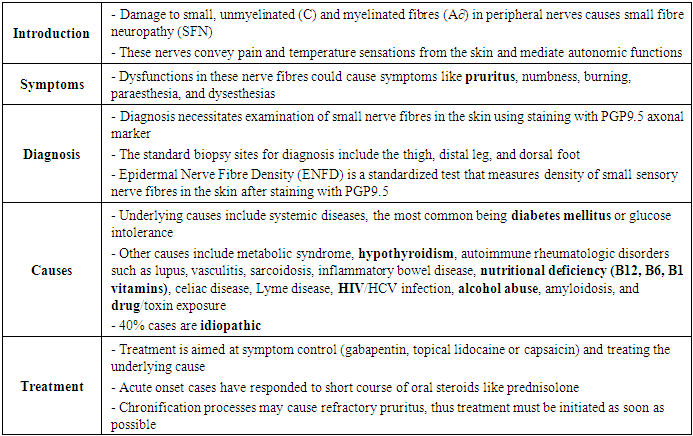
- Neuropathic itch results due to an itch arising anywhere along the afferent nerve pathway due to damage of the nervous system. It is characteristically observed in post herpetic pruritus, multiple sclerosis, and brain tumours. [15] Conditions affecting the peripheral nervous system like small fiber neuropathy, scars and burns, radiculopathies and postherpetic neuralgia are associated with neuropathic itch. [21] In small-fiber neuropathy, pruritus might be localized or generalized, and could occur due to infectious, autoimmune, genetic diseases and drugs. [21] A comprehensive overview on small-fiber neuropathy is provided in Table 2. [22] Scars and burn injuries could be associated with pruritus owing to damage of cutaneous nerves. Postherpetic neuralgia is a common aetiology of neuropathic itch at the site of the affected peripheral nerve. Also, compression or irritation of different neural structures might induce localized neuropathic itch along the corresponding dermatome (brachioradial pruritus, notalgia paresthetica, cheiralgia paresthetica etc.). At central level, space-occupying lesions like abscesses, cysts, tumours, vascular malformations or syringomyelia may initiate neuropathic itch. [21]
|
6.5. Psychological Causes
- Psychogenic itch can be described as an itch disorder where psychological factors play an evident role in triggering, intensity, aggravation, or persistence of pruritus. [23] It classically presents with excessive impulses to scratch at otherwise normal skin. [14] Many psychiatric diagnoses like depression, obsessive compulsive disorder, anxiety, mania, psychosis, and substance abuse have been associated with pruritus. [14]
6.6. Pruritus of Unknown Origin
- In certain cases, the underlying cause remains unclear, and is called pruritus of unknown cause/origin. It is a diagnosis of exclusion and patients are re-assessed periodically to try to identify potential causes for symptoms. [24]
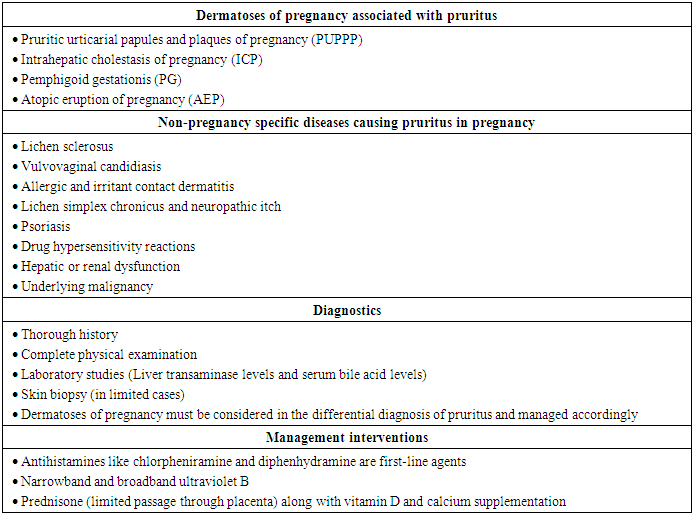
6.7. Pruritus in Pregnancy
- Pruritus is the major dermatological symptom in pregnancy, occurring in about 18% of pregnancies. [25] A comprehensive overview on pruritus in pregnancy is given in Table 3. [26,27]
|
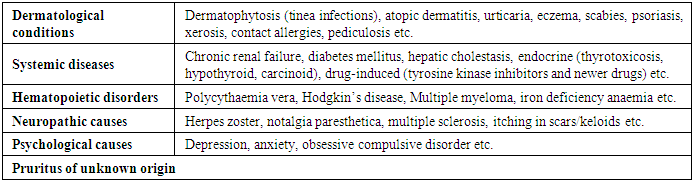
6.8. Consensus Opinion
- According to the panel experts, most common causes of pruritus in Indian settings are mentioned in Table 4. They also added that failure of early diagnosis and prompt treatment of small-fiber neuropathy may lead to refractory pruritus, with secondary changes like excoriation, lichenification etc. Hence, awareness of this underdiagnosed condition is necessary for optimal treatment of chronic pruritus.
|
7. Assessment of the Severity and Patient Quality of Life (QoL)
- Since pruritus is a multifactorial subjective symptom, assessment might be a challenge. Various scales are available for assessing pruritus intensity. The mono-dimensional scale such as visual analogue scale (VAS) is a simple method of indicating intensity of pruritus with the help of a 10 cm long, ruler-shaped scale. Both endpoints are marked with a number corresponding to intensity, with 0 representing “no itch” and 10 the “worst imaginable itch”. Tools like the Dynamic Pruritus Score and Itch-Free Days questionnaire allow a closer evaluation of patient responses to treatment. [28] The multidimensional 5-D itching scale evaluates numerous components of chronic pruritus, including affected areas of the body, itch intensity, course of itch throughout the day, disability induced by pruritus and whether or not the symptom has changed in the past few weeks, and if so, how (5-D's: degree, duration, direction, disability and distribution). [28] Also, the 12-Item Pruritus Severity Score (12-PSS) is a reliable score that has been validated in patients with chronic pruritus. It could prove to be a useful tool in clinical trials as well as daily routine practice for qualifying patients for antipruritic therapy and assessing efficacy of therapy. [29]Furthermore, certain tools are available for assessing QoL in affected patients. The Dermatology Life Quality Index (DLQI) is one such widely used and validated tool. [29] The usefulness of DLQI has been established for patients with pruritic conditions of cutaneous origins. [28] Additionally, ItchyQol has been developed specifically for pruritic conditions and focuses on the effect of pruritus on day-to-day activities, characteristics of symptoms and the level of psychological strain. The Hospital Anxiety and Depression Scale (HADS) is most broadly used to assess psychiatric comorbidities like anxiety and depression, which often accompany chronic pruritus. [28]
7.1. Consensus Opinion
- According to the panel experts, the visual analogue scale (VAS) and Dermatology life Quality Index (DLQI) are the most common tools used in the Indian settings. In addition, tools like the Dynamic Pruritus Score, Itch-Free Days questionnaire, 12-PSS and ItchyQoL might aid in assessing various parameters of severity, QoL and treatment response.
8. Essential Diagnostic Approaches for Pruritus
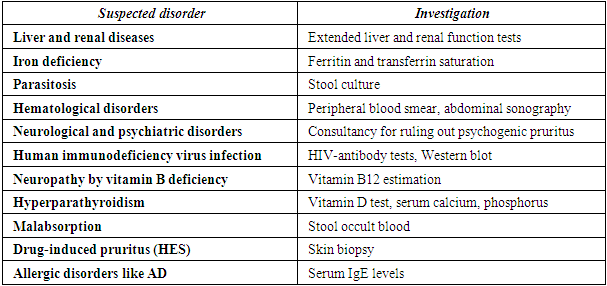
- Assessing a patient with pruritus must initially involve thorough history and physical examination of the skin. A detailed history including past medical, family and drug history can aid in further diagnosing underlying conditions. [30] Onset, duration of pruritus, quality, time course, localization, preceding skin changes, relieving factors, exacerbating factors, atopic diathesis, history of allergies, weight loss, fever, fatigue, emotional stress, and other symptoms indicating underlying disease need to be reviewed. [1] Presence of a primary skin lesion may indicate a dermatologic cause. The history must include recent exposures to new topical, oral, or airborne substances that could result in skin lesions. New cosmetics or creams could trigger dermatological conditions like allergic contact dermatitis, urticaria, and photodermatitis. New medications, nutritional supplements or illicit drugs could cause urticaria or fixed drug eruptions. [3] Drugs that could induce pruritus are listed in Table 5. [19,20,25,30,31]
|
8.1. Consensus Opinion
- The panel experts opined that the initial clinical approach in patients with pruritus mainly involves a comprehensive patient history. Additionally, physical examination was essential for determining whether pruritus is due to a dermatologic disorder or is secondary to an underlying systemic disease. They also added that drug history was crucial in cases of acute pruritus.
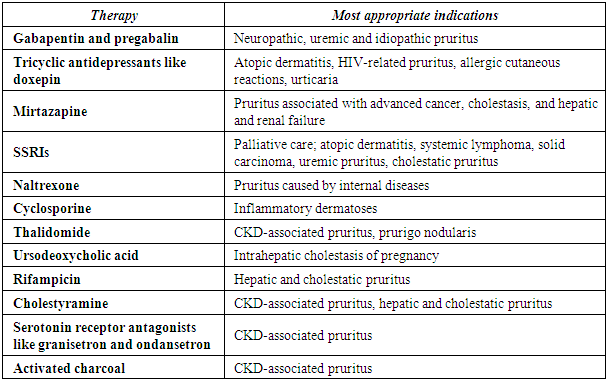
9. Investigations and Screening Tests for Chronic Pruritus
- Investigations could be performed to determine any underlying condition. [25] Screening tests and investigations like fasting blood sugar, postprandial blood sugar, complete blood count, erythrocyte sedimentation rate, absolute eosinophil count, peripheral smear, urinalysis, stool routine and occult blood, thyroid-stimulating hormone (TSH), free T4, liver function test, creatinine, aspartate aminotransferase (AST), alanine transaminase (ALT), alkaline phosphatase, and bilirubin could be performed. [1]If primary skin lesions like erythema, vesicles, blisters, pustules or wheals are noticeable and, according to the patient history, have been present since onset of itch, pruritus on primarily inflamed skin can be diagnosed. Further investigations could be performed accordingly. These include skin biopsy, microbiological investigations and, in certain cases, laboratory testing like serum IgE and indirect immunofluorescence. If a patient with chronic pruritus reports no visible skin lesions at onset, pruritus on primarily non-inflamed skin can be diagnosed. A systemic disease, medications, pregnancy or particular skin diseases could be causative. Based on patient history and pre-existing diseases, laboratory and radiological investigations are obligatory for a definitive diagnosis. [25]Disease-specific investigations are mentioned below:• In all cases of generalized pruritus without rash, full blood count and ferritin levels must be checked. [32]• Patients with generalized pruritus with suspicion of haematological involvement must have initial investigations including full blood count, blood film, lactate dehydrogenase and ESR. [32]• Patients with generalized pruritus must not undergo routine endocrine investigations unless they present with additional clinical features suggesting diabetes, other endocrinopathy or renal disease. [32]• In cases of suspected renal insufficiency, creatinine (and urea for elderly), phosphate, parathyroid hormone (PTH), bicarbonate, urinalysis, urine protein concentration and sonography, computed tomography (CT) or magnetic resonance imaging (MRI) of the kidneys are advised. [1]• In cases of suspected liver diseases with or without cholestasis, γ-GT, arterial pressure (AP), bilirubin, AST, ALT (and hepatitis B-, hepatitis C-antibodies, if a risk-patient), lactate dehydrogenase (LDH), antimitochondrial antibodies (AMAs), antinuclear antibody, anti-hepatitis B core antibody, hepatitis B surface antigen, anti-hepatitis C virus-antibody, anti-smooth muscle antibody, anti-actin antibody, sonography of the liver, CT or MRI, magnetic resonance cholangiogram or endoscopic retrograde to rule out primary sclerosing cholangitis are advised. [1] • If iron deficiency is suspected, ferritin and transferrin saturation (TSAT) must be done 1.• In cases of suspected malabsorption, serum protein, serum albumin, calcium, blood count, gliadin-antibody, Vitamin A, Vitamin B12 and endoscopy with biopsy are advised. [1] • For neurological diseases, investigations include cerebrospinal fluid analysis, electroencephalogram (EEG), magnetic resonance imaging (MRI), computed tomography (CT) of brain and functional tests for multiple sclerosis; cerebrospinal fluid analysis with histopathology, EEG, MRI, CT of brain for brain tumours; MRI of thoracic spine for notalgia paresthetica and MRI of the thoracic and cervical spine for brachioradial pruritus. [33]• Psychiatric and psychosomatic exploration; psychiatric short questionnaire for depressive and anxiety disorder could be used for psychiatric or psychosomatic diseases. [33]• For suspected drug-induced pruritus, γ-GT, AP, bilirubin, AST, ALT, LDH, and skin biopsy in case of Hydroxyethyl starch (HES) exposition must be performed. [1]• For pruritus of elderly, serum creatinine, ALT, AST, alkaline phosphatase, bilirubin, TSH, full blood count and blood urea nitrogen must be performed. [1]• Stool culture and microscopic examination must be done in cases of parasitoses. [1]
9.1. Consensus Opinion
- According to the panel experts, basic investigations for chronic pruritus could include evaluation of CBC, creatinine, thyroid stimulating hormone (TSH), HbA1c or fasting blood sugar and postprandial blood sugar, liver function test, renal function test, urine examination, chest X-ray, erythrocyte sedimentation rate (ESR) and histopathology. Based on results of the baseline investigations, further extended investigations could be done accordingly (Box 1).
10. General Care Measures for Pruritus
- The general care measures for pruritus include the following: [1,2,25]• Use of lukewarm water baths (maximum 20 min) • Application of moisturizers/emollients (moisturizers / emollients containing anti-pruritic agent like pramoxine may be preferred) • Use of soft clothing permeable to air (like cotton) • Cool environment• Avoidance of irritants• Behavioural therapy, relaxation and stress reduction• Application of mild, non-alkaline, perfume-free soaps, moisturizing syndets and shower/bath oils
10.1. Consensus Opinion
- According to the panel experts, general care measures for pruritus mentioned above, need to be followed meticulously by the patient.
11. Topical Therapies for Pruritus
- The multifaceted generation of itch and automatic scratch response result in the clinically challenging itch-scratch cycle. Currently, there are innumerable therapies available for pruritus. [13] The current section discusses common topical therapies used for managing pruritus.
11.1. Local Anaesthetics
- Local anaesthetics like benzocaine, lidocaine and polidocanol are broadly used for symptomatic treatment of localised forms of neuropathic pruritus, chronic kidney disease (CKD)-associated pruritus, post-burn pruritus, paraneoplastic pruritus, as well as in palliative care setting. [25] Pramoxine is effective in reducing itch in patients with xerosis, uremic pruritus, and psoriasis. It has been used as a single agent, in combination with mild potency topical steroids or lactic acid lotion as well as added to moisturizers/emollients. In a randomized, double-blind, comparative trial in patients suffering from uremic pruritus, application of pramoxine 1% lotion twice daily for 4 weeks significantly decreased pruritus compared to a control lotion and was generally well-tolerated. [34]
11.2. Capsaicin
- Capsaicin is used for managing chronic pruritus, but is not considered suitable for facial and periorificial skin. Also, capsaicin requires frequent reapplication. [1]
11.3. Topical Calcineurin Inhibitors
- Tacrolimus and pimecrolimus have proved to be effective in decreasing pruritus in patients with AD, chronic irritant hand dermatitis, rosacea, lichen sclerosis, anogenital pruritus, and prurigo nodularis. These drugs regulate T-cell activation and inhibit release of several inflammatory cytokines. [34]
11.4. Menthol, Camphor, and Zinc
- Menthol, camphor, and zinc have established rapid onset of action and short duration of relief. They can be applied on widespread areas with no significant risk of systemic toxicity. [1]
11.5. Tricyclic Antidepressants Like Doxepin
- Doxepin 5% cream significantly reduces pruritus in patients with AD, lichen simplex chronicus, contact dermatitis and nummular dermatitis. However, drowsiness occurs in around 20-25% of patients, limiting its use, particularly in children. [35]
11.6. N-palmitoylethanolamine
- Emollients containing endogenous lipid N-palmitoylethanolamine (0.3%) significantly enhance skin barrier function and have weak-to-moderate antipruritic and analgesic effects in experimentally induced pain, pruritus and erythema by topical application. [25]
11.7. Topical Glucocorticosteroids
- Topical glucocorticosteroids are the first line therapy for inflammatory dermatoses, but are not recommended for treating pruritus in the absence of a skin disease. [25] Misuse of topical corticosteroids has become an important issue in India. Common problems seen in dermatology practice are steroid-induced and steroid aggravated dermatoses. [36] A recent Indian study by Thomas et al. reported that steroid misuse was a problem of epidemic proportion in rural India and that there was an urgent need to tighten regulatory controls over manufacturing, sale and prescription of irrational topical steroid combinations. [37]
11.8. Topical Antihistamines
- Topical antihistamines are available without a prescription but offer limited benefits in the treatment of pruritic conditions. Overall, studies on topical antihistamines, including topical diphenhydramine, have been inconsistent, inconclusive or limited in design. [34]
11.9. Consensus Opinion
- According to the panel experts, topical corticosteroids exhibit an effective antipruritic effect and are useful for inflammatory dermatoses. However, extensive use might be associated with steroid misuse. Other topical therapies used for pruritus include local anaesthetics, pramoxine, capsaicin, calcineurin inhibitors, menthol, camphor, zinc, doxepin and palmitoyl-ethanol-amine. Capsaicin may cause burning pain due to which patients avoid it. Other topical therapies include urea, glycerol, propylene glycol, lactic acid, potassium permanganate, endocannabinoids, ethyl chloride sprays and topical sodium cromoglycate. Topical antihistamines may cause contact dermatitis/sensitization.
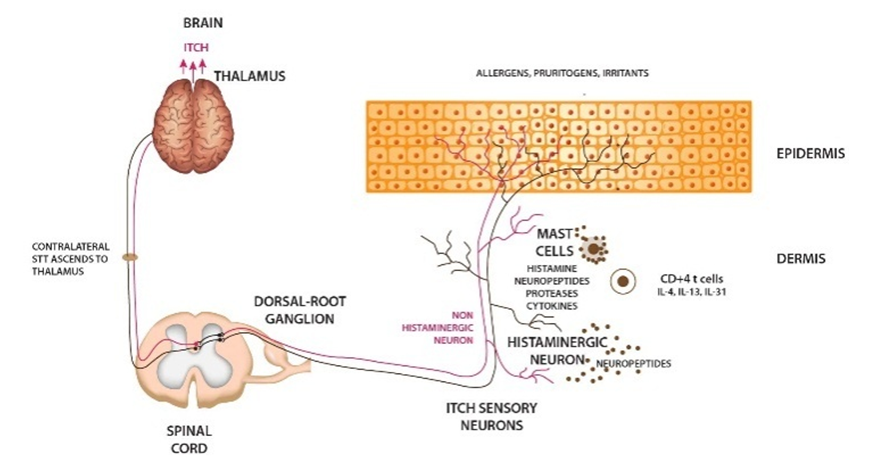
12. Systemic Therapies for Pruritus
12.1. Oral H1 Antihistamines
- First-generation antihistamines bind to both central and peripheral histamine-1 receptors, whereas second-generation antihistamines selectively bind to peripheral histamine-1 receptors. This results in different therapeutic and side effect profiles. [38] Oral H1 antihistamines like hydroxyzine and diphenhydramine are generally the first line of treatment for generalized pruritus. [2] In conditions like atopic dermatitis, hydroxyzine and cetirizine show an ameliorative effect by producing essential sedation and pruritus relief. [39]Hydroxyzine is widely used for symptomatic relief of pruritus. [40] A recent real-world Indian study conducted by Thomas et al. established that hydroxyzine significantly improved symptoms of pruritus and quality of life in patients with chronic pruritus due to dermatological causes over 12 weeks. [40] The European guidelines on chronic pruritus recommends use of hydroxyzine as a first choice in treatment of pruritus occurring as a result of several aetiologies due to its antipruritic, anxiolytic and sedative properties. [33] Also, higher concentrations of hydroxyzine are found in the skin compared to plasma. [41] Second generation antihistamines like cetirizine, levocetirizine and fexofenadine are also often employed to combat pruritus. [33] Evidence reports that up-dosing these antihistamines significantly reduce pruritus. [42]
12.2. Anticonvulsants
- Gabapentin and pregabalin are agonists of g-amino butyric acid that effectively reduce pruritus probably via their role in neural modulation. These drugs aid in treating neuropathic itch, uremic itch, and prurigo nodularis. [30] Gabapentin is also used for treating generalized pruritus of unknown origin that is unresponsive to usual therapy modalities. [43]
12.3. Cyclosporine
- Cyclosporine A is an effective immunosuppressant used for treatment of pruritus in AD and certain autoimmune diseases. Successful treatment of prurigo nodularis of different origins has been reported in 16 patients with an efficacy of 92% and side effect profile of 50%. It may also be effective in lichen planus or drug-induced pruritus. [44]
12.4. Selective Serotonin-Reuptake Inhibitors and Serotonin-Norepinephrine Reuptake Inhibitors
- Selective serotonin reuptake inhibitors (SSRIs) have been used to treat pruritus in patients with prurigo, AD, psychogenic pruritus, paraneoplastic pruritus, and polycythaemia vera. Effectiveness has been reported with paroxetine, fluvoxamine, and sertraline. Serotonin-norepinephrine reuptake inhibitors (SNRIs) were developed later than SSRIs. Venlafaxine has been used at doses between 150 and 300 mg/d. [44]
12.5. Aprepitant
- Aprepitant is a promising NKR1 antagonist for treatment of chronic pruritus, and may be used as a second-line option in refractory cases. [33]
12.6. Antidepressants
- Mirtazapine and specifically doxepin have proved to be effective for pruritus related to urticaria, AD and HIV. [33] Low-dose doxepin is also useful in renal pruritus and various pruritic non-inflammatory dermatoses. [44]
12.7. Opioid Modulators
- μ-opioid receptor (MOR) antagonists like naltrexone and naloxone, have been proven to reduce pruritus secondary to cholestasis, AD, and uremic pruritus. However, use is limited by cost and adverse effects like hepatotoxicity, insomnia, and fatigue. [30]
12.8. Thalidomide
- Thalidomide has reported to be effective in managing prurigo nodularis and pruritus associated with HIV infection. [1]
12.9. Ursodeoxycholic Acid
- Evidence suggests that ursodeoxycholic acid could be used for relieving pruritus from intrahepatic cholestasis of pregnancy. [2]
12.10. Cholestyramine
- Cholestyramine is an acknowledged therapeutic option in hepatic and cholestatic pruritus. [33]
12.11. Serotonin Receptor Antagonists
- Due to pathophysiological significance of serotonin in kidney and liver diseases, serotonin receptor antagonists like ondansetron and granisetron have been used anecdotally to treat pruritus. [25]
12.12. Activated Charcoal
- Activated charcoal is used for treatment of CKD-associated pruritus. [25]
12.13. UV Phototherapy
- Narrowband UVB (311–313 nm) and UVA1 (340–400 nm) are effective in managing AD and associated pruritus. UVB may be effective in managing pruritus associated with end-stage kidney disease, cholestasis, chronic urticaria, prurigo, cutaneous T-cell lymphoma, aquagenic itch, and scleroderma. Phototherapy must be combined with standard first-line therapies. [45]
12.14. Consensus Opinion
- According to the panel experts, oral antihistamines like hydroxyzine, cetirizine and levocetirizine are highly effective and are first line of treatment for pruritus. Up-dosing of antihistamines is effective against pruritus. Modern antihistamines like bilastine and fexofenadine work at higher doses against pruritus. The other systemic therapies include gabapentin and pregabalin, tricyclic antidepressants, doxepin, mirtazapine, naltrexone and cyclosporine. Gabapentin is effective for treatment of neuropathic itch, uremic pruritus and hepatobiliary pruritus. Narrowband UVB is an effective option for relieving pruritus associated with AD. Aprepitant has demonstrated effectiveness in relieving pruritus but is quite expensive. Serlopitant is preferred over aprepitant due to toxicity issues. The panel experts have formulated algorithms for management of acute and chronic pruritus in clinical practice (Figures 3 and 4*).
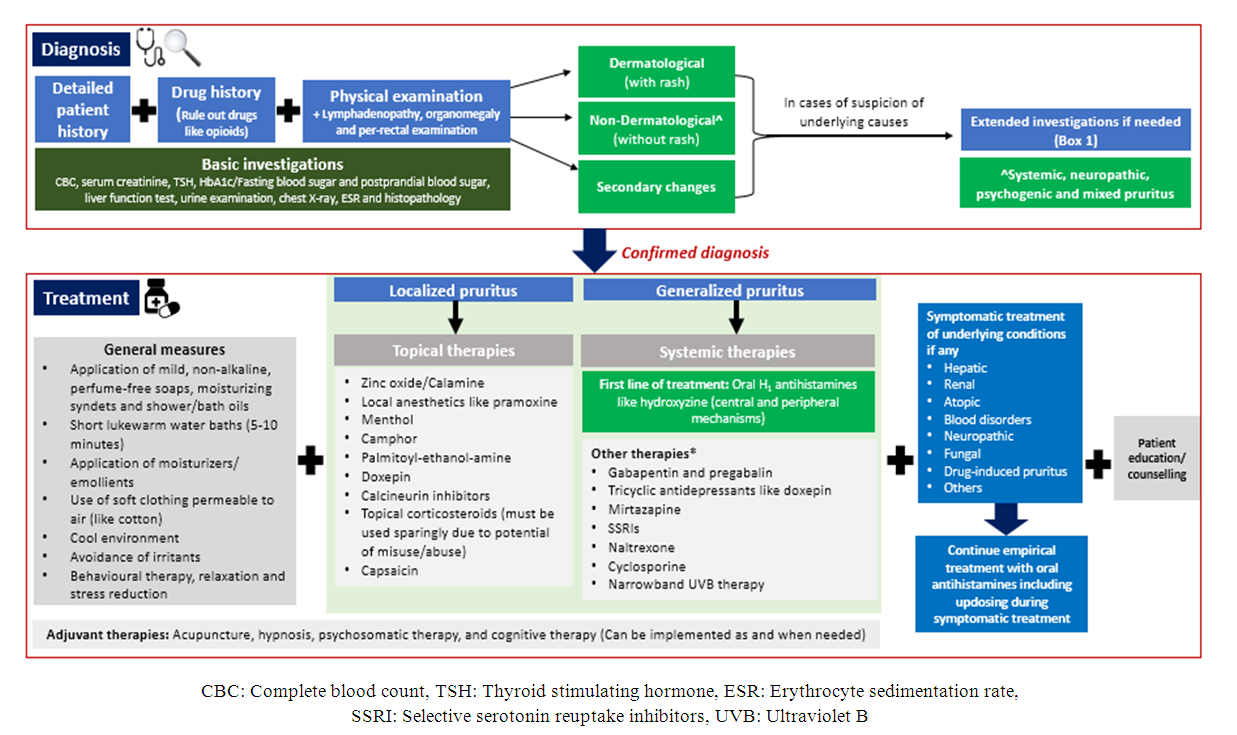 | Figure 3. Management algorithm for chronic pruritus |
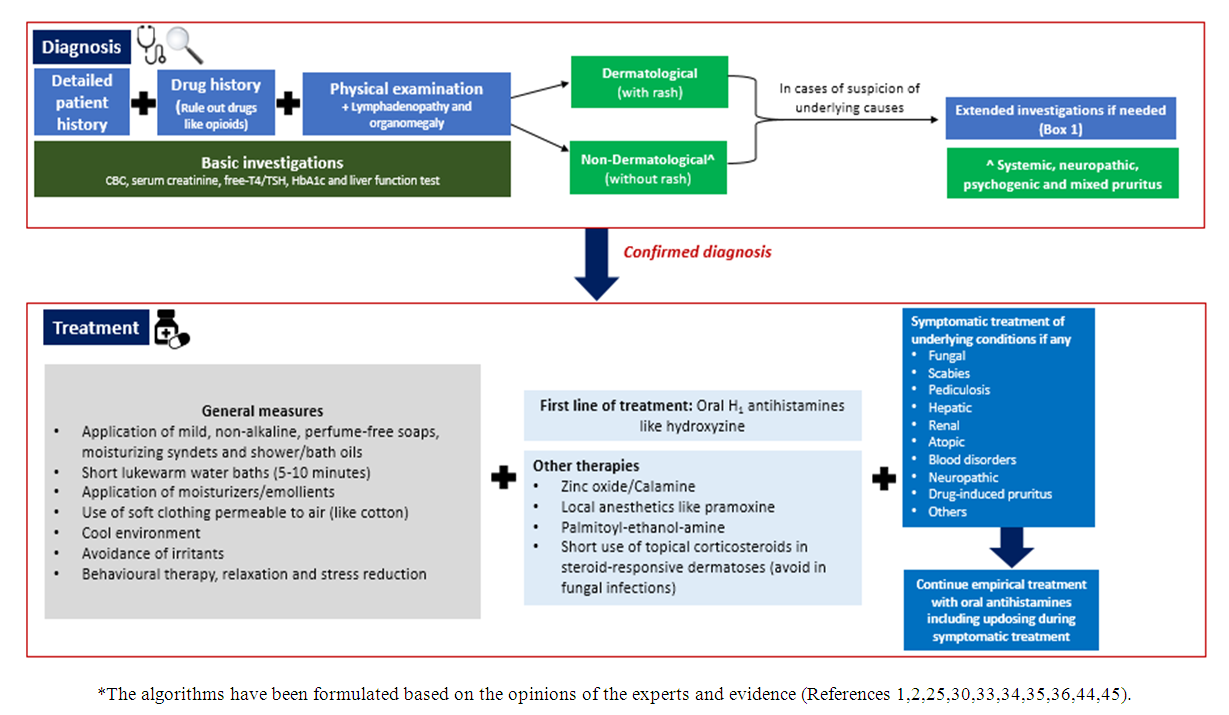 | Figure 4. Management algorithm for acute pruritus |
|
|
13. Role of Adjuvant Therapies and Patient Awareness
- To avoid scratching, behavioural therapy including distraction or alternative scratching techniques like habit reversal could be considered. In patients with pruritus and coexisting depression, psychotherapy combined with psychotropic medication could help. [33] Acupuncture and hypnosis might also have a role in treatment of pruritus. [44] Moreover, a transcutaneous electrical nerve stimulation (TENS) unit is an inexpensive and accessible therapeutic device which is beneficial for relieving chronic pruritus. [46] Lastly, patient education regarding skin hydration, avoidance of triggers and relief measures helps in coping with the vicious circle of itch–scratch–itch. [15,33]
13.1. Consensus Opinion
- Adjuvant therapies like acupuncture, hypnosis, psychosomatic therapy, yoga and cognitive therapy might have a role in treatment of pruritus but there is lack of adequate evidence. Internet-based behavioural therapy and TENS have been proved to be useful in managing pruritus. Patient education plays an important role in management of pruritus. Educational training programs are imperative for dealing with the itch-scratch-itch cycle. The panel experts have formulated a patient education leaflet which could be beneficial for dermatologists and their patients (supplement 1).
14. Conclusions
- Pruritus is commonly seen in routine clinical practice of clinical different specialities, and is associated with various skin, systemic and psychogenic causes. It has a significant impact on an individual’s quality of life. Dominant causes in India include xerosis, eczema, dermatophytosis etc. A thorough patient history, physical examination and basic investigations enable the dermatologist to identify possible causes of pruritus. A combination of general care measures and appropriate topical/systemic therapies could help in symptomatic improvement of pruritus. Oral antihistamines like hydroxyzine are the first-line treatment of pruritus.
ACKNOWLEDGEMENTS
- We would like to acknowledge Scientimed Solutions Pvt. Ltd. for assistance in developing the manuscript.
Conflict of Interest
- There is no conflict of interest among the authors.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML