-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Dermatology and Venereology
p-ISSN: 2332-8479 e-ISSN: 2332-8487
2021; 10(2): 25-29
doi:10.5923/j.ajdv.20211002.02
Received: Nov. 10, 2021; Accepted: Dec. 6, 2021; Published: Dec. 24, 2021

A Comparative Study of Surgical Excision Versus Curettage and Cautery in the Treatment of Basal Cell Carcinoma Regarding Aesthetic Outcome, Complication and Recurrence
Hayder RM Al-Hamamy1, Fatima J. Rahmatullah2
1Iraqi Board for Medical Specialization, Baghdad, Iraq
2Dermatology Clinic, Alfurat Alawsat Teaching Hospital, Najaf, Iraq
Correspondence to: Fatima J. Rahmatullah, Dermatology Clinic, Alfurat Alawsat Teaching Hospital, Najaf, Iraq.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

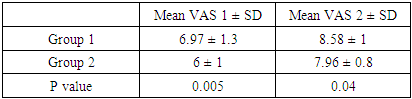
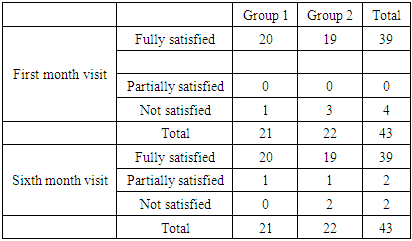
Background: Basal cell carcinoma (BCC) is the most common skin malignancy. If left untreated, it may cause local destruction and disfigurement, so early treatment is important. The treatment method should be chosen carefully to reach effective cancer clearance with best aesthetic result. Objectives: To compare two common methods of treatment of basal cell carcinoma, surgical excision versus curettage and cautery regarding aesthetic outcome, complications and recurrence. Patients and methods: This is an open labeled prospective comparative therapeutic study which has been conducted at the Department of Dermatology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq, from March 2014 to February 2018. A total of 37 patients with 43 BCC were enrolled. They were allocated into two groups; the 1st group was treated with surgical excision (20 patients with 21 BCC) while the 2nd group was treated by curettage and electrodessication (17 patients with 22 BCC). Aesthetic result was assessed for each patient at one and six months after treatment, photographs were taken and patient satisfaction was recorded. Visual analogue scale was measured by assessing the photographs of the 1st month and 6th months by 1 surgeon and 3 dermatologists. The mean result of the 1st group and the 2nd group were compared. Each patient was followed for 2 years to detect any recurrence. Results: according to visual analogue scale, the results of group 1 (surgical excision) was significantly better at one (p value =0.005) and six months (p value =0.04) while difference in patient satisfaction was not significant. Few minor complications were noted which cleared in a short time. Regarding recurrence, one BCC in each group recurred and both were in the same patient. Conclusion: Surgical excision is a simple and effective treatment modality for treatment of BCC with better aesthetic results. Recurrence may relate to individual factors if technical factors are optimum in both methods of treatment.
Keywords: BCC, Surgical excision, Cautery, Electrodessication, Curettage, Aesthetic, Recurrence
Cite this paper: Hayder RM Al-Hamamy, Fatima J. Rahmatullah, A Comparative Study of Surgical Excision Versus Curettage and Cautery in the Treatment of Basal Cell Carcinoma Regarding Aesthetic Outcome, Complication and Recurrence, American Journal of Dermatology and Venereology, Vol. 10 No. 2, 2021, pp. 25-29. doi: 10.5923/j.ajdv.20211002.02.
1. Introduction
- BCC is the most common cancer worldwide, and its incidence appears to be increasing especially in countries where fair skin is the predominant type. As BCC begins to develop in younger patients, the cosmetic outcome of treatment is gaining increasing importance [1]. However, accomplishing cure and preserving function are the most important aspects in treating BCC. The available treatments for BCC can be divided into surgical and nonsurgical techniques, with surgical techniques subdivided into two categories; excision and destruction [2]. MOH micrographic surgery is considered the best option in high risk or cosmetically important areas [3]. Surgical excision with a safe margin is considered by many as the gold standard of treatment [2]. The defect is closed directly or a graft or flap is designed if primary closure is not feasible. Electrocautery and curettage is widely used by dermatologist and the defect is left to heal with primary intension [4].The important aspects the surgeon must consider is the final cosmetic result, recurrence rate in addition to the feasibility and availability of the procedure considering the large number of BCC he has to treat.
2. Patients and Methods
- A total of 37 patients with 43 BCC were enrolled in this open labeled prospective comparative therapeutic study which has been conducted at Department of Dermatology, Baghdad Teaching Hospital, Medical City, Baghdad, Iraq, from March 2014 to February 2018.Inclusion criteria: Primary BCC less than 20 mm in diameter.Exclusion criteria: Location on the eyelids and tip or ala of the nose.The lesions were allocated into 2 groups:Group 1: A total of 20 patients with 21 BCC were treated by surgical excision. The defect was repaired either with direct closure or a flap when direct closure was not possible.Group 2: A total of 17 patients with 22 BCC were treated by curettage and electrocautery.Each patient was informed that he/she has skin cancer and treatment is mandatory. Informed consent was granted by the patient. Detailed history, clinical examination and photography were done before surgery. The diameter and surface area of the lesions were measured by drawing the outline on a transparent paper and measured on a scaled paper.ProcedurePreparation: The safe margin and the planned incision line were drawn on the skin then the skin was sterilized with povidone iodine. Local anesthesia in the form of lidocaine 2% with adrenaline 1/100000 was used except in patients who had any contraindication in whom lidocaine 2% alone was used.Group 1: An elliptical incision was done including a safe margin of 4mm, with number 15 blade. Specimen was sent for histopathological examination in 10% formaldehyde solution. Perfect hemostasis and undermining was achieved before closure. Deep dermal stitches were placed, approximating the wound edges and improving the overall cosmetic result by decreasing the tension on the superficial skin sutures. In 18 lesions the defect was closed directly while three lesions a skin flap was needed; 2 were on the cheek and were closed with rhombic flap while the third lesion was located on the right nasofacial area and was closed by island pedicle flap. Topical antibiotics were used for all patients in this group in the form of clindamycin solution twice daily; starting from day of surgery. In addition, systemic antibiotics were prescribed for diabetic patients and patients with flap surgery. Suture removal was done for all the patients with facial lesions on the 6th day and trunk lesions on the 8th day.Group 2: Shave biopsy was done and the specimen was sent for histopathological examination in 10% formaldehyde. The remaining part of the tumor was removed by a curette followed by electrodessication, another 2 cycles of curettage and electrodessication in radial direction to reach the margin marking and in depth were done. Topical antibiotics (fucidic acid ointment) were prescribed to all patients starting from the day of surgery. In addition, oral antibiotics were prescribed for diabetic patients only.EvaluationThe aesthetic result and patient satisfaction were assessed for each patient one month and six months after surgery. The aesthetic results were evaluated by visual analogue scale by one surgeon and 3 dermatologists other than the researchers.The visual analogue scale (VAS) is calculated as such; each observer was asked to rate the cosmetic result on a scale from 1 to 10, where 10 is the best cosmetic result and 1 is the worst. The range, mean and standard deviation of the value given by the 4 observers were calculated. The values of the 2 groups were compared.Patient's satisfaction was measured by asking the patient at each visit whether he or she was satisfied, partially satisfied, or not satisfied.Recurrence: each patient was followed by serial visit at 1, 6, 12 and 24 months to detect recurrence.
3. Results
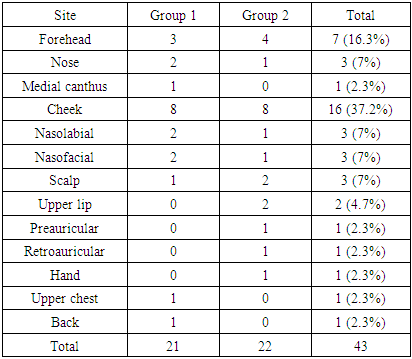
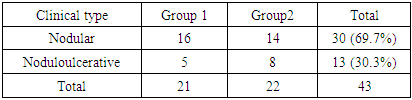
- A total of 37 patients with 43 BCC enrolled in the study, 24 patients (64.86%) were males and 13 patients (35.13%) were females with male to female ratio 1.8:1. Their ages ranged from 34-88 years with a mean and SD = (64± 15.01) years. The duration of the lesions ranged from 0.15-37 years with mean and SD= (3.85 ± 6.76) years. The diameter of the lesions ranged from 2–17.5 mm with mean and SD= (9.95 ± 3.58) mm. The surface area ranged from 3-181 mm2 with mean and SD= (70.2± 46.77) mm2. The sites of the lesions are shown in table 1. The clinical types are shown in table 2.
|
|
|
|
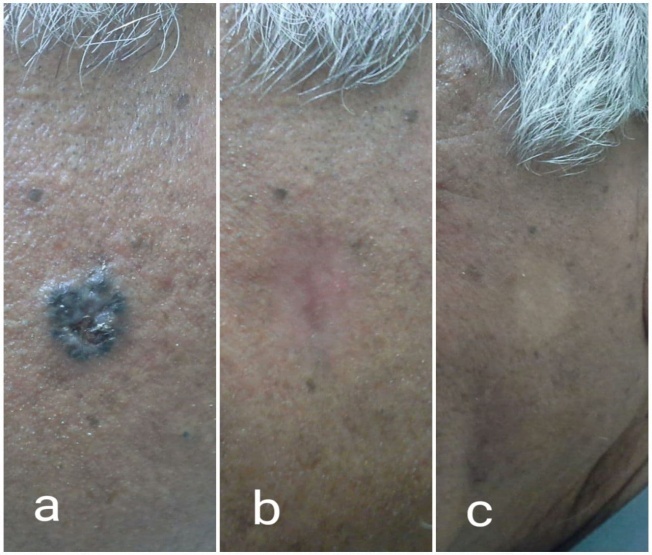 | Figure 1. a) BCC on the right cheek treated by curettage and cautery. b) after 1 month and c. after 6 months |
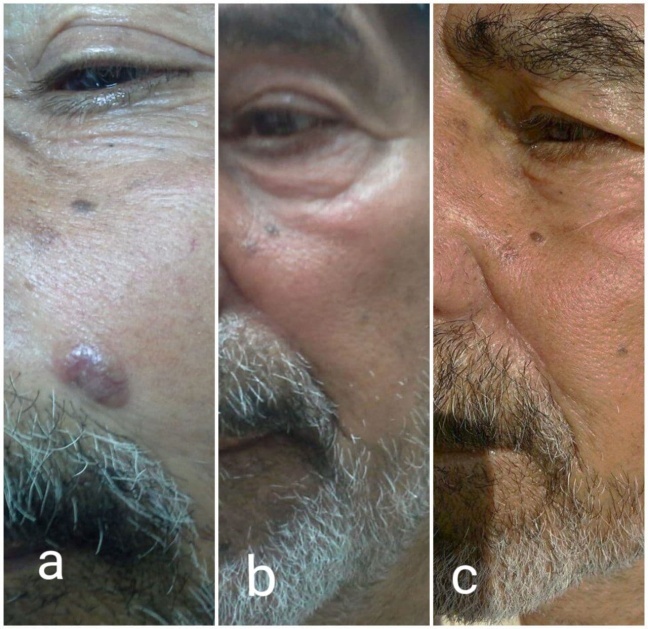 | Figure 2. a) BCC on left nasolabial fold treated by surgical excision b) after 1 month and c) after 6 months |
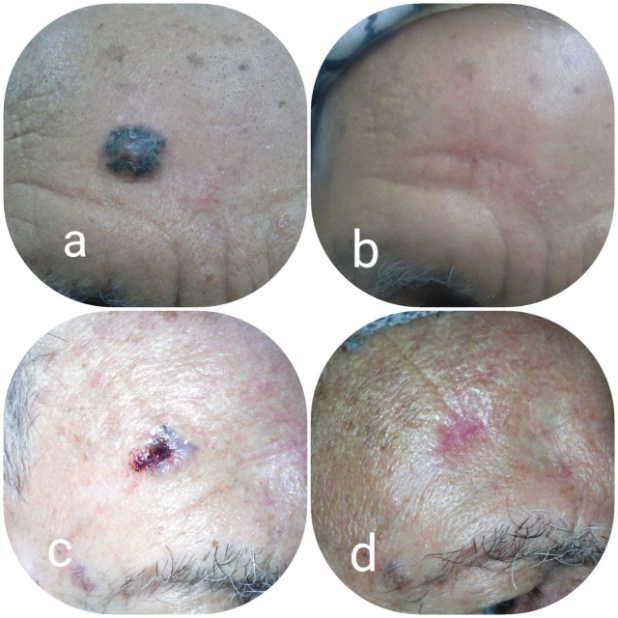 | Figure 3. a) before and b) 1 month after surgical excision. c) before and d) 1 month after curettage and cautery |
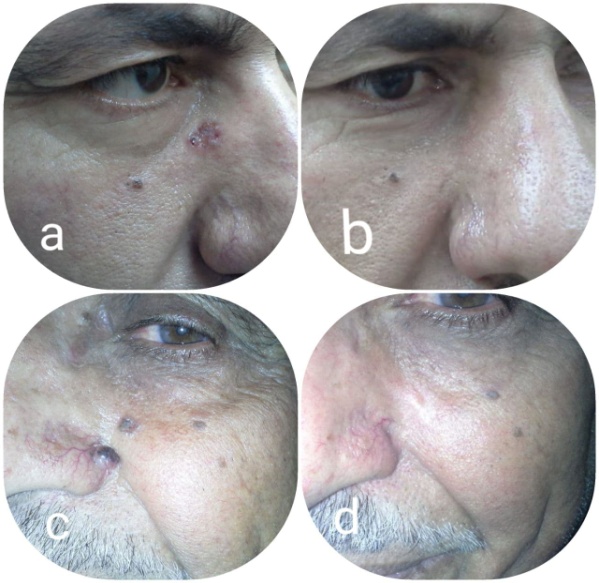 | Figure 4. a) before and b) 6 months after surgical excision. c) before and d) 6 months after curettage and cautery |
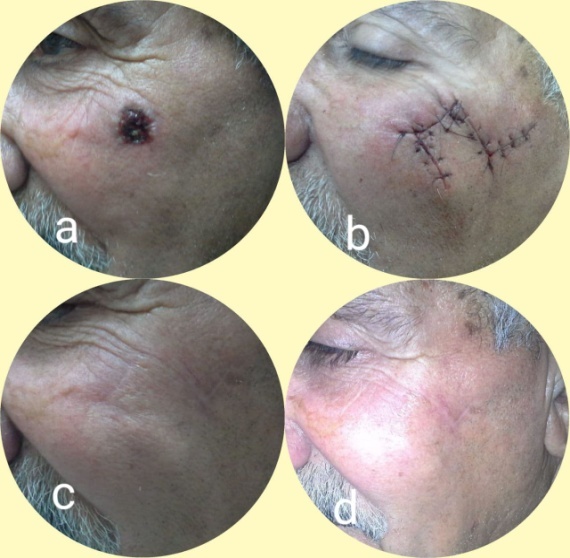 | Figure 5. a) BCC on left cheek removed by surgical excision and wound closed using rhomboid flap. b) after surgery c.) after 1 month and d) after 6 months |
4. Discussion
- Many treatment modalities are employed for the treatment of BCC with various efficacies; and each one has its advantages and disadvantages. These include Moh’s surgery, classic surgical excision, destructive techniques, topical treatments and radiotherapy. There are few randomized controlled studies comparing different skin cancer treatments, and much of the published literature on the treatment of BCC consists of open studies, some with low patient numbers and relatively short follow-up periods [2].Recurrence rate is variable in different studies and highly affected by the treatment type and operator experience. Lowest recurrence rates were obtained by Moh’s surgery, however, it is not popular yet despite its effectiveness as it is costly and time consuming. Surgical excision remains the gold standard for treatment of BCC because a safe margin can be ascertained histopathologically and is associated with better wound healing and the lowest relapse rate [1]. However, many dermatologists prefer curettage and cautery because they think that surgical excision is a difficult procedure, needs experience and is time consuming. In addition, they feel that they are not very competent with flaps and grafts which might be needed to close the defects.Curettage and electrodessication, although a fast and cost effective technique for superficial lesions, doesn’t allow histological margin assessment. Overall 5-year cure rates reported for BCC were 91% to 97% [5,6]. However, recurrence rates can be high for high risk locations (21%) and high risk histological subtypes (27%) [7,8,9]. This technique should not be used to treat areas with terminal hair growth such as the scalp or beard area in males due to risk that a tumor extending down follicular structures may not be adequately removed. If subcutaneous layer is reached during the course of surgery, then surgical excision should generally be performed instead [1].In a survey of 166 U.K. consultant dermatologists in 1995, 24% of 1597 lesions presenting for the first time were treated by curettage and cautery, making it the second most common form of treatment after surgical excision (58%) [10].In a study of 69 curettage and electrodessication wounds that were immediately re-excised using Moh’s surgery, residual tumor was found in 33% of cases overall, with striking differences seen in different body sites (47% of head and neck sites and 8.3% of trunk and limb sites contained residual BCC) [11].In the present only 3 BCC needed flaps after excision while the defect was closed by direct closure in 18 lesions. The flaps were not difficult to perform and they closed the defect properly. Regarding the aesthetic result, surgical excision was superior to curettage and electrodessication as the VAS was significantly higher after one month and six months of treatment. The great majority of patients were satisfied whether they were treated with surgery or curettage and electrodessication because they were happy with getting rid of the cancer. Being of old age, they paid little attention to the aesthetic result. A number of studies compared surgery with other forms of treatment of BCC for example Avrilm et al (1997) found surgery better than radiotherapy [12], Thissen et al (2000) found surgery superior to cryotherapy [13]. While Essers et al (2007) found no difference regarding cosmetic results comparing surgery versus Moh’s surgery [14]. Regarding recurrence, 24 patients with 26 lesion completed the study follow up period for 2 years (13 in group 1 and 11 in group 2) only one of them has recurrence in 2 lesion (the same patient had 2 recurrent lesions) one in the scalp which was treated by surgical excision and the other lesion was on the mustache which was treated by curettage and cautery. Histopathology of the 2 recurrent lesions was of adenoid subtype and as we know it is of low risk potential. So the recurrence in such characteristics may indicate individual and personal factors causing the recurrence. Other factor that may contribute to that recurrence is the location of both lesions in terminal hair bearing areas causing the malignant cells to migrate deeply along the hair follicles leading to this unexpected recurrence.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML